Journal of Veterinary Medicine And Science
OPEN ACCESS | Volume 3 - Issue 1 - 2026
ISSN No: 3065-7075 | Journal DOI: 10.61148/3065-7075/JVMS
Xavier Escoda1, Isaac Carrasco1,2*, Marta Martínez2, Annabel Dalmau3, Glòria Albinyana4
1Anicura Glòries Hospital Veterinari. Bailén 28, Barcelona, 08010, Spain.
2IVC Evidensia Canis Mallorca Hospital.Veterinario. Agnès de Pacs 12, Palma de Mallorca, 07010, Spain.
3Anicura Mediterrani Hospital Veterinari. Fusters 3, Reus, 43204, Spain.
4Citopat Veterinària. Provença 392, Barcelona, 08025, Spain.
*Corresponding author: Isaac Carrasco, Anicura Glòries Hospital Veterinari. Bailén 28, Barcelona, 08010, Spain. Email: icarrascorivero@gmail.com
Received: December 13, 2024
Accepted: December 18, 2024
Published: December 23, 2024
Citation: Escoda X, Carrasco I, Martínez M, Dalmau A, Albinyana G (2024) “Subcutaneous Panniculitis-Like T-Cell Lymphoma in Two Dogs with Indolent Progression, As A Clinical and Histopathological Form of Non-Epitheliotropic Lymphoma.” Journal of Veterinary Medicine and Science, 1(2); DOI: 10.61148/3065-7075/JVMS/017
Copyright: © 2024 Isaac Carrasco. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The subcutaneous panniculitis-like form of non-epitheliotropic T-cell lymphoma (SPTCL) has previously been described in dogs and is generally associated with poor prognosis. We describe two cases that showed a slow and benign progression, similar to the a-b T-cell phenotype without haemophagocytic syndrome form of the disease observed in humans. In contrast to the more aggressive g-d phenotype, the T-cells involved in this form of SPTCL in humans are CD30- and CD56-, as seen in the present cases, highlighting their potential as prognostic markers for a better outcome also in dogs.
Introduction
Cutaneous lymphoma accounts for approximately 5% of all canine lymphomas and can be broadly classified into non-epitheliotropic and epitheliotropic forms [1,2]. In dogs, the epitheliotropic form is more common than the non-epitheliotropic form (NECL), the latter are generally large cell lymphomas and have been classified into three subtypes: anaplastic large T-cell lymphoma, subcutaneous panniculitis-like T-cell lymphoma and peripheral T-cell lymphoma [2,3].
Nodules are present in almost all cases of NECL. These nodules are dermal or subcutaneous, firm, erythematous and alopecic, and pruritus is rarely seen. Arciform or serpiginous shapes are more common as cutaneous involvement in multicentric lymphomas and are rarely seen as isolated skin lesions [1].
Literature on the clinical management of non-epitheliotropic cutaneous lymphoma is scarce, but it has a guarded prognosis, with a median survival time of 4-9 months [1,2].
In this paper two cases of NECL with an unexpected benign progression and a clinical dermatological presentation consisting of nodular and/or arciform-serpiginous lesions involving the deep dermis and panniculus (compatible with the subcutaneous panniculitis-like form of NECL) are presented.
Case 1:
A - 7-year-old neutered mixed-breed dog was presented for evaluation of a six-month history of a dermatological problem that began as a single erythematous, alopecic, and non-pruritic nodule and developed into a larger arciform skin lesion in the sternal region (image 1).
The patient had been unsuccessfully treated with oral glucocorticoids, and no additional systemic pathological changes were evident.
Based on the appearance of the lesion, an initial differential diagnosis including allergic contact reaction, drug reaction, reactive cutaneous histiocytosis, papulo-nodular form of leishmaniosis, or neoplasia, such as mast cell tumour or lymphoma, was considered.
A cytological sample was obtained by using a fine-needle aspiration, which showed a large lymphocyte population after Diff-Quick® staining. (Image1)
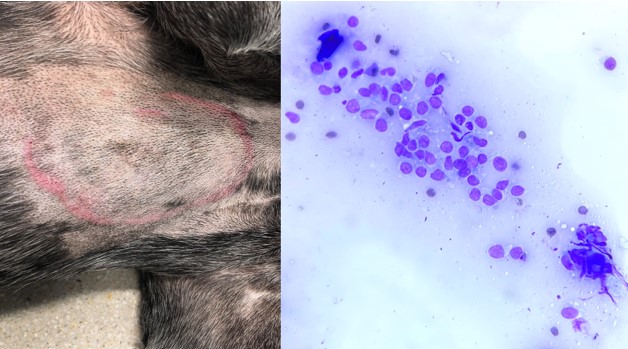
Image 1: Macroscopic appearance of lesions observed in case 1; and cytological findings after DiffQuick® staining of a sample taken using a fine needle.
Considering the cytological findings, tissue samples were taken for histopathological assessment using an 8 mm biopsy punch, which revealed infiltration of lymphocytic cells in the deep dermis and panniculus. Neoplastic lymphocytes had medium-sized nuclei that were densely stippled and occasionally had 1-2 prominent nucleoli with mild to moderate mitotic activity, accompanied by a mild or moderate numbers of histiocytes. (Image 2)
CD3 and PAX-5 stains were then performed, using polyclonal rabbit anti-human CD3 (DAKO, 1:100) and monoclonal mouse anti-human Pax5 (1EW), LEICA, RTU antibodies. More than 80% of the cell population examined was strongly positive for CD3, while less than 5% showed nuclear positivity for PAX-5, confirming a T-cell proliferation. (Image 2). In addition, a PCR test for antigen receptor rearrangements (PARR) confirmed a clonal proliferation of T-cells, supporting the diagnosis of non-epitheliotropic lymphoma.
Considering the diagnosis, complete blood work and staging with abdominal ultrasound (AUS) and thoracic x-rays were performed, all of which were unremarkable. Subsequently, a more extensive surgical approach was suggested to remove the solitary skin lesion.
Histopathological examination of the entire lesion revealed a malignant lymphocytic infiltration involving the panniculus and dermis was observed. There were no residual neoplastic cells near the margins of the sample, but some lymphatic vessels were affected. At this point, CD30 and CD56 staining were performed, using monoclonal mouse anti-human CD30 (JCM182), LEICA, RTU and monoclonal mouse anti-human CD56 (CD564), LEICA, RTU antibodies, and both were negative. (Image2)
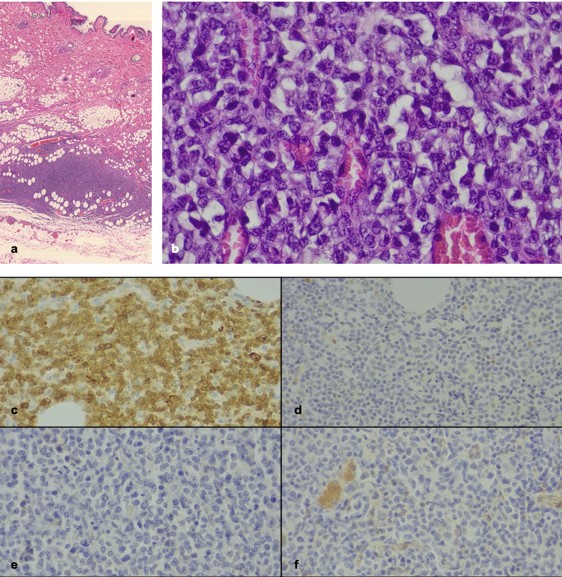
Image2: Histopathological study of biopsy samples in case 1; a. It is worth highlighting the strong cellular infiltrate that affects the panicle and respects the dermis and epidermis, b. Detail of the same preparation but at higher magnifications; c. CD3 staining positive; d. PAX-5 staining negative; e. CD30 staining negative; f. CD56 staining negative
Nonspecific treatment was administered in this case, and eighteen months after diagnosis the patient was alive and free of disease.
Case 2:
A 6-year-old golden retriever was presented with erythematous and non-pruritic skin nodules on the trunk of three weeks of evolution (Image 3). There was no evidence of systemic disease, and the dog had no history of any pathology to consider. In addition, no topical or systemics treatments had been administered for this condition.
Based on the appearance of the lesions, an initial differential diagnosis included nodular dermatoses of infectious origin, such as leishmaniasis; inflammatory conditions such as reactive histiocytosis; or neoplastic conditions, such as lymphoma and mastocytoma, was considered.
A cytological sample was then taken. After Diff-Quick® staining a large lymphocyte population with malignant changes was observed (Image 3).
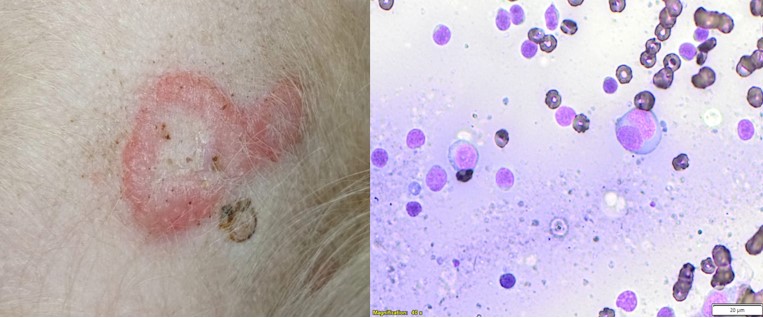
Image3: Macroscopic appearance of lesions observed in case 2, and cytological findings after DiffQuick® staining of a sample taken using a fine needle.
Multiple skin biopsy samples were then collected using an 8 mm biopsy punch. Histopathological evaluation revealed a multifocal dermatitis and panniculitis characterised by histiocytic infiltration with a proliferation of neoplastic lymphocytes. Neoplastic lymphocytes had medium-sized occasionally vesiculated nuclei that were densely punctate to hyperchromatic and occasionally had 1-2 prominent nucleoli and mild to moderate mitotic activity (Image 4).
CD3 and PAX-5 stainings were then performed, and more than 80% of the cell population examined was strongly positive to CD3, while less than 5% presented nuclear positivity to PAX-5, confirming that this was a T-cell proliferation (Image 4).
PARR was also performed in this case, but inconclusive results were obtained due to insufficient samples available for analysis. Despite this limitation, considering the absence of marked inflammation, which could mask neoplastic cell populations, and histomorphological features and immunophenotyping, non-epitheliotropic lymphoma remained the most probable diagnosis.In addition, both CD30 and CD56 staining were also negative in this case (Image4).
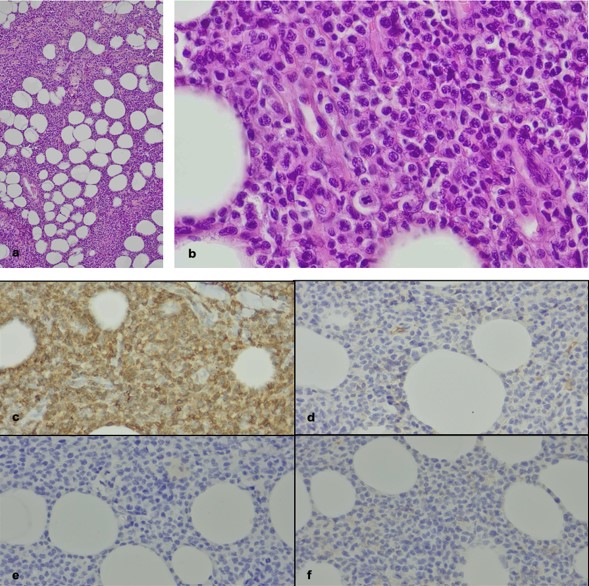
Image 4: Histopathological study of biopsy samples in case 2; a. A strong cellular infiltrate affects the panicle; b. Detail of the same preparation but at higher magnifications; c. CD3 staining positive; d. PAX-5 staining negative; e. CD30 staining negative; f. CD56 staining negative
A complete blood work, including Leishmania spp. serology, as well as staging with AUS and thoracic x-rays, were performed, with no abnormalities detected.
The lesions progressively disappeared within three weeks without any specific treatment, and eighteen months after diagnosis the patient was alive and free of disease.
Discussion:
In these two cases, we report a nodular and/or arciform mild-erythematous and non-pruritic form of subcutaneous panniculitis-like non-epitheliotropic T-cell lymphoma that was indolent, despite the guarded prognosis of the disease described in previous studies [1,2].
Given the clinical presentation, it is mandatory to rule out other diseases with a similar pattern but different therapeutic needs and prognosis, such as inflammatory or proliferative diseases, including panniculitis, reactive histiocytosis, or cutaneous benign lymphocytosis [4,5]. For this purpose, histopathological examination and specific immunohistochemistry are essential, although these can be challenging due to the frequent heavy infiltration of other inflammatory cells seen in some cases [6]
As mentioned above, cutaneous lymphocytosis would be a differential diagnosis given the benign course of the disease in the present cases. In humans, cutaneous pseudolymphoma (CPL) (or cutaneous lymphocytosis) has been described as a group of inflammatory lymphocytic disorders, either primary or secondary to stimuli such as drugs, trauma or contact dermatitis, that can mimic malignant lymphoma both clinically and histologically [7]. In contrast to lymphoma, lesions are usually self-limiting, and the involvement of other organs is rare, although progression to lymphoma has been reported [5].
Trauma or contact dermatitis cannot be completely ruled out as triggers of the disease, given the localisation of the lesions seen in the present cases. On the other hand, there was no reported history of drug use in the three months prior to the appearance of the lesions. However, considering the extensive list of drugs responsible for causing CPL in humans [7], the involvement of routinely used vaccines or antiparasitic drugs cannot be excluded in our cases.
In any case, in a case series of eight dogs with CPL the most common lesions observed were erythematous and alopecic macules and patches, and scaling, whereas nodules or plaques were not present in any of the dogs included [5]. In addition, the T-cell infiltrate rarely extends into the deeper dermis, unlike what was observed in the present cases, making this diagnosis less probable.
As in humans, a form of NECL named subcutaneous panniculitis-like T-cell lymphoma (SPTCL) has been described in dogs,6 presenting as solitary or multiple lesions. In this form, an infiltration of CD3+ T-cells affecting the subcutis without epitheliotropism is observed, often accompanied by a large population of histiocytic cells. This form of NECL is often indolent in humans, depending on the immunophenotype [3], in contrast to that observed in the case series reported by Noland et al., in which dogs included were euthanised 0.5-7 months post-diagnosis [6].
Given the histopathological and clinical outcome observed, these two cases may be considered similar to SPTCL reported in humans. However, not all cases of SPTCL exhibit a benign behavior in this species. The presence of concomitant haemophagocytic syndrome is considered a poor prognostic marker, and the a-b T-cell phenotype is associated with a better survival rate than g-d phenotype [3,6]. The a-b T-cell phenotype is characterised by negative CD30 and CD56 staining. Although this typing is not routinely performed in dogs, it was performed in the present cases and resulted in negative results for both CD30 and CD56 in both cases. Therefore, considering the outcome of our cases and the immunophenotyping results, we can hypothesise that these SPTCL cases were behave similarly to the a-b T-cell human phenotype without haemophagocytic syndrome.
There are few therapeutic recommendations for the treatment non-epitheliotropic lymphoma in dogs, and various treatment options and regimens have been used, ranging from prednisolone alone to various combinations of vincristine, doxorubicin, cyclophosphamide, chlorambucil, lomustine, melphalan and L-asparaginase [2]. As seen in a similar case report [8], surgical excision alone was sufficient to control the disease without further medication in the case 1. In contrast, in case 2 the lesions resolved spontaneously, and both patients were currently alive and disease free 18 months after the diagnosis.
SPTCL is a rare dermatological disease in dogs, with limited literature available. However, it should be considered in our differential diagnosis list for patients with compatible lesions. Although further studies involving a significant number of dogs are needed to draw definitive conclusions, we suggest that performing immunohistochemical staining for CD30 and CD56 on the biopsy sample may be useful in predicting the disease outcome in some cases.
This work was self-funded, and the authors have no conflict of interest to declare