Journal of International Research and Reviews
OPEN ACCESS | Volume 1 - Issue 1 - 2024
ISSN No: 3068-370X | Journal DOI: 10.61148/3068-370X/JIRR
Jason Semple
Prepared for The Following Course in A Doctor of Health Sciences Education Program College of Graduate Health Studies, A. T. Still University.
*Corresponding author: Jason Semple, Prepared for The Following Course in A Doctor of Health Sciences Education Program College of Graduate Health Studies, A. T. Still University.
Received: April 15, 2025
Accepted: May 25, 2025
Published: May 07, 2025
Citation: Jason Semple. (2025) “Preparing for Extubation and Multidisciplinary Rounds.” Journal of International Research and Reviews, 1(1); DOI: 10.61148/JIRR/002.
Copyright: © 2025 Jason Semple. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
In intensive care units (ICUs), patients receiving mechanical ventilation require coordinated efforts and timing across a multidisciplinary care team to gradually remove the ventilator from the patient, a process called ventilator weaning and extubation. The timeliness of the weaning process affects the patient's length of stay in the ICU and ICU bed availability for other patients admitted to the hospital. If patients are extubated later in the day, it is common for those patients to remain in the ICU for an additional day. An expedited approach to weaning and extubation has already proven safe and successful in post-surgical patients (Ellis et al., 2021). The goal of this continuous quality improvement initiative (CQI) is to facilitate timely weaning and extubation as a means to avoid unnecessarily prolonged duration of mechanical ventilation and ICU admission.
Causes of the Problem:
Early Morning Rounds:
Every morning, a multiple-disciplinary care team rounds on each patient in the ICU. During this time, the physician and many other care team members input orders and develop the care plan for the day. The physician is the one who is burdened with the most patients, so this is the most opportune and efficient time for him or her to assess a patient’s readiness to extubate and give approval. The issue that arises from this process is that the physician and care team round roughly one hour after the day-shift ICU staff arrive. Many patients are not ready for extubation when ICU rounds begin.
Status Quo:
The benefits of timely extubation have been well-established for both hospitals and individual patients (Holowachuk et al., 2019; Fernando et al., 2020; Zajic et al., 2023). Despite this knowledge, no clear process had been established to facilitate early extubation at this facility. The status quo had been to wait for the physician to round on mechanically ventilated patients, and then request that weaning attempts be made. If the ICU staff anticipated that the patient would be weaned, they could proactively begin weaning before the physician saw the patient, but that was not standard or expected.
Weaning and Extubation Timeframe:
The mechanical ventilation screening and weaning process often takes longer than one hour. Each patient that was determined to be ready to wean had to have both their sedation and ventilator settings weaned. The length of time required for that weaning is variable depending on the individual patient. Because of this time constraint, the ventilation screening and weening process would have to begin before the day-shift staff arrived. Night-shift staff had not been expected to routinely participate in the ventilator screening and weaning process, and because of this, they were less familiar with the process.
Negative Effects:
The negative effects on the patient were that if the patient was not ready to extubate until after the physician and care team had already rounded on them, there may be a considerable delay before the patient is extubated. This delay causes several immediate issues for the patient. First, the vent-weaning process can be very uncomfortable for patients. Second, the longer the patient remains on mechanical ventilation, the more problems such as ventilator-associated pneumonia and self-extubation are likely to arise (Wang et al., 2022). Lastly, delayed extubation may result in delayed patient discharge from the ICU. After extubation, patients need to be monitored before they can be safely moved out of the ICU and into a lower acuity care area.
The negative effects on the health organization are related to workflow and bed placement (Chan et al., 2018). If a patient that could have been extubated and discharged from the ICU earlier is delayed, they are unnecessarily using valuable hospital resources, ICU beds, and ICU staff that other patients may need. If the hospital has a relatively high census or most patients are high-acuity, not being able to discharge ICU patients in a safe and timely manner raises serious concerns for the well-being of patients who may be waiting to get into an ICU bed.
Stakeholders:
The intensive-care physicians are stakeholders because they are tasked with overseeing the appropriate care for the patients in the ICU. The day- and night-shift ICU staff are primary stakeholders because they are the ones tasked with performing ventilation screening and weaning in a safe and timely manner. The ICU staff most involved in those processes are nurses and respiratory therapists. Lastly, the hospital administrator is considered a stakeholder because he or she is tasked with attending to the day-to-day operations of the hospital which include bed placements both in and out of the ICU.
Solutions:
Begin Ventilator Weaning Earlier:
If the ventilator readiness to wean assessment and weaning process were started 30 minutes to 1 hour before day-shift staff arrived, it would be more feasible for the weaning process to be completed by the time the physician rounds in the ICU. This solution would require significant training for the night-shift staff. Since early extubation attempts are not already a standardized process at the facility, a standardized workflow and timeframe would need to be created. Sedation weaning will need to begin around the morning shift change so that ventilator weaning can begin shortly thereafter. This solution would allow for earlier extubation times and improve workflow in the ICU.
Begin Patient Rounds Later:
If ICU rounds began one hour later, it would be more feasible for the day-shift ICU staff to complete the entire ventilator weaning process before the rounds began. This would alleviate many of the current inefficiencies and workflow issues relating to planned extubations. Additionally, the duration of mechanical ventilation would be minimally prolonged by one hour compared to the other proposed solution to begin ventilator weaning earlier. However, every other task in the ICU that occurs after ICU rounds would be delayed. This delay would affect everything from scheduled procedures/surgeries to consultations, and additional assessments.
Prioritize Early Extubation Without Reforming Standard Procedures and Timeframes:
If ICU nurses and respiratory therapists prioritize early extubation, the average extubation time in the ICU would improve somewhat, but the patients are not likely to be ready for extubation by the time ICU rounds start. The expectation for early extubation without a standard procedure or timeframe would require a willingness from staff and a champion for the quality improvement initiative. This solution would reduce the duration of mechanical ventilation, but it would not eliminate inefficiencies in workflow.
Data Collection:
Selection of an appropriate data collection tool requires an accurate assessment of the problem and the proposed solution. As noted above, early weaning and extubation benefits are already well established. Therefore, a regression analysis that correlates extubation times with various patient benefits is unnecessary. The patient-specific bedside adjustments that encompass weaning are complex medical decisions that are outside the purview of this initiative. Therefore, a process flowchart would be inappropriate. The data collected should assess extubation times and duration of ICU stay, as well as common indicators of overly aggressive weaning such as re-intubation occurrences. An appropriate data collection tool would be to create a run chart for each of those measurements.
Overview, Background, and Theory:
A run chart is a simple tool that visually displays a measurement over time, which allows one to distinguish between causes of variation (Sollecito & Hardison, 2020). Whereas control charts focus on acceptable limits and variance, run charts focus on patterns over time. Figure 1, shown below, is an example of a run chart’s display of medication errors over time.
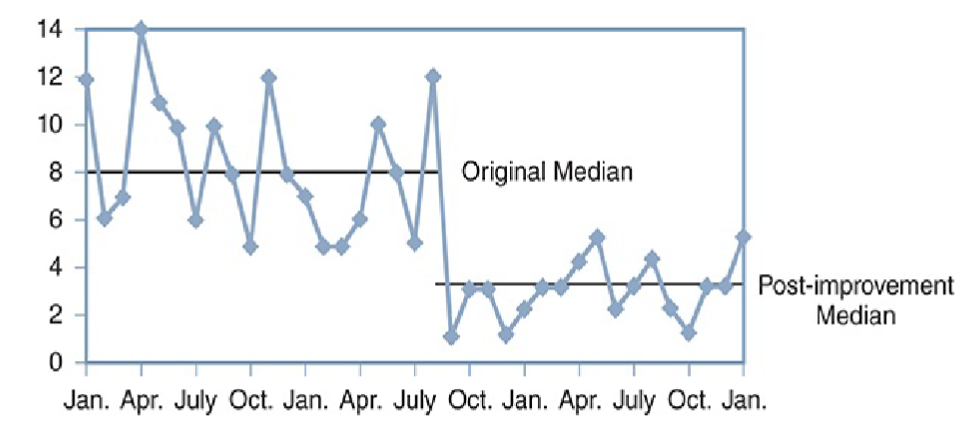
Figure 1: Run Chart of Number of Medication Errors
Note. Figure 4.3 from Sollecito & Hardison (2020, p. 272)
If a process change is made, and the measurement used in the run chart is believed to be affected by that change, then the run chart can be used to determine the effect of the process change. Conversely, if no process change was made, but the run chart’s measurements demonstrate considerable variance from an established norm, then an investigation may be made to determine the cause of the variance (Sollecito & Hardison, 2020).
Application, Strengths, and Limitations:
In the context of this quality improvement initiative, three measurements and run charts will be used as indicators of success:
average extubation time
length of ICU stay after extubation
re-intubation rates.
Baseline data before this initiative indicate that the average extubation time in the ICU averages between 1 p.m. and 2 p.m. After the process change is made to begin the weaning process earlier, the extubation time run chart will indicate the degree to which the extubation time can be affected. The length of ICU stay after the time of extubation will be included to measure the benefits of this process change. Since patients who are extubated later on in the day are typically observed overnight, the process changes to extubate sooner should correlate with drastically reduced lengths of ICU admission. Lastly, since the goal of this process change is to facilitate earlier extubation and potentially reduce the duration of observation in the ICU, negative effects such as re-intubation after extubation should be monitored in a separate run chart. An increase in reintubation rates would indicate the process change is negatively affecting patient outcomes.
The strengths of the run chart for this quality initiative are its ability to track measured data over time simply and visually. With an adequate amount of baseline data that the ICU has already been tracking, variances in extubation time, ICU length of stay, and reintubation rates should be easily identifiable. One major limitation to the use of run charts is that measured outliers may be recorded and considered as representative of the process change instead of as an outlier. Certain types of mechanically ventilated patients have skewed extubation times and do not have a traditionally normal weaning time frame. For example, many surgical patients are brought to the ICU, on ventilators, in the afternoon, with the expectation that those patients would be weaned and extubated that day. As such, these surgical patients would not be part of the process change, and their data should be excluded from the run charts. Since the hospital is already tracking the data used in the run charts via reports in the electronic health record, the data collection process only requires an individual to filter through the individual patients in those reports and screen for outliers or patients that should be excluded. To facilitate this screening, that individual should work with bedside staff to identify patients who should be excluded. This collaboration should require minimal staff training of roughly 30-60 minutes, as well as the formulation of an easy bedside screening tool that bedside staff can use to communicate with the data analyzer.
Conclusion:
Multidisciplinary care teams are necessary to provide for all of a patient’s intensive care needs. The CQI efforts to facilitate and expedite mechanical ventilation screening and weaning require multidisciplinary efforts from both day- and night-shift staff. Safe and timely ventilator weaning and extubation can reduce patient complications, reduce the length of admission, and improve bed placement and availability within the hospital. The solution to begin ventilator weaning earlier creates the most desirable outcome of facilitating early extubation and reducing inefficiencies in ICU workflow. The measured results that indicate the success of this initiative are early extubation times, decreased length of ICU admissions, and no increase in re-intubation rates.