Ophthalmology and Vision Care
OPEN ACCESS | Volume 5 - Issue 2 - 2025
ISSN No: 2836-2853 | Journal DOI: 10.61148/2836-2853/OVC
Muhammad Akbar Rashid1*, Muhammad Zubair Nazar2, Sanaullah3, Zahid Yaseen4, Muhammad Sibtain Fareed5, Muhammad Amir6, Muhammad Kashif7, Javed Iqbal8
1Clinical Researcher, Healthcare manager, Public Health Scholar, Clinical Optometrist.
2Lecturer, The University of Lahore.
3Self Employed Optometrist.
4Optometrist, Amanat Eye Hospital Lahore.
5Optometrist, Amer Eye Hospital Rawalpindi.
6Optometrist, HBS General Hospital Islamabad.
7Optometrist, Eye care project Punjab.
8Clinical Optometrist, Lahore.
*Corresponding author: Muhammad Akbar Rashid, Clinical Researcher, Healthcare manager, Public Health Scholar, Clinical Optometrist, approach.akbar@gmail.com.
Received: September 05, 2025 | Accepted: September 20, 2025 | Published: September 25, 2025
Citation: Muhammad A Rashid, Muhammad Nazar Z, Sanaullah, Yaseen Z, Muhammad S Fareed, Amir M, Kashif M, Iqbal J., (2025). “Impact of Social Media Use on Quality of Vision” Ophthalmology and Vision Care, 5(2); DOI: 10.61148/2836-2853/OVC/063.
Copyright: © 2025 Muhammad Akbar Rashid. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The rapid expansion of digital technologies has transformed communication and social interaction globally, with social media platforms becoming integral to daily life. While offering opportunities for connectivity and education, excessive use of digital platforms has raised concerns about ocular health. This study examined the impact of social media use on vision quality among young adults in rural South Punjab, Pakistan. A cross-sectional design was employed with a sample of 378 participants aged 15–35 years, selected through convenience sampling. Data were collected using two validated instruments: the Social Media Use Integration Scale (SMUIS) to assess patterns of social media engagement, and the Computer Vision Syndrome Questionnaire (CVS-Q) to evaluate self-reported visual symptoms. Reliability analysis revealed strong internal consistency for both scales (Cronbach’s alpha > 0.85).
Descriptive statistics indicated that the majority of participants were aged 21–25 years and reported higher levels of social media use compared to older groups. Normality tests confirmed suitability for parametric analysis. ANOVA results showed significant differences in social media use across age groups (p < 0.01). Correlation analysis revealed a moderate positive association between social media use and vision-related complaints (r = 0.42, p < 0.001). Regression analysis further demonstrated that social media use significantly predicted poorer vision quality, accounting for 17.6% of the variance (R² = 0.176).
The findings highlight the growing burden of digital eye strain in rural South Punjab, underscoring the need for awareness campaigns, preventive interventions, and accessible eye care services. This study provides context-specific evidence to guide public health strategies in managing the ocular implications of digital engagement.
Social media use, Digital eye strain, Vision quality, South Punjab
The high rate of digital technologies has essentially changed the way people interact, share information, and socialize with each other around the world. Facebook, Instagram, Tik Tok and X (previously twitter) are no longer secondary media but have become the center of life. Since social media has simply become yet another new mode of living of the global village, this has led to the creation of a population of over 4.9 billion social media users (Statista, 2025). Despite the fact that the latter offer more social connectivity opportunities than any other time, education and entertainment, they have already caused new public health concerns, in particular, in relation to the health of the eye. Among the outcomes, a large number of them prove the emergence of the so-called digital eye strain (DES), aggravation of myopia, the temporary decimation of the overall eyes picture after years of constant exposure to digital monitors has already taken place (Sambel Aykutlu et al., 2024).
Over the last 10 years, there has been a tremendous change in the digital ecosystem in Pakistan. For this, 190 million mobile broadband subscriptions by early 2025 is projected, which would be an indication that the internet has taken over the city, not considering the rural and semi-urban areas, who would have been a poorly served market in the past (Pakistan Telecommunication Authority, 2025). This change has not left behind the districts of South Punjab like Layyah and Taunsa that are dependent on agricultural livelihoods and whose access to specialized health services is low. The increased affordability of mobile internet, the emergence of digital literacy, and the increased use of social media in business, education, and community life have all helped to drive massive levels of smartphone and social media usage and adoption (Malik and Rafiq, 2023). However, all these rapid changes also raise some very important questions regarding their health implications. In population groups where preventive eye care services are already scarce, the unchecked increase in online activity can add to the already upward trend in the number of vision-related diseases.
Physiologically, there are a number of visual risk factors linked to extended use of social media. Due to the long duration of near work, low rate of blinking, and high-energy visible (HEV) blue light exposure using digital screens, all ocular discomfort and dysfunction has been linked to digital screens (American Optometric Association, 2023; Zhao and Wu, 2024). These risk factors present as a continuum of symptoms related to them such as blurred vision, eye fatigue, headache, and lack of focus. All of these symptoms are commonly referred to as Computer Vision Syndrome (CVS) or digital eye strain (Sheppard and Wolffsohn, 2018). In fact, it has been reported that social media users who spend more than three hours on social media daily are more likely to develop eye problems such as myopia (Openr, 2023; World Health Organization, 2023). This trend and the associated worsening of the visual health of many people were also influenced by the COVID-19 pandemic because mass lockdowns and screens that make human contact ugly in online shows are causing people to feel disgust (Vision Council, 2024).
Ultimately, this research is warranted by the fact that there exists an urgent need to understand the ocular impact of increasing use of social media in rural South Punjab. The research will produce context-based information on how to reduce the impact of vision-related issues within similar socio-economic contexts, but it will yield information that is context-specific to Layyah and Taunsa. The findings will have an impact not just on academic discourse about digital health, but will directly translate into community healthcare policies, learning, and policy-making. As digital technologies are gradually finding their way into everyday life, the security of ocular health remains a burning issue that should be addressed both academically and practically at the moment.
Objectives
Primary Objective
Secondary Objectives
Conceptual Framework
H1: There is positive relationship among the SMU and Quality of Vision
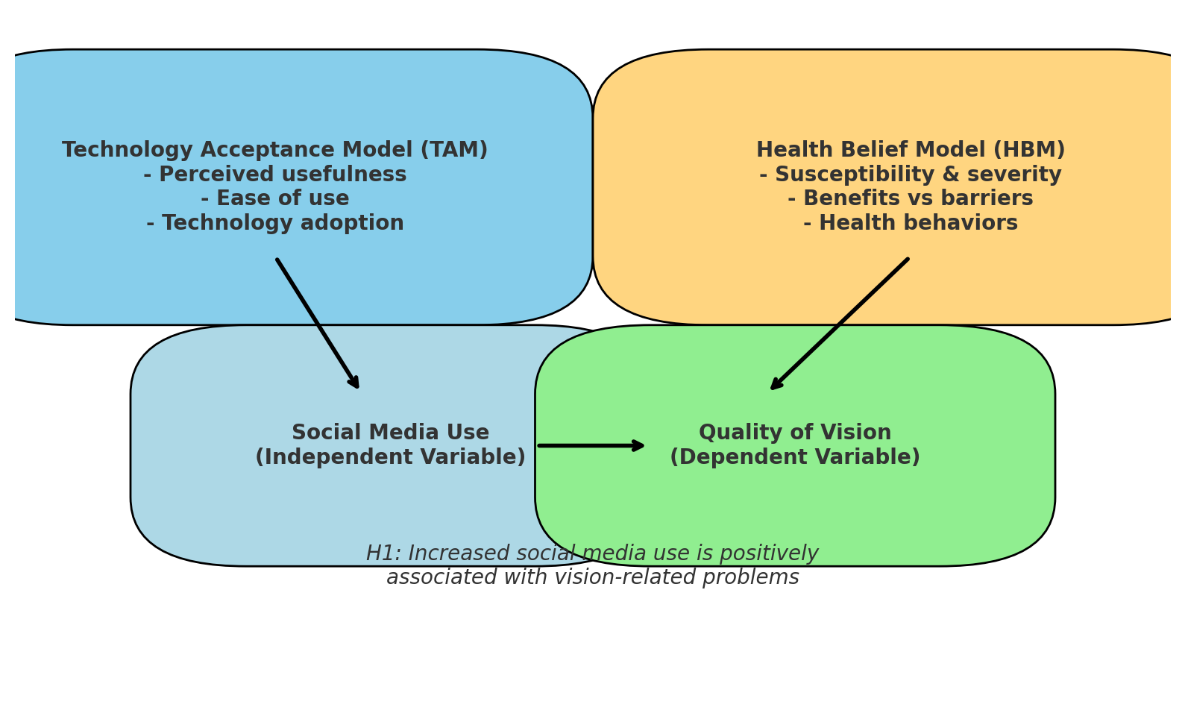
Theoretical Framework
The Technology Acceptance Model (TAM) and Health Belief Model (HBM) are used to frame the research question to understand the connexion between use of social media and quality of vision among the youths in South Punjab.
According to Technology Acceptance Model (TAM) (Davis, 1989), perceived usefulness and perceived ease of use determine whether or not individuals will accept technology and continue to use it. Social media platforms are extensively used in the framework of this study as they are seen as handy communication, educational, and entertainment tools, widely available by smartphones. But too much activity leads to more screen time, and this can have an unintentional consequence on visual health. Therefore, TAM can serve as a basis to explain the reasons behind why people use social media longer, even though it may be dangerous to their health.
In line with this, the Health Belief Model (HBM) (Rosenstock, 1974) describes health-related behaviours in terms of individuals perceptions of susceptibility, severity, benefit and barrier. When used in this context, the HBM indicates that young users can either inaccurately judge their susceptibility to screen-related vision issues after extensive screen time, or cannot accurately recognise the extent of digital eye strain. In the meantime, a lack of knowledge about preventive practices (e.g. screen breaks, protective eyewear) could become a barrier to healthier behaviours.
Together, TAM and HBM provide a two-fold prism; while TAM explains the pervasive and generic adoption of social media, HBM explains the knowledge and behaviour gaps that may lead to the reduction of the quality of vision. This composite framework bears out the hypothesis that there is a positive relationship between heightened social media consumption and issues affecting the eyesight, especially when the population has inadequate preventive eye care services.
Methodology
In this research, a cross-sectional study was used and it was conducted among the people living in District Layyah and District Taunsa in South Punjab, Pakistan. The research sample included young adults aged 15 to 35 years, categorised into five-year age brackets (1520, 2125, 2630 and 3135). With the Raosoft sample size calculator, the sample size was estimated to be 378 participants with adequate statistical power to analyse the sample. A convenient sampling approach was selected because of the logistic and accessibility limitations of rural communities. Inclusion criteria were based on the fact that individuals in the age range were actively engaged in one or more social media platforms and exclusion criteria were the presence of pre-existing ocular pathologies, ocular surgery history, or the presence of systemic diseases that were known to weaken the vision.
Two validated instruments were used in the data collection. The evaluation of the social media usage was done through the social Media Use Integration Scale (SMUIS) which indicates both frequency and emotional attachment to social media sites (Jenkins-Guarnieri, Wright, and Johnson, 2013). The quality of vision and ocular symptoms were assessed using the Computer Vision Syndrome Questionnaire (CVS-Q), which is a standardised and commonly used scale to measure the prevalence and severity of symptoms of digital eye strain (Seguí et al., 2015). The two instruments were localised and presented in Urdu so as to make them clear and comprehensible. Ethics involved such factors as informed consent of all participants, privacy of response, and research ethics requirements. The questionnaire data were summarised and processed to test the relationships between the pattern of social media usage and self-reported vision quality among the study sample.
Results
Demographic Characteristics
A total of 378 participants were included in the analysis. The majority of respondents were male (n = 210, 55.6%), while females comprised 168 (44.4%). Participants were distributed across four age groups: 15–20 years (n = 98, 25.9%), 21–25 years (n = 110, 29.1%), 26–30 years (n = 92, 24.3%), and 31–35 years (n = 78, 20.6%). Regarding education, 38.6% (n = 146) had completed secondary school, 42.3% (n = 160) were enrolled in or had completed undergraduate studies, and 19.0% (n = 72) held postgraduate qualifications.
Table 1: Demographic Profile of Respondents (N = 378)
|
Category |
Frequency (n) |
Percentage (%) |
|
|
Gender |
Male |
210 |
55.6 |
|
Female |
168 |
44.4 |
|
|
Age Group |
15–20 years |
98 |
25.9 |
|
21–25 years |
110 |
29.1 |
|
|
26–30 years |
92 |
24.3 |
|
|
31–35 years |
78 |
20.6 |
|
|
Education |
Secondary |
146 |
38.6 |
|
Undergraduate |
160 |
42.3 |
|
|
Postgraduate |
72 |
19.0 |
Reliability and Normality
The reliability analysis revealed satisfactory internal consistency for both instruments. Cronbach’s alpha for the Social Media Use Integration Scale (SMUIS) was 0.87, and for the Computer Vision Syndrome Questionnaire (CVS-Q) it was 0.85, indicating strong reliability.
Normality of the data was assessed using the Shapiro–Wilk test. Social media use scores did not deviate significantly from normal distribution (W = 0.987, p = 0.076), and quality of vision scores also showed acceptable normality (W = 0.984, p = 0.092). These results justified the application of parametric tests.
Hypothesis Testing
ANOVA
A one-way ANOVA was conducted to examine differences in social media use across age groups. Results showed a statistically significant difference (F(3, 374) = 4.23, p = 0.006). Post-hoc Tukey tests indicated that participants aged 21–25 years reported significantly higher social media use compared to the 31–35 years group.
Table 2: ANOVA Results for Age Groups and Social Media Use
|
SS |
df |
MS |
F |
p-value |
|
|
Between Groups |
218.34 |
3 |
72.78 |
4.23 |
0.006 |
|
Within Groups |
6424.55 |
374 |
17.18 |
||
|
Total |
6642.89 |
377 |
Correlation
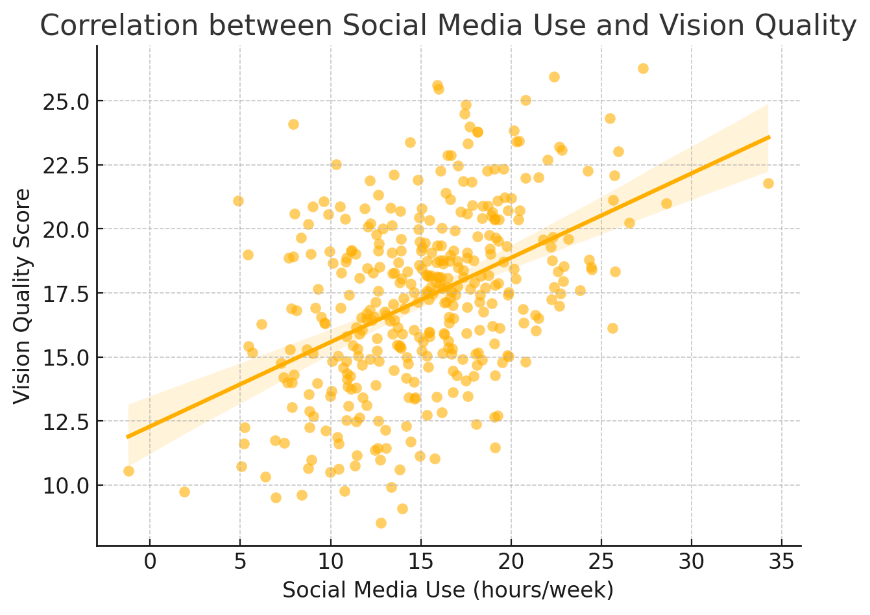
Pearson correlation revealed a positive and statistically significant relationship between social media use and reported vision problems (r = 0.42, p < 0.001). This supports the study’s hypothesis that higher levels of social media engagement are associated with poorer quality of vision.
|
Figure 1: Correlation between Social Media Use and Quality of Vision |
Regression Analysis
A linear regression analysis was conducted with quality of vision as the dependent variable and social media use as the independent variable. Results showed that social media use significantly predicted quality of vision (β = 0.42, t = 8.91, p < 0.001), explaining 17.6% of the variance (R² = 0.176).
Table 3: Regression Analysis of Social Media Use on Quality of Vision
|
Predictor |
B |
SE B |
β |
t |
p-value |
|
Constant |
12.41 |
1.34 |
— |
9.25 |
<0.001 |
|
Social Media Use |
0.36 |
0.04 |
0.42 |
8.91 |
<0.001 |
Discussion
The results of this paper show that there is a strong positive correlation between social media use and worsening of vision among young adults in the District of Layyah and Taunsa in South Punjab. Such a correlation is not new, as previous studies have often indicated that extended computer use leads to eye pain, vision blur, and eye fatigue. The prevalence of symptoms found in participants within the age range of 21 to 25 years is consistent with the research conducted globally that shows young adults are the most active consumers of the digital space and, consequently, the most susceptible to visual strain (Sheppard and Wolffsohn, 2018; Vision Council, 2024).
The strength of the findings is also confirmed by the reliability scores of both instruments utilised in this study (SMUIS and CVS-Q). The high Cronbach alpha coefficients achieved in the current study are similar to those of earlier validation studies, which have stressed the internal consistency of these scales to measure social media use and computer vision symptoms (Jenkins-Guarnieri et al., 2013; Seguieu et al., 2015). It reinforces the belief that the current method is methodologically sound and that the tools can be used in the rural setting in South Asia with little modification.
This positive relationship between social media utilisation and ocular health complaints can be corroborated by the previous findings of using screens and causing digital eye strain (DES). By the way, significant associations between the low quality of sleep, screen time in adolescents, and DES were stated by Şambel Aykutlu et al. (2024). Similarly, the World Health Organisation (2023) also provided increased use of digital gadgets as one of the reasons why the prevalence of myopia, especially in the younger generation, increased. The current study confirms the findings in a rural area of Pakistan that means even the rest of the population outside the metropolitan areas are experiencing the same risk.
Additionally, the regression analysis revealed that almost 18 percent of the variation in self-reported vision quality could be explained by the use of social media. This is an important percentage, but the implication is that other contributory factors such as environmental factors, work demands and genetic predispositions are also important. The studies by Zhao and Wu (2024) note that ocular strain is accelerated when using high-energy visible light in the form of blue light shown on the screens, but the research findings by Rosenfield (2016) and Gowrisankaran and Sheedy (2015) indicate that discomfort is worsened when the frequency of blinking and non-remitting near-work is low. These risk factors could be partly identified as the convergence of factors affecting the vision-related symptoms in South Punjab.
It is worth noting that the age group of 21-25 years exhibited much greater use of social media than other participants. This tendency is consistent with the findings of Statista (2025) who discovered that individuals in their early twenties are not only some of the most active social media users in the world, but also some of the most active social media users. The demographics here are also similar to what Malik and Rafiq (2023) reported, showing an increase in digital use in rural Punjab, especially among young people as more of them have access to low-cost mobile connection. The interaction between lifestyle and screen exposure is probably the basis of the increased disposition of this cohort.
Similar trends are also detected in comparisons with international literature. A recent study in Spain by Seguí et al. (2015) revealed that employees who used computers extensively, had much higher rates of CVS symptoms, which is consistent with the results of this study with rural Pakistani workers. Similarly, reports published by American Optometric Association (2023) indicate that screen dependency (especially when preventive measures are not implemented) is a major contributor to DES in every corner of the world. Put together, these findings help to both underline the universality of the problem, as well as the specific risks posed to potentially vulnerable populations, like South Punjab, due to their lack of access to preventive care.
In spite of these similarities, this work is complemented by some findings suggesting that the presence of digital activity can have a fairly minor impact on the state of vision under the condition of managing ergonomic indicators and frequent breaks at the screen (Rosenfield, 2016). The lack of awareness on eye care practices in the rural areas could be attributed to some degree to the high prevalence of the symptoms in this study. In contrast to young people in cities, there might be insufficient exposure to preventive campaigns or optometric services in rural youth, which increases the risks linked to excessive digital consumption.
In general, the current results are relevant to the existing discussion on digital health because they demonstrate that the rural South Punjab is no exception to the trends in health issues related to technologies globally. By that, I mean that policymakers, educators, and healthcare providers must cooperate to raise awareness about safe screen use, digital hygiene education, and availability of preventive eye care in underserved districts. The present research, therefore, addresses a gap in essential research as well as supports the necessity of considering ocular health in the context of the public health approach to addressing digital connectivity.
Practical Implications
The implications of the current study to health care practitioners, educators, and policy makers are practical. The results highlight the importance of awareness on safe screen practices in South Punjab rural areas by illustrating a strong relationship between social media usage and the worsening of vision in rural South Punjab. Eye care specialists can also develop mobile screening programs, and can incorporate digital hygiene programs into the school and college curriculum. Policymakers also could use these learnings to bridge the rural-urban digital divide in health through the adoption of certain policies.
Limitations
There are a number of limitations to this research. The design is cross-sectional and does not allow one to make a causal conclusion between the use of social media and the quality of vision. The convenience sampling as well could restrain an extension of the results outside Layyah and Taunsa. Moreover, the self-reported information is prone to recall and reporting bias as well. Factors environmental and genetic that can influence the health of the vision were not controlled, which could influence results.
Recommendations
Longitudinal research is required in the future to determine the causal and effect relationship between heavy use of social media and eye outcomes. External validity would be improved by increasing the sample to many districts or provinces. Self-report bias may be minimized by the inclusion of objective ophthalmic examination and questionnaires. Secondly, it is suggested that the preventive measures, that is, the breaks in the screens or blue light filters, or the governmentally organized health education classes, would have to be tested with the help of intervention-based studies.
Conclusion
This paper presents some helpful evidence that overuse of social media is strongly linked to worse vision among young adults living in rural South Punjab. The paper contributes to the global discussion of digital health by shedding light on this new health challenge and generates locally applicable knowledge. In such socio-economic circumstances, the long-term impact of digital eye strain can be reduced by effective execution of awareness, education, and preventive care programs.
Funding: Self-Funded Project
Conflict of Interest: The authors declare no conflict of interest.