Ophthalmology and Vision Care
OPEN ACCESS | Volume 5 - Issue 2 - 2025
ISSN No: 2836-2853 | Journal DOI: 10.61148/2836-2853/OVC
Dr. A. S. M. Moin Uddin1, Dr. Muntakim Shahid4, Dr. Md. Rajeeb Alam3, Dr. Md. Lutfuzzahan5, Mohammad Shamsal Islam5*
1Associate Professor & Senior Consultant, Department of Cornea and Anterior Segment, & Co-Ordinator, Cataract Training Program (CTP), IIEI&H.
2Associate Professor & Senior Consultant, Department of Cornea and Anterior Segment, IIEI&H.
3Senior Consultant, Department of Cornea and Anterior Segment, IIEI&H.
4Consultant, Department of Cornea and Anterior Segment, IIEI&H.
5Epidemiologist, Department of Education, IIEI&H.
*Corresponding author: Mohammad Shamsal Islam, Epidemiologist, Department of Education, IIEI&H.
Received: May 20, 2025
Accepted: June 01, 2025
Published: June 05, 2025
Citation: A. S. M. Moin Uddin, Muntakim Shahid, Md. Rajeeb Alam, Md. Lutfuzzahan, Mohammad S Islam., (2025). “Challenges and Opportunities of Corneal Disease Treatment In Bangladesh: A Systematic Review And Meta-Analysis” Ophthalmology and Vision Care, 5(1); DOI: 10.61148/2836-2853/OVC/062.
Copyright: © 2025 Mohammad Shamsal Islam. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Corneal blindness is an important contributor to visual disability globally and has a greater prevalence in low-income countries like Bangladesh. The causes of corneal blindness include infectious keratitis and ocular trauma, and corneal transplantation is considered a sight-saving procedure. Corneal blindness is preventable and treatable in most cases. We need appropriate information, which is important to understand the challenges and effective interventions to minimize the gap in prevention and treatment. Our article aims to identify the challenges and opportunities, including primordial, primary, and secondary prevention, to address reducing the burden of corneal blindness in Bangladesh. Human resource development and awareness campaigns are usually designed to reduce ocular trauma and infectious keratitis and improve access to primary eye care. Fulfilling the required training for general ophthalmologists in the management of basic corneal surgeries, treating the disease, and access to eye care services in rural & remote areas are the key factors for corneal disease prevention and treatment in Bangladesh. In most cases, corneal transplantation facilities and complicated treatment are tertiary centered. The scarcity of trained cornea doctors, the lack of donor corneal tissue, poor eye banking services, and poor awareness about the collection of human corneas are the challenging factors in ensuring corneal-related treatment in Bangladesh. 3D-printed corneas, cultured stem cells, and biomaterials may be the alternative approach for us. Collaborative efforts from eye healthcare professionals, policymakers, and civil society are required to design and implement the appropriate prevention strategies aiming to reduce the prevalence of corneal blindness in Bangladesh.
Corneal disease, infectious keratitis, ocular trauma, IIEI&H
Introduction:
A corneal ulcer is considered 4th leading cause of blindness globally, and around 5.1% of people worldwide suffer from corneal ulcer-related diseases. Ocular trauma and ulcerations contribute about 1.5 to 2 million new cases every year globally. Quack treatment and traditional medicine play a vital role as major risk factors in the epidemic of corneal ulceration in developing countries as well. Recent statistics suggest that about 350000 children are born with or develop infections at the teenage age, which ultimately leads to corneal blindness1. Such young-age corneal disease may lead to cataracts and glaucoma in rural poor communities if there is not enough treatment for eye injuries and some communicable diseases2. Some risk factors include infections and nutritional, inflammatory, inherited, and degenerative conditions that may lead to visual impairment and blindness. In developing countries, the corneal disease rate is tenfold higher compared to developed countries. The reasons for the higher prevalence of corneal disease in developing countries include variations in climate, geographical location, extreme poverty levels, cultural beliefs and practices, war and conflicts, Social Determinants of Health (SDH), poor health education, and lack of awareness. There are huge variations of corneal disease distribution geographically.
In Asia, we found fungal keratitis, or fungal corneal ulcers, as a major blinding eye disease. About 105 species of fungi classified in 56 genera have been reported to cause keratomycosis3. Among such fungi, filamentous forms are the major etiologic agents involved in corneal ulcers. Use of corticosteroids or antibiotics, extraocular foreign bodies, trauma, post-operative infections, pre-existing eye diseases, contact lens, systemic illness, age, sex, climate and seasons, abrasion, burns and chemical injuries, corneal surface disorders, dry eye, exposure keratitis, etc. are the predisposing factors to cause fungal corneal ulcers in Asia people4. Fungal keratitis is particularly common in South Asian agricultural societies where trauma with vegetable matter or organic matter often leads to corneal ulceration5. The clinical appearance of fungal corneal ulcers varies greatly depending on the type of organisms, the duration of the disease, and the severity of infection6. Bangladesh is transitioning into a middle-developing nation, and policymakers are facing challenges in eliminating corneal blindness. The rate of corneal blindness in at least one eye ranged from 0.5% to 0.9%, which is higher than that reported in India7. A community-level study at Chittagong, Bangladesh, revealed that about 53.5% of bacteria and 39.9% of fungi were found as microbial etiology of corneal ulcers8. The incidence of fungal keratitis (42.86%) was higher than bacterial keratitis (25%) in Rajshahi, the northern part of Bangladesh9. Common predisposing factors of infectious keratitis in developing countries, including contact lenses, are common risk factors in developed countries10.
Evidence shows that corneal ulcer typically affects people in the most economically productive stage of life, with a median age of 40 years, and may reduce the vision-related quality of life11. The treatment is costly and prolonged if the case is represented as delayed. Patients in Low and Middle-Income Countries (LMIC) are typically poor, and they are not much aware of it in most cases; about ~60% of eyes are rendered blind12. A good outcome depends on early, appropriate treatment, correct identification of the causative organism, and careful follow-up. The leading causes of corneal blindness in Bangladesh have been reported to be keratitis and trauma. There is an absence of representative clinic-based data on the magnitude and etiologies of corneal diseases managed by ophthalmologists in Bangladesh. The identification of risk factors could lead to targeted improvements in public health measures, such as the promotion of eye protection to prevent trauma-related corneal injuries and hand hygiene to prevent the spread of infectious keratitis in any vulnerable group.
Materials and methods:
A meta-analysis protocol has been developed, followed by the PROSPERO database, and the protocol was prepared using the Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocol (PRISMA-P)13. The researchers completed the PRISMA-P checklist. A summary of eligibility criteria for Population, Intervention, Comparison, Outcome, and Study design (PICOS) was done.
In this meta-analysis and systematic review, the researcher has developed a standard protocol as well as a critical appraisal tool to produce evidence to understand the challenges and opportunities of corneal disease treatment.
followed by PRISMA meta-analysis and systematic review guidelines. Peer-reviewed articles and grey literature on the challenges and opportunities of corneal disease treatment, associated factors in corneal diseases, and access to treatment and treatment outcome of corneal diseases using very specific keywords were searched on eight resourceful websites, followed by inclusion and exclusion criteria. We used an SLR technique including three steps to extract the published articles and grey reports from different websites. The three steps are selecting the initial list of the articles and reports, techniques used to evaluate the article and the report, and data extraction and analysis. Our searched 8 websites are Science Direct, Wiley Online Library, Web of Science (SCI, SSCI, HCI), Google Scholar, Medline (PubMed), PMC, CINAHL, and Hindawi published between January 2010 to January 2024 published in the English language.
For the included clinical studies, the updated Cochrane risk-of-bias tool (RoV 2.0) was used to evaluate the perceived risk of bias within the randomized studies. For in vitro research, and as no pre-determined guidelines to assess the risk of bias exist, a modification of the Cochrane tool was implemented with an attempt to incorporate specific important elements that would help identify the presence of potential bias. We followed the Newcastle-Ottawa Quality Assessment Scale to assess the risk of bias regarding the selection of the studies. The Principal Investigator (PI) independently assessed the quality of the studies, and the co-investigators verified the evaluated studies. if researchers disagreed on interpretations, a discussion session of interpreters was held to reach a decision.
If the article is below an acceptable standard, the article is excluded from further analyses. Alternatively, studies of acceptable merit were further investigated through moderator analyses in an attempt to explain heterogeneity among effect sizes due to quality elements. We conducted this meta-analysis and systematic review by selecting sources and keywords, combining the most promising strings of keywords using logical operators, identifying search areas for articles and reports, and executing the search process to identify relevant empirical studies through screening based on specific inclusion and exclusion criteria.
A. Exploring the initial list of studies.
To explore the initial list of studies, the researcher searched the articles in the database using very specific keywords to find the desired articles and grey literature containing the words corneal ulcer, ulceration, challenges, opportunity, and treatment. We also searched corneal ulcer treatment outcomes, corneal ulcer challenges, and corneal ulcer treatment opportunities. We searched eight resourceful online databases for articles and grey literature published between January 2010 to January 2024 to gather the relevant articles and grey literature on corneal ulcer treatment outcomes, corneal ulcer challenges, and corneal ulcer treatment opportunities. We found a total of 32795 articles and grey literature by using specific keywords and the numbers returned about 26 by searching combined keywords.
Table 1: Initial Search strategy and outcomes
|
Total articles & grew literature found (January 2010 to January 2024) |
|||||||||
|
Search Databases |
Search items |
|
|||||||
|
Data sources |
Field and access |
Document Type |
Corneal Ulcer |
Corneal Ulcer Treatment |
Corneal Ulcer Treatment Challenges |
Corneal Ulcer Treatment Opportunities |
Corneal Ulcer Treatment Challenges & Opportunities |
Corneal Ulcer Treatment Challenges & Opportunities in Bangladesh |
Corneal Ulcer Treatment Challenges & Opportunities in Bangladesh & South Asia |
|
Springer link |
All |
Journals |
6, 300 |
2569 |
120 |
09 |
13 |
12 |
08 |
|
Science Direct |
All |
Journals |
6. 340 |
1967 |
345 |
93 |
05 |
06 |
04 |
|
Wiley Online Library |
All |
Journals |
5, 045 |
1890 |
256 |
112 |
22 |
08 |
03 |
|
Medline (PUB MED) |
All |
Journals |
4,328
|
1680 |
360 |
135 |
15 |
04 |
03 |
|
PMC |
All |
Journals |
2, 368 |
1867 |
245 |
55 |
12 |
04 |
02 |
|
Web of Science (SCI, SSCI, HCI) |
All |
Journals |
3, 375 |
1569 |
160 |
110 |
21 |
03 |
02 |
|
Hindawi |
All |
Journals |
1, 072 |
568 |
120 |
11 |
05 |
03 |
02 |
|
Google Scholar |
All |
Journals |
3, 967 |
1690 |
250 |
245 |
19 |
02 |
02 |
|
Total |
32795 |
13800 |
1861 |
770 |
102 |
42 |
26 |
||
B. Topicality of evaluation
We were alert in evaluating the standard and quality of articles and grey literature from the outcomes of the initial list of studies. The authors read all articles and grey literature titles and abstracts, execute summaries and full text to exclude irrelevant articles and reports. Furthermore, regarding the topicality of the evaluation of collected articles and grey literature, we followed our study protocol as well as inclusion and exclusion criteria (Figure 1).
C. Extraction and analysis of data
In the extraction and analysis of data stage, we selected articles and the grey literature considering key details of the relevant articles and grey literature based on inclusion and exclusion criteria [30] including duration of publications, types of outcome measures, deleting similar articles, the relevance of the results and no longitudinal studies and wrong intervention. Considering the above criteria, finally, we selected 12 articles and 3 grey literature and trusted websites to develop the background of the study. As a result, 12 articles and reports were selected for further analysis. Figure 1 below shows the results of the search and selection of studies with exclusion steps. Researchers developed a structured format form in the Excel sheet to extract information from each study. Title, author, country, journal, publication date, the main outcome, the study design (design, sample size, participants, risk bias, study quality assessment), the results (effect estimates and 95% CI), and limitations were included in the format. In the case of multiple studies that used the same data source, we considered the study as the most recent data. Following the methods of DerSimonian and Laird [31], the authors summarized to find out the challenges and opportunities of corneal ulcer treatment through a random-effects meta-analysis. We used RevMan V.5.4 to synthesize the data and ensure the adjusted ORs and 95% CIs.
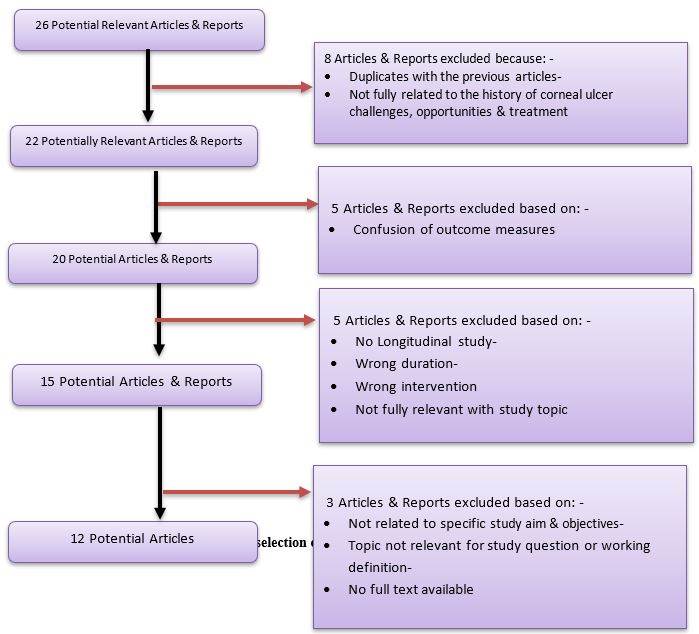
Figure 1: Results of the search and selection of studies with exclusion steps
Patient and public involvement:
In our study, there is no patient involved.
Statistical analysis:
This meta-analysis used the random-effects model due to heterogeneity to assess the challenges and opportunities of corneal ulcer disease treatment in Bangladesh [32]. Cochran’s Q χ2 statistic and the I2 tests were applied to assess the random variations between primary studies. The I2 test aims to understand the percentage variance in a meta-analysis attributable to heterogeneity among the studies [5]. In our meta-analysis, we interpreted as an I2 value of 0%=no heterogeneity, ≤25% = low, 25%–50%=moderate, 50–75=substantial and≥75% = high level heterogeneity. In the case of high heterogeneity, subgroup, and sensitivity analyses were conducted to identify possible moderators for the heterogeneity.
Table 2: Study types and quality assessment indicator for meta-analysis
|
Type of Study |
Coef. |
95% of CI. |
P value |
|
Community-based study |
8.6643212 |
6.2134922 |
p < 0.08 |
|
Hospital-based study |
9.6344344 |
7.0834934 |
p < 0.09 |
|
Clinical Study |
5.5341023 |
4.5534980 |
p < 0.04 |
|
Narrative review |
7.6027312 |
5.77377987 |
p < 0.06 |
|
Meta-Analysis |
4.4960233 |
4.2236981 |
p < 0.03 |
|
Systematic Review |
7.7744254 |
5.3334955 |
p < 0.09 |
|
Community intervention |
4.7935252 |
4.0083467 |
p < 0.02 |
|
National survey study |
4.6743244 |
4.0835581 |
p < 0.03 |
|
Community-based study |
7.6243290 |
5.1132922 |
p < 0.06 |
|
Hospital-based study |
5.0955211 |
4.5034087 |
p < 0.04 |
|
Hospital-based study |
3.9045431 |
3.2035900 |
p < 0.001 |
|
RCT |
3.7148173 |
3.5543762 |
p < 0.002 |
Risk of Bias assessment:
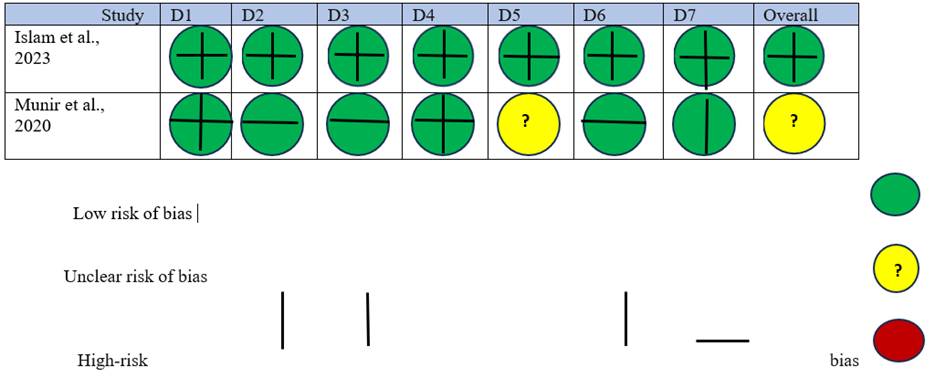
Fig. 2 Risk of bias in each domain of the included randomized control studies
D1: Random sequence generation (Selection bias)
D2: Allocation concealment (Selection bias)
D3: Blinding of participants and personnel (Performance bias)
D4: Blinding of outcome assessment (Detection bias)
D5: Incomplete outcome data (Attrition bias)
D6: Selective reporting (Reporting bias)
D7: Other bias
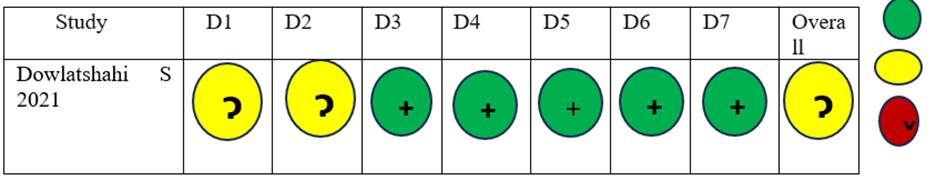
Fig. 3 Risk of bias in each domain of the included cohort studies
Domains:
D1: Bias due to confounding
D2: Bias due to selection of participants
D3: Bias in the classification of interventions
D4: Bias due to deviations from intended interventions
D5: Bias due to missing data
D6: Bias in measurement of outcome
D7: Bias in the selection of the reported result.
|
Study |
Item -1
|
Item-2a |
Item-2b |
Item-3 |
Item-4 |
Item-5 |
Item- 6 |
Item-7 |
Item- 8 |
Item- 9 |
Item-10 |
Item-11 |
Item-12 |
Item-13 |
Item-14 |
|
Singh, 2011 |
YES |
YES |
YES |
YES |
YES |
NO |
NO |
NO |
NO |
NO |
YES |
YES |
YES |
YES |
YES |
|
Sommer et al., 2014 |
YES |
YES |
YES |
YES |
YES |
NO |
NO |
NO |
NO |
NO |
YES |
YES |
NO |
YES |
YES |
|
Yusufu et al 2021 |
YES |
YES |
YES |
YES |
YES |
NO |
NO |
NO |
NO |
NO |
YES |
YES |
YES |
YES |
YES |
|
Anahita & Sayan 2023 |
YES |
YES |
YES |
YES |
YES |
NO |
NO |
NO |
NO |
NO |
YES |
NO |
YES |
YES |
YES |
|
Tran et al 2020 |
YES |
YES |
YES |
YES |
YES |
NO |
NO |
NO |
NO |
NO |
YES |
YES |
YES |
YES |
YES |
|
Shivangi & Pravin 2022 |
YES |
YES |
YES |
YES |
YES |
YES |
NO |
NO |
YES |
YES |
YES |
YES |
YES |
YES |
YES |
|
Rashid et al, 2020 |
YES |
YES |
YES |
YES |
YES |
NO |
NO |
NO |
YES |
YES |
YES |
YES |
YES |
YES |
YES |
|
Chowdhury et al., 2024 |
YES |
YES |
YES |
YES |
YES |
NO |
NO |
NO |
NO |
NO |
YES |
NO |
NO |
YES |
YES |
|
Hazlett et al 2016 |
YES |
YES |
YES |
YES |
YES |
NO |
NO |
NO |
NO |
NO |
YES |
YES |
NO |
YES |
YES |
Item 1. Structured summary of trial design, methods, results, and conclusions.
Item 2a. Scientific background and explanation of rationale.
Item 2b. Specific objectives and/or hypotheses.
Item 3. The intervention for each group, including how and when it was administered, with sufficient detail to enable replication.
Item 4. Completely defined, pre-specified primary and secondary measures of outcome, including how and when they were assessed.
Item 5. How sample size was determined.
Item 6. The method used to generate the random allocation sequence.
Item 7. The mechanism used to implement the random allocation sequence (for example, sequentially numbered containers), describes any steps taken to conceal the sequence until intervention was assigned.
Item 8. Who generated the random allocation sequence, and who enrolled?
Item 9. If done, who was blinded after assignment to intervention (for example, care providers, those assessing outcomes), and how
Item 10. Statistical methods are used to compare groups for primary and secondary outcomes.
Item 11. For each primary and secondary outcome, results for each group, and the estimated size of the effect and its precision (for example 95% confidence interval).
Item 12. Trial limitations, addressing sources of potential bias, imprecision, and, if relevant, multiplicity of analyses.
Item 13. Sources of funding and other support (for example suppliers of drugs), role of funders.
Item 14. Where the full trial protocol can be accessed, if available.
Results:
Key Challenges of the Corneal Ulcer Treatment
Challenges of corneal disease care & treatment:
Absent of corneal disease diagnostic facilities, non-availability of sophisticated tools, limited centers of excellence with modern technology, and lack of symptom-based diagnosis facilities14. Scarcity of well-trained surgeons and nurses, shortage of modern operating rooms and good equipment, non-availability of eye bank facilities, absence of regular follow-up of clinical services and treatment, and Social Determinants of Health (SDH) play roles as push factors to ensure the corneal ulcer treatment in South Asia countries15.
Surgical intervention and post-operative service costs are barriers to reducing corneal ulcer-related blindness in developing countries. Considering the cost of corneal ulcers, prevention strategies, and policies cost-effective tools, and successful programs in decreasing the number of corneal ulcer cases and the prevalence of blindness in Bangladesh16. About 95% of African countries' corneal ulcer cases are preventable or treatable if patients are attended to in the clinic or hospital promptly and physicians ensure the referral of those cases to a tertiary hospital17. Innovative programs, including telehealth consultation through primary eye health centers in rural settings, may reduce the corneal-related blindness burden in developing countries. This approach is important for mobilizing public health resources for the underprivileged community and reducing the global burden of visual disability18.
Challenges of developing new treatments for corneal diseases:
There are no susceptibility standards for topical therapy for corneal disease treatment (Hazlett et al., 2016). Topical ocular antibiotics are likely to result in higher concentrations at the corneal surface than would be present following systemic administration19. Unfortunately, these concentrations are quickly diminished by reflex tearing and blinking after instillation20. Since there is currently no standard to measure the efficacy of topical therapies, it must be assumed that antibiotic concentrations reached in the ocular tissues are at an equal or greater concentration than would be seen in the serum21. Studies have been done in animal and human models to determine the PK concentration of topical antibiotics used in ocular disease21. Combining this information with MIC data provides the potential to predict clinical efficacy, however, the issues with drug delivery are only one of the many challenges to treating ocular infections22.
Challenges of Resistant strains
The development of methicillin-resistant S. aureus (MRSA) is a significant clinical problem regarding appropriate and effective treatment23. Resistance has developed over time and is due to many factors: extended prophylaxis, overuse of antibiotics for systemic infections, in agriculture, sub-therapeutic doses, and misuse for non-bacterial infections, as well as specific bacterial species, that predispose them to resistance24. The emergence of MRSA strains, resistant to the most commonly used fluoroquinolones has resulted in the necessity to develop new antimicrobials for bacterial keratitis.
Challenges of use of Antibiotics
The objective of antibiotic therapy is to rapidly eliminate the corneal pathogen. Monotherapy with fourth-generation fluoroquinolones (moxifloxacin or gatifloxacin is the current, most commonly used antibiotic therapy. However, P. aeruginosa has a high ability to trigger antibiotic resistance mechanisms making them difficult to eradicate even25.
Challenges of Corneal cross-linking
Corneal cross-linking (CXL) and more specifically, PACK-CXL (photoactivated chromophore for infectious keratitis-CXL) is a new therapeutic approach to treating infectious corneal diseases26. The technique employs riboflavin drops and 365 nm ultraviolet-A light to generate additional cross-links in the cornea. Specifically, the riboflavin acts as a chromophore and releases free radicals, creating new bonds between collagen fibers and proteoglycans27. These additional cross-links increase the overall biomechanical strength of the cornea. It is difficult to see how blindness from corneal ulcers worldwide can be reduced dramatically with the treatment of the ulcers themselves; cases often present too late to prevent the corneal scarring that causes blindness28.
Challenges of adaptation of guidelines and protocol:
Many tertiary eye care centers have their oldest protocol for managing corneal ulcers. There are no updated modern WHO recommendation guidelines and protocols for suitable modification according to the circumstances of corneal ulcers29. Microbial keratitis due to fungal, bacterial, or viral infection, particularly HSV, can result in significant vision loss secondary to corneal scarring and other adverse events, and such diseases may be controlled and prevented following standard guidelines and protocol for treatment30.
Key Opportunities:
Opportunities for corneal disease treatment in Bangladesh:
Addressing the above challenges, we need a multipole approach: enhancing the supply chain for existing medications and developing new, low-cost treatment alternatives for developing countries like Bangladesh31. Local manufacturing initiatives, subsidized treatment programs, and the use of generic drugs could play pivotal roles in making corneal disease treatments more accessible in poor resource settings32. Community-based management programs could offer practical support and education to patients, improving adherence and treatment outcomes33.
Bridging this gap requires the innovation of cost-effective, accessible diagnostic tools and comprehensive training for healthcare workers in their use. Regular diagnosis makes it a routine part of ocular health assessments in primary care settings34. Telemedicine could address these challenges in the developing world. prevention of corneal blindness, appropriate treatment modalities, and providing adequate rehabilitation services to the patients35.
Clinical and community-based research related to the prevention of suppurative keratitis and enhancing host resistance immediate need to pursue. Large-scale public education programs to sensitize those at risk of suppurative keratitis, and to encourage earlier presentation, should be undertaken36. Coupled with this, education of practitioners, general physicians, and other health workers, as well as general ophthalmologists, will go a long way towards ensuring correct diagnosis, appropriate treatment, and timely referral before extensive damage to the cornea occurs37. Management of corneal abrasions at primary care levels within 48 hours has been demonstrated by various studies to be the best way to prevent corneal ulcers in low- and middle-income countries38. This could be adopted in any population and is cost-effective both for health providers and the patient.
Effective management at the secondary level & appropriate referral to tertiary hospital:
Well-trained ophthalmologist and/or an ophthalmic assistant, or a physician trained in a community setting a vital issue for managing corneal diseases in low-resource settings.
Public-private partnerships follow the unified approach to bringing together healthcare providers, policymakers, the financial sector, the pharmaceutical industry, and communities that may reduce the corneal ulcer-related burden in Bangladesh39. By integrating awareness campaigns, improving diagnostic and treatment accessibility, and ensuring ethical industry practices, significant strides can be made in corneal disease management40.
Budget-appropriate diagnostics, treatment accessibility, and committed financial and pharmaceutical industry involvement, it is possible to transform the landscape of corneal disease care in Bangladesh, ensuring that those in need receive effective, compassionate, and equitable eye care treatment41.
The use of small molecules that downregulate the host inflammatory response, especially to danger-associated molecular pattern molecules, such as HMGB1, is anticipated. Therapeutically, alternative approaches to corticosteroid treatment, such as topical cyclosporine to manage ongoing HSK will be utilized. PACK-CXL (for bacterial) and DALK (for HSK) procedures will also potentially provide better management and outcomes for keratitis patients 41-42.
Based on the above-mentioned clinical patterns newer strategies may be adopted to reduce the morbidity associated with this condition are likely going to have to be multidimensional, involving corneal ulcer prevention, improved early and accurate diagnostics techniques such as next-generation sequencing, and novel antimicrobial agents to address the development of drug resistance. Adjuvant therapies that focus on modifying the immune response to the infection, thereby reducing the corneal melting and scarring that ultimately lead to poor vision, may have the greatest potential to improve clinical outcomes42.
As microbial keratitis is more common in middle-aged people with low socioeconomic status working in outdoor occupations, Community-based awareness programs and ophthalmologists should train for proper diagnosis and management of microbial keratitis43
DED and MGD are common among Bangladesh garment factory workers. MGD and reduced tear stability play important roles in dry eye symptoms. The mixed type of DED is most common, with significantly worse symptoms in this subgroup. The use of a standard force MG evaluator may be advantageous for clinical and epidemiological assessment of MG function. Emerging treatments for MGD may play a bigger role in people in certain occupational groups who suffer from a higher risk of dry eye42-43.
Role of the Pharmaceutical Industry in Corneal Disease Treatment
Pharmaceutical companies in developing countries are a crucial part of such eye diseases. Beyond merely supplying medications and investing in the development of new drugs and devices, there is a moral imperative for these entities to initiate the reverse engagement of new drugs to provide early induction of new treatment modalities. Such involvement should be guided by a genuine commitment to improving public health outcomes and balancing profitability with social responsibility. These goals should then be facilitated and institutionalized by enlightened government policies and administration. Collaborative partnerships between governments, non-governmental organizations, and industry have been shown, albeit up to now on smaller scales, to facilitate such an approach, ensuring that corneal disease management becomes a shared priority43.
Role of the Cornea Society of Bangladesh
Senior ophthalmologists leading corneal disease treatment and research under the umbrella of the Cornea Society and being the de facto authority in this field could assume these roles, both as an organization and just as important, as individual members42-43.
Changing the One Donor–One Recipient Paradigm
Traditionally, a single donor cornea has been used to restore sight to a single recipient. However, with the widespread adoption of lamellar keratoplasty techniques, one donor corneal tissue can be used for 2 patients (such as for deep anterior lamellar keratoplasty and Descemet membrane endothelial keratoplasty), where permissible43. In addition, the lower rates of corneal transplant rejection associated with anterior and posterior lamellar keratoplasty techniques compared with penetrating keratoplasty translate to decreased rates of graft failure and the need for repeat keratoplasty44. Anterior lamellar keratoplasty also permits the use of corneal tissue with poorer endothelial quality, the tissue that would otherwise be discarded or used only for tectonic keratoplasty, to be used for optical keratoplasty43-44.
Alternatives to Traditional Cadaveric Human Donor Corneas
Complicated and end-stage treatment of corneal disease is a big challenge for the ophthalmologist, and there are limited options for giving treatment to the patients50. In this case, corneal transplantation is the lifeline treatment option, but the shortage of transplants and the lack of trained surgeons limiting access to transplantations are barriers to giving such treatment in developing 43. Although such donor corneal tissue has limited applicability for some indications, an artificial cornea is widely used in this treatment. The high rate of complications, including neuroprosthetic membrane formation, glaucoma, corneal melting, and endophthalmitis, has not scaled to meet the challenge of the treatment. Considering the above situation, KPros is currently used as a last resort with a global implantation rate reaching only 1000–2000 cases annually44.
Establishing of Regional Corneal Eye Bank:
Under the umbrella of SARRAC, a regional cornea eye bank may be established, and member countries can share the cornea according to their needs. SARRAC country's cornea society may play a vital role in this context44.
Discussion:
Still, corneal diseases are prevalent in Bangladesh and other developing countries, and preventive interventions and ophthalmic clinical services are not up to the mark in low-resource settings. The aged population, occupational factors, socio-demographic status, and faster development activities are associated with an increased burden of corneal disease in Bangladesh.
Visual impairment from corneal diseases hardly affects the productive years of poor communities, especially women. Our four studies suggest that the prevalence of corneal opacity in rural Bangladesh, India, Nepal, and China has a significantly higher prevalence of infectious keratitis 6-9.
There are about 2 million people in China and 7 million people in India awaiting a corneal transplant, unfortunately, there is no accurate information about the corneal disease burden in Bangladesh10.
About 8 million people in Bangladesh are suffering from eye diseases, and it is estimated that among them, around 5,00,000 of those patients are suffering from corneal diseases, and some of them are waiting for corneal transplantation11.
After the independence of Bangladesh, we improved our eye health care, although the burden of corneal blindness in Bangladesh remains a significant eye health problem. Address this eye health burden with a multi-stakeholder approach, including regional eye bank facilities, timely collection of donor corneas and imported tissue, changing the one donor-one recipient paradigm, using alternatives to traditional cadaveric human donor corneas, and expanding corneal surgeon training are important factors that need to address for corneal disease services and treatments.
One newspaper report shows that annually, Bangladesh needs at least 20,000 to 25,000 corneas, but we can meet only 5% to 10% of this demand, and imported corneas are not enough to meet the demand for corneal transplants. Cultural taboos, poor awareness, poor public-private partnership approach, and lack of appropriate policy are responsible for the narrow scope of the corneal collection from local sources.
In the last 30 years, in Bangladesh, the number of corneal doctors has increased, but unfortunately, the number of eye banks and the supply of corneas did not increase following the number of surgeons. There has been no national cornea disease survey taking place since Bangladesh’s independence.
Diagnostic facilities, the non-availability of equipment, limited centers of excellence with modern technology, and a lack of symptom-based diagnosis facilities are key factors in getting corneal services in Bangladesh. Scarcity of well-trained ophthalmic nurses and surgeons in rural and remote areas, and nurses. No regular follow-up of clinical services and Social Determinants of Health (SDH) factors harm corneal ulcer treatment in Bangladesh. Adaptation with modern surgical intervention and accessible post-operative service costs may reduce corneal ulcer-related blindness in Bangladesh. Revised prevention strategies and policies for public-private partnerships for corneal disease treatment in Bangladesh are needed.
Most studies suggest that about 95% of corneal ulcer cases are preventable or treatable. An effective and appropriate referral system may be the best option for the prevention and quality of treatment of corneal disease in Bangladesh. Three studies suggested that telehealth consultation is an innovative program for primary eye health centers in rural settings to reduce corneal-related blindness in Bangladesh. Community-based public health resources may be utilized for underprivileged communities and reduce the burden of visual disability.
We summarize the challenges and opportunities of corneal disease treatment in Bangladesh and the South Asia region and Corneal ulceration and trauma were the two major causes of corneal blindness in this region. In Bangladesh and Nepal, corneal trauma and ulceration are considered the second leading cause of unilateral visual loss after cataracts.
Diagnostic facilities, the non-availability of equipment, limited centers of excellence with modern technology, and a lack of symptom-based diagnosis facilities. Scarcity of well-trained ophthalmic nurses and surgeons in rural and remote areas, and nurses. No regular follow-up of clinical services and Social Determinants of Health (SDH) factors harm corneal ulcer treatment in Bangladesh. Adaptation with modern surgical intervention and accessible post-operative service costs may reduce corneal ulcer-related blindness in Bangladesh. Revised prevention strategies and policies for public-private partnerships for corneal disease treatment in Bangladesh are needed.
Most studies suggest that about 95% of corneal ulcer cases are preventable or treatable. An effective and appropriate referral system may be the best option for the prevention and quality of treatment of corneal disease in Bangladesh.
Three studies suggested that telehealth consultation is an innovative program for primary eye health centers in rural settings to reduce corneal-related blindness in Bangladesh. Community-based public health resources may be utilized for underprivileged communities and reduce the burden of visual disability.
Some studies focus on topical therapy for corneal disease treatment. Although there is no standard to measure the efficacy of topical therapies, some clinical research may be conducted on this topic. The development of methicillin-resistant S. aureus (MRSA) is a significant clinical problem about appropriate and effective treatment.
Antibiotic therapy is frequently used in our country, and monotherapy with fourth-generation fluoroquinolones is the most commonly used antibiotic therapy. However, P. aeruginosa has a high ability to trigger antibiotic resistance mechanisms, making them difficult to eradicate. Many developed countries use corneal cross-linking (CXL) and, more specifically, PACK-CXL as a new therapeutic approach to treat infectious corneal diseases. We may think of such an approach in our country's context.
Microbial keratitis due to fungal, bacterial, or viral infection, particularly HSV, can result in significant vision loss secondary to corneal scarring and other adverse events, and such diseases may be controlled and prevented following standard guidelines and protocol for treatment. secondary and tertiary eye care centers used the old protocol for managing corneal ulcers. WHO-recommended guidelines and protocols for suitable modification according to the circumstances of corneal ulcers may be adapted.
Some studies reveal that a continuous supply of medications and the development of new drugs with low-cost treatment, subsidized treatment programs, and the use of generic drugs could play pivotal roles in making corneal disease treatments more accessible in poor resource settings. Bridging this gap requires the innovation of cost-effective, accessible diagnostic tools, and comprehensive training for healthcare workers is needed. Clinical and community-based research related to the prevention of suppurative keratitis and host resistance is immediately needed. Large-scale public education programs to sensitize those at risk of suppurative keratitis and to encourage earlier presentation should be undertaken. Coupled with this, education of practitioners, general physicians, and other health workers, as well as general ophthalmologists, will go a long way towards ensuring correct diagnosis, appropriate treatment, and timely referral before extensive damage to the cornea occurs. Management of corneal abrasions at primary care levels within 48 hours has been demonstrated by various studies to be the best way to prevent corneal ulcers in low- and middle-income countries.3-6 This could be adopted in any population and is cost-effective both for health providers and the patient.
Budget-appropriate diagnostics, treatment accessibility, and committed financial engagement of the pharmaceutical industry for corneal disease care in Bangladesh are required to ensure effective, compassionate, and equitable corneal disease treatment. Collaborative partnerships between governments, non-governmental organizations, and industry are new approaches to ensure corneal disease management as a priority policy. The Cornea Society, being the de facto authority in this field, could play vital roles, both as an organization and, just as important, as individual members in improving corneal treatment. Under the umbrella of SARRAC, a regional cornea eye bank may be established, and member countries can share the cornea according to their needs. SARRAC country's cornea society may play a vital role in this context.
Conclusion
Bangladesh is facing unique challenges and unmet needs for the management and treatment of corneal disease. These challenges are closely associated with the opportunity of the discussed issue, and the scientific and clinical solutions lens may be a significant factor. To deliver optimal ophthalmic services to satisfy the great demands of corneal disease patients, we also need to address the socio-demographic factors.
Acknowledgment:
We are grateful to Gaco Pharmaceuticals Ltd. for their cordial support of this study.
Author contributions:
All authors together conceived and developed the study under the lead of the first author. The 1st, and 5th authors developed the study protocol. All authors attended the synthesis of the data into an Excel data sheet for analysis and writing the draft version. All authors developed the first draft and the entire team discussed the results and contributed to the final manuscript. All authors read and approved the final draft of the manuscript.
Conflict of Interest:
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
 Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. Published 2015 Jan 1. doi:10.1186/2046-4053-4-1
Moher D, Shamseer L, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1. Published 2015 Jan 1. doi:10.1186/2046-4053-4-1 Sanders R, Gascoyne B, Appleby P, Rashida SA, Jolley E. Eye Health Service Uptake among People with Visual Impairment and Other Functional Difficulties in Bangladesh: A Cross-Sectional Study with Short-Term Follow-Up. Int J Environ Res Public Health. 2021;18(17):9068. Published 2021 Aug 27. doi:10.3390/ijerph18179068
Sanders R, Gascoyne B, Appleby P, Rashida SA, Jolley E. Eye Health Service Uptake among People with Visual Impairment and Other Functional Difficulties in Bangladesh: A Cross-Sectional Study with Short-Term Follow-Up. Int J Environ Res Public Health. 2021;18(17):9068. Published 2021 Aug 27. doi:10.3390/ijerph18179068 Shrime MG, Hamer M, Mukhopadhyay S, et al. Effect of removing the barrier of transportation costs on surgical utilisation in Guinea, Madagascar, and the Republic of Congo. BMJ Glob Health. 2017;2(Suppl 4):e000434. Published 2017 Sep 26. doi:10.1136/bmjgh-2017-000434
Shrime MG, Hamer M, Mukhopadhyay S, et al. Effect of removing the barrier of transportation costs on surgical utilisation in Guinea, Madagascar, and the Republic of Congo. BMJ Glob Health. 2017;2(Suppl 4):e000434. Published 2017 Sep 26. doi:10.1136/bmjgh-2017-000434 Ung L, Chodosh J. Urgent unmet needs in the care of bacterial keratitis: An evidence-based synthesis. Ocul Surf. 2023;28:378-400. doi:10.1016/j.jtos.2021.08.013
Ung L, Chodosh J. Urgent unmet needs in the care of bacterial keratitis: An evidence-based synthesis. Ocul Surf. 2023;28:378-400. doi:10.1016/j.jtos.2021.08.013 Pavel, M.S., Chakrabarty, S. & Gow, J. Cost of illness for outpatients attending public and private hospitals in Bangladesh. Int J Equity Health 15, 167 (2016). https://doi.org/10.1186/s12939-016-0458-x
Pavel, M.S., Chakrabarty, S. & Gow, J. Cost of illness for outpatients attending public and private hospitals in Bangladesh. Int J Equity Health 15, 167 (2016). https://doi.org/10.1186/s12939-016-0458-x Hazlett L, Suvas S, McClellan S, Ekanayaka S. Challenges of corneal infections. Expert Rev Ophthalmol. 2016;11(4):285-297. doi:10.1080/17469899.2016.1203254
Hazlett L, Suvas S, McClellan S, Ekanayaka S. Challenges of corneal infections. Expert Rev Ophthalmol. 2016;11(4):285-297. doi:10.1080/17469899.2016.1203254 Rashid MM, Akhtar Z, Chowdhury S, et al. Pattern of Antibiotic Use among Hospitalized Patients according to WHO Access, Watch, Reserve (AWaRe) Classification: Findings from a Point Prevalence Survey in Bangladesh. Antibiotics (Basel). 2022;11(6):810. Published 2022 Jun 16. doi:10.3390/antibiotics11060810
Rashid MM, Akhtar Z, Chowdhury S, et al. Pattern of Antibiotic Use among Hospitalized Patients according to WHO Access, Watch, Reserve (AWaRe) Classification: Findings from a Point Prevalence Survey in Bangladesh. Antibiotics (Basel). 2022;11(6):810. Published 2022 Jun 16. doi:10.3390/antibiotics11060810 Mondal H, Kim HJ, Mohanto N, Jee JP. A Review on Dry Eye Disease Treatment: Recent Progress, Diagnostics, and Future Perspectives. Pharmaceutics. 2023;15(3):990. Published 2023 Mar 19. doi:10.3390/pharmaceutics15030990
Mondal H, Kim HJ, Mohanto N, Jee JP. A Review on Dry Eye Disease Treatment: Recent Progress, Diagnostics, and Future Perspectives. Pharmaceutics. 2023;15(3):990. Published 2023 Mar 19. doi:10.3390/pharmaceutics15030990 Ray P, Singh S, Gupta S. Topical antimicrobial therapy: Current status and challenges. Indian J Med Microbiol. 2019;37(3):299-308. doi:10.4103/ijmm.IJMM_19_443
Ray P, Singh S, Gupta S. Topical antimicrobial therapy: Current status and challenges. Indian J Med Microbiol. 2019;37(3):299-308. doi:10.4103/ijmm.IJMM_19_443 Agrahari V, Mandal A, Agrahari V, et al. A comprehensive insight on ocular pharmacokinetics. Drug Deliv Transl Res. 2016;6(6):735-754. doi:10.1007/s13346-016-0339-2
Agrahari V, Mandal A, Agrahari V, et al. A comprehensive insight on ocular pharmacokinetics. Drug Deliv Transl Res. 2016;6(6):735-754. doi:10.1007/s13346-016-0339-2 Cabrera FJ, Wang DC, Reddy K, Acharya G, Shin CS. Challenges and opportunities for drug delivery to the posterior of the eye. Drug Discov Today. 2019;24(8):1679-1684. doi:10.1016/j.drudis.2019.05.035
Cabrera FJ, Wang DC, Reddy K, Acharya G, Shin CS. Challenges and opportunities for drug delivery to the posterior of the eye. Drug Discov Today. 2019;24(8):1679-1684. doi:10.1016/j.drudis.2019.05.035 Nandhini P, Kumar P, Mickymaray S, Alothaim AS, Somasundaram J, Rajan M. Recent Developments in Methicillin-Resistant Staphylococcus aureus (MRSA) Treatment: A Review. Antibiotics (Basel). 2022;11(5):606. Published 2022 Apr 29. doi:10.3390/antibiotics11050606
Nandhini P, Kumar P, Mickymaray S, Alothaim AS, Somasundaram J, Rajan M. Recent Developments in Methicillin-Resistant Staphylococcus aureus (MRSA) Treatment: A Review. Antibiotics (Basel). 2022;11(5):606. Published 2022 Apr 29. doi:10.3390/antibiotics11050606 Hazlett LD, Xu S, Somayajulu M, McClellan SA. Host-microbe interactions in cornea. Ocul Surf. 2023;28:413-423. doi:10.1016/j.jtos.2021.09.008
Hazlett LD, Xu S, Somayajulu M, McClellan SA. Host-microbe interactions in cornea. Ocul Surf. 2023;28:413-423. doi:10.1016/j.jtos.2021.09.008 Tovar AA, Frankel ST, Galor A, Sabater AL. Living with Dry Eye Disease and its Effects on Quality of Life: Patient, Optometrist, and Ophthalmologist Perspectives. Ophthalmol Ther. 2023;12(5):2219-2226
Tovar AA, Frankel ST, Galor A, Sabater AL. Living with Dry Eye Disease and its Effects on Quality of Life: Patient, Optometrist, and Ophthalmologist Perspectives. Ophthalmol Ther. 2023;12(5):2219-2226 Sharma N, Arora T, Singhal D, et al. Procurement, storage and utilization trends of eye banks in India. Indian J Ophthalmol. 2019; 67:1056–1059
Sharma N, Arora T, Singhal D, et al. Procurement, storage and utilization trends of eye banks in India. Indian J Ophthalmol. 2019; 67:1056–1059 Pan CW, Qian DJ, Sun HP, et al. Visual impairment among older adults in a rural community in Eastern China. J Ophthalmol. 2016;2016: 9620542.
Pan CW, Qian DJ, Sun HP, et al. Visual impairment among older adults in a rural community in Eastern China. J Ophthalmol. 2016;2016: 9620542. Srinivasan M, Ravilla T, Vijayakumar V, et al. Community Health Workers for Prevention of Corneal Ulcers in South India: A Cluster-Randomized Trial. Am J Ophthalmol. 2022;237:259-266. doi:10.1016/j.ajo.2021.12.010
Srinivasan M, Ravilla T, Vijayakumar V, et al. Community Health Workers for Prevention of Corneal Ulcers in South India: A Cluster-Randomized Trial. Am J Ophthalmol. 2022;237:259-266. doi:10.1016/j.ajo.2021.12.010 Agarwal S, Khan TA, Vanathi M, Srinivasan B, Iyer G, Tandon R. Update on diagnosis and management of refractory corneal infections. Indian J Ophthalmol. 2022;70(5):1475-1490. doi:10.4103/ijo.IJO_2273_21
Agarwal S, Khan TA, Vanathi M, Srinivasan B, Iyer G, Tandon R. Update on diagnosis and management of refractory corneal infections. Indian J Ophthalmol. 2022;70(5):1475-1490. doi:10.4103/ijo.IJO_2273_21 Cabrera-Aguas M, Khoo P, Watson SL. Infectious keratitis: A review. Clin Exp Ophthalmol. 2022;50(5):543-562. doi:10.1111/ceo.14113
Cabrera-Aguas M, Khoo P, Watson SL. Infectious keratitis: A review. Clin Exp Ophthalmol. 2022;50(5):543-562. doi:10.1111/ceo.14113 Cicinelli MV, Marmamula S, Khanna RC. Comprehensive eye care - Issues, challenges, and way forward. Indian J Ophthalmol. 2020;68(2):316-323. doi:10.4103/ijo.IJO_17_19
Cicinelli MV, Marmamula S, Khanna RC. Comprehensive eye care - Issues, challenges, and way forward. Indian J Ophthalmol. 2020;68(2):316-323. doi:10.4103/ijo.IJO_17_19 Lubega M, Ogwok J, Nabunya B, Mbalinda SN. Role of community-based health clubs in promoting patients' health education for diabetes self-care management: an interventional qualitative study in a Ugandan urban setting. BMJ Open Qual. 2023;12(4):e002473. Published 2023 Dec 22. doi:10.1136/bmjoq-2023-002473
Lubega M, Ogwok J, Nabunya B, Mbalinda SN. Role of community-based health clubs in promoting patients' health education for diabetes self-care management: an interventional qualitative study in a Ugandan urban setting. BMJ Open Qual. 2023;12(4):e002473. Published 2023 Dec 22. doi:10.1136/bmjoq-2023-002473 Jo Y, LeFevre AE, Healy K, et al. Costs and cost-effectiveness analyses of mCARE strategies for promoting care seeking of maternal and newborn health services in rural Bangladesh. PLoS One. 2019;14(10):e0223004. Published 2019 Oct 1. doi:10.1371/journal.pone.0223004
Jo Y, LeFevre AE, Healy K, et al. Costs and cost-effectiveness analyses of mCARE strategies for promoting care seeking of maternal and newborn health services in rural Bangladesh. PLoS One. 2019;14(10):e0223004. Published 2019 Oct 1. doi:10.1371/journal.pone.0223004 Tidke SC, Tidake P. A Review of Corneal Blindness: Causes and Management. Cureus. 2022;14(10):e30097. Published 2022 Oct 9. doi:10.7759/cureus.30097
Tidke SC, Tidake P. A Review of Corneal Blindness: Causes and Management. Cureus. 2022;14(10):e30097. Published 2022 Oct 9. doi:10.7759/cureus.30097 Upadhyay MP, Srinivasan M, Whitcher JP. Diagnosing and managing microbial keratitis. Community Eye Health. 2015;28(89):3-6.
Upadhyay MP, Srinivasan M, Whitcher JP. Diagnosing and managing microbial keratitis. Community Eye Health. 2015;28(89):3-6. Lee PP. Vision and Public Health: Framing a Purpose for Our Work. Ophthalmology. 2017;124(2):148-150. doi:10.1016/j.ophtha.2016.11.003
Lee PP. Vision and Public Health: Framing a Purpose for Our Work. Ophthalmology. 2017;124(2):148-150. doi:10.1016/j.ophtha.2016.11.003 Rathi VM, Thokala P, MacNeil S, Khanna RC, Monk PN, Garg P. Early treatment of corneal abrasions and ulcers-estimating clinical and economic outcomes. Lancet Reg Health Southeast Asia. 2022;4:100038. doi:10.1016/j.lansea.2022.100038
Rathi VM, Thokala P, MacNeil S, Khanna RC, Monk PN, Garg P. Early treatment of corneal abrasions and ulcers-estimating clinical and economic outcomes. Lancet Reg Health Southeast Asia. 2022;4:100038. doi:10.1016/j.lansea.2022.100038
 Kate A, Basu S. Corneal blindness in the developing world: The role of prevention strategies. F1000Res. 2024;12:1309. Published 2024 Mar 5. doi:10.12688/f1000research.141037.2
Kate A, Basu S. Corneal blindness in the developing world: The role of prevention strategies. F1000Res. 2024;12:1309. Published 2024 Mar 5. doi:10.12688/f1000research.141037.2 Ahmed M, Whitestone N, Patnaik JL, et al. Burden of eye disease and demand for care in the Bangladesh Rohingya displaced population and host community: A cohort study. PLoS Med. 2020;17(3):e1003096. Published 2020 Mar 31. doi:10.1371/journal.pmed.1003096
Ahmed M, Whitestone N, Patnaik JL, et al. Burden of eye disease and demand for care in the Bangladesh Rohingya displaced population and host community: A cohort study. PLoS Med. 2020;17(3):e1003096. Published 2020 Mar 31. doi:10.1371/journal.pmed.1003096 https://link.springer.com/article/10.1007/s10903-018-0766-x
https://link.springer.com/article/10.1007/s10903-018-0766-x https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(13)70003-2/fulltext
https://www.thelancet.com/journals/langlo/article/PIIS2214-109X(13)70003-2/fulltext Islam MM; Nuzhath T. Health risks of Rohingya refugee population in Bangladesh: a call for global attention. J Glob Health. 2018 Nov 9. https://doi.org/10.7189/jogh.08.020309
Islam MM; Nuzhath T. Health risks of Rohingya refugee population in Bangladesh: a call for global attention. J Glob Health. 2018 Nov 9. https://doi.org/10.7189/jogh.08.020309 Tannoury M, Attieh Z. The Influence of Emerging Markets on the Pharmaceutical Industry. Curr Ther Res Clin Exp. 2017;86:19-22. Published 2017 Apr 18. doi:10.1016/j.curtheres.2017.04.005
Tannoury M, Attieh Z. The Influence of Emerging Markets on the Pharmaceutical Industry. Curr Ther Res Clin Exp. 2017;86:19-22. Published 2017 Apr 18. doi:10.1016/j.curtheres.2017.04.005 Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution [published correction appears in Lancet Glob Health. 2018 Nov;6(11):e1162. doi: 10.1016/S2214-109X(18)30438-8] [published correction appears in Lancet Glob Health. 2018 Nov;6(11):e1162. doi: 10.1016/S2214-109X(18)30456-X] [published correction appears in Lancet Glob Health. 2021 Aug;9(8):e1067. doi: 10.1016/S2214-109X(21)00250-3]. Lancet Glob Health. 2018;6(11):e1196-e1252. doi:10.1016/S2214-109X(18)30386-3
Kruk ME, Gage AD, Arsenault C, et al. High-quality health systems in the Sustainable Development Goals era: time for a revolution [published correction appears in Lancet Glob Health. 2018 Nov;6(11):e1162. doi: 10.1016/S2214-109X(18)30438-8] [published correction appears in Lancet Glob Health. 2018 Nov;6(11):e1162. doi: 10.1016/S2214-109X(18)30456-X] [published correction appears in Lancet Glob Health. 2021 Aug;9(8):e1067. doi: 10.1016/S2214-109X(21)00250-3]. Lancet Glob Health. 2018;6(11):e1196-e1252. doi:10.1016/S2214-109X(18)30386-3 Kate A, Basu S. Corneal blindness in the developing world: The role of prevention strategies. F1000Res. 2024;12:1309. Published 2024 Mar 5. doi:10.12688/f1000research.141037.2
Kate A, Basu S. Corneal blindness in the developing world: The role of prevention strategies. F1000Res. 2024;12:1309. Published 2024 Mar 5. doi:10.12688/f1000research.141037.2 Singh NP, Said DG, Dua HS. Lamellar keratoplasty techniques. Indian J Ophthalmol. 2018;66(9):1239-1250. doi:10.4103/ijo.IJO_95_18
Singh NP, Said DG, Dua HS. Lamellar keratoplasty techniques. Indian J Ophthalmol. 2018;66(9):1239-1250. doi:10.4103/ijo.IJO_95_18 Alanazi LF, Aldossari SH, Gogandy MA, Althubaiti GA, Alanazi BF, Alfawaz AM. Attitude, beliefs and awareness towards corneal donation in Saudi Arabia. Saudi J Ophthalmol. 2019;33(2):121-129. doi:10.1016/j.sjopt.2019.02.003
Alanazi LF, Aldossari SH, Gogandy MA, Althubaiti GA, Alanazi BF, Alfawaz AM. Attitude, beliefs and awareness towards corneal donation in Saudi Arabia. Saudi J Ophthalmol. 2019;33(2):121-129. doi:10.1016/j.sjopt.2019.02.003 Basak SK. Data gap: Transplantable corneal blindness, current transplantation, and eye banking in India. Indian J Ophthalmol. 2023;71(9):3125-3127. doi:10.4103/IJO.IJO_2096_23
Basak SK. Data gap: Transplantable corneal blindness, current transplantation, and eye banking in India. Indian J Ophthalmol. 2023;71(9):3125-3127. doi:10.4103/IJO.IJO_2096_23 Rahman, Mir. New Era of Cornea Transplantation in Bangladesh. Transplantation 101():p S104, August 2017. | DOI: 10.1097/01.tp.0000525141.99931.bb.
Rahman, Mir. New Era of Cornea Transplantation in Bangladesh. Transplantation 101():p S104, August 2017. | DOI: 10.1097/01.tp.0000525141.99931.bb.