Oncology and Cancer Screening
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2994-8746 | Journal DOI: 10.61148/2994-8746/JOCS
Rajiv Kumar
Faculty of Sciences, University of Delhi, Delhi. 110007, India.
Corresponding author: Rajiv Kumar, Faculty of Sciences, University of Delhi, Delhi. 110007, India.
Received: March 05, 2025 Accepted: March 25, 2025 Published: April 12, 2025
Citation: Rajiv Kumar. (2025) “Cancer: Pathology Of Inflammation And Therapeutic Targets”, J Oncology and Cancer Screening, 6(1); DOI: DOI: 10.61148/2994-8746/JOCS/70
Copyright: © 2025 Rajiv Kumar. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Inflammation induces acute and/or chronic inflammatory reactions in various organs, including the heart, lung, brain, pancreas, liver, kidney, intestinal system, and reproductive system, theoretically leading to tissue damage or disease and therefore it is a critical component of tumour progression
Inflammation induces acute
Editorial
Inflammation induces acute and/or chronic inflammatory reactions in various organs, including the heart, lung, brain, pancreas, liver, kidney, intestinal system, and reproductive system, theoretically leading to tissue damage or disease and therefore it is a critical component of tumour progression.1 In the presence of infectious and non-infectious agents, the rate of inflammatory reactions increased, which triggered inflammatory signaling pathways, including NF-κB, JAK-STAT, and MAPK.2 Chronic inflammation and the allied underlying molecular mechanisms triggering cellular events that promote the malignant transformation of normal cells in the gastrointestinal tract to cancer. The etiology of inflammation, inflammatory responses, organ-specific inflammatory responses and mechanisms underlying are crucial points that should be explored to investigate the correlation between pathology of cancer and inflammation.3 Pathological conditions of inflammation, such as intrinsic, are responsible for neoplasia, and extrinsic promote cancer and have a deep association with inflammation and cancer. Both extrinsic and intrinsic inflammation induce immunosuppression that further promotes tumor development. Such a relationship between chronic inflammation and carcinogenesis illustrated by the interpretation of specific cancers and mechanisms underlying. Intrinsic and extrinsic pathways triggered NF-κB, HIF-1, and STAT-3 and upkeep tumorigenic factors in the tumour microenvironment at multiple levels. NF-κB is a mediator of the immune response and its phosphorylation initiates translocation of NF-κB protein to the nucleus.4 Furthermore, NF-κB governed the transcription of pro-inflammatory cytokines and chemokines. These alterations promote tumor-associated inflammation and, inhibiting anti-tumor immune responses. These unwanted transformations and alterations promote metastatic spread and progression, as well as tumor growth. However, mediators such as IL-1, IL-6, TNF, and PGHS-2 existed in the cellular environment that can alter aforesaid promoting factors.5 Overexpression of the IL-1 agonists IL-1α and IL-1β promotes tumor invasiveness and metastasis by altering angiogenic genes and growth factors.
Besides autoimmune diseases, obesity, bacterial and viral infections, tobacco, excessive alcohol consumption, smoking, and asbestos exposure also initiate tumor-extrinsic inflammation and further increase cancer risk and stimulate malignant progression.6 Thus, infection, chronic irritation, and inflammation initiate and promote carcinogenesis, cause DNA damage, and trigger cytokines and promote growth factors. Besides, the persistent inflammation in the tumour microenvironment enhanced various events, including angiogenesis, metastasis, response to hormones, chemotherapeutic agents proliferation, survival of malignant cells, and subversion of adaptive immunity.7 Pathologic conditions such as gastroesophageal reflux, cholelithiasis, inflammatory bowel disease, chronic cholecystitis and the existence of microbial agents initiate and propagate obstructive or diffuse interstitial lung disease.8 Chronic inflammation consists of several cascades of cellular and humoral factors and can initiate an inflammatory response, which contributes to the pathogenesis of various cancers.
Cancer-initiating mutations also promote cancer-elicited inflammation and instigated malignant progression via inflammatory cells.9 Besides, inflammatory cytokines promote cellular events that propagate malignancy and carcinogenesis.10 Inflammatory cytokines initiate heart failure, coronary artery disease, myocardial infarction, and other adverse cardiac events as well as inductee several inflammatory cascades that propagates the atherosclerotic process. Several other aspects of atherogenesis are accelerated by cytokines. Many cytokines such as interleukin-1, macrophage migration inhibitory factor, interleukin-6, interleukin-10, tumor necrosis factor-α, and transforming growth factor-β are involved in tumorigenesis and cancer pathogenesis. Cytokines also initiate the pathogenesis of cardiovascular disease and cancer.11,12 Inflammatory metabolites including prostaglandins, leukotrienes, thromboxane, and specialized pro-resolving mediators regulate the phenomenon of initiation and resolution of inflammation.
Newly developed therapeutics such as local irradiation, recombinant, small-molecule inhibitors, oncolytic viruses, cytokines, neutralizing antibodies, and TLR agonists can alter inflammation and be applied as a therapeutic for cancer, and as per the results obtained from the undergoing clinical trials13, it can be a reality.14 Therefore, a few cellular events, such as the route of initiation and resolution of inflammation, the phenomenon of the crosstalk between tumor development and inflammatory processes can be the potential targets for hunting inflammation during cancer. Nanotherapeutics can target mediators responsible for metabolism and immune system responses for dealing with the convergence of intracellular mechanisms of inflammation, metabolic transformation, and cancer progression.15
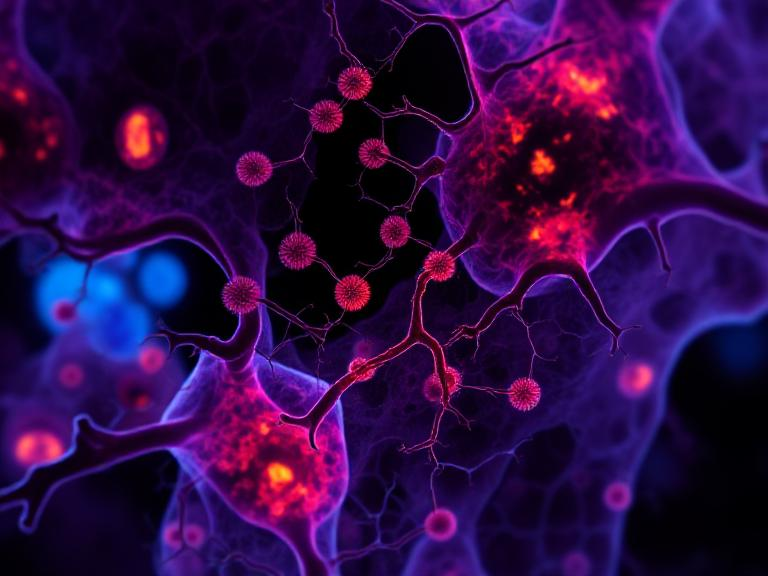
Figure 01. An illustration of the pathology of cancer, related inflammation, and therapeutic targets.
Acknowledgements
One of the authors, Rajiv Kumar, gratefully acknowledges his younger brother, Bitto.
Consent for publication
Not Applicable.
Funding
This research received no particular grant from any funding agency in the public, private, or not-for-profit sectors.
Conflict of interest
The authors declare no conflict of interest, financial or otherwise.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Data availability statement
Due to the nature of the research, [ethical, legal/commercial] supporting data is not applicable and thus not available.