International Surgery Case Reports
OPEN ACCESS | Volume 7 - Issue 3 - 2025
ISSN No: 2836-2845 | Journal DOI: 10.61148/2836-2845/ISCR
Victor Rogerio1, Amanda Brasil de Freitas1, Thiago Gomes Teixeira1, Pietra Roschel de Borba1, Viviane Rabelo1, Marcelo Germani3*, Victor R Munoz-Lora1,2
1Let's HOF Academy, São Paulo, Brazil.
2Department of Periodontology and Implantology, University of Guarulhos, São Paulo, Brazil.
3Department of Biological Sciences, Bauru School of Dentistry, University of São Paulo, Bauru, Brazil.
*Corresponding author: Marcelo Germani, Department of Biological Sciences, Bauru School of Dentistry, University of São Paulo, Bauru, Brazil.
Received: April 20, 2025
Accepted: April 26, 2025
Published: April 30, 2025
Citation: Rogerio V, Amanda Brasil de Freitas, Thiago G Teixeira, Pietra Roschel de Borba, Rabelo V, Marcelo Germani, Victor R Munoz-Lora. (2025) “A Multi-layer Forehead Rejuvenation with Hyaluronic Acid and Botulinum Toxin: A Case Report.”, International Surgery Case Reports, 7(1); DOI: 10.61148/2836-2845/ISCR/090
Copyright: © 2025. Marcelo Germani. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
The increasing demand for enhancing the quality and contour of forehead skin has revealed the limitations of standalone botulinum toxin (BTx) treatments for deep wrinkles. This report presents two cases where forehead rejuvenation was achieved using a combination of hyaluronic acid filler and BTx in a multi-layer approach. Patients received BTx injections prior to filler placement at supraperiosteal and subcutaneous levels. The technique involved deep bolus and retrograde cannula injections using appropriate safety measures. Thirty-day follow-up confirmed significant aesthetic improvement with minimal complications and high patient satisfaction. This combined approach should be considered a promising strategy for treating frontal deep wrinkles.
Introduction:
The growing demand to enhance the quality and contour of forehead skin has surged, driven by the limitations of standalone botulinum toxin (BTx) treatments, which may prove insufficient for effectively addressing deep wrinkles and depressions.
The predominant challenge in forehead procedures, aimed at restoring volume and structure, is the significant risk associated with potential blindness.1,2 Hyaluronic acid (HA) emerges as the most extensively employed and secure polymer for forehead treatment. However, comprehension of facial anatomy and adherence to key recommendations is crucial in this area.3–5 Here, we present two cases of safely addressing frontal deep wrinkles using a combination of BTx and HA gels.
Materials and Methods
Two male patients seeking treatment for deep forehead wrinkles underwent a comprehensive procedure. In both cases, abobotulinumtoxinA (Abo - Galderma,Upsala, Sweden) was administered 30 minutes prior to the forehead filling. HA was injected using a multi-layer approach (Figures 1 and 2). Initially, several 0.05 mL boluses of Restylane® (Q-Med AB, Galderma, Sweden) were strategically placed along the wrinkles in the supraperiosteal plane, utilizing a 29G ultra-thin wall needle positioned at 90 degrees. Each injection point involved a pinch maneuver, and a prior 10-second aspiration was performed. Then, Restylane Skinboosters® Vital (Q-Med AB, Galderma, Sweden) was distributed in the subcutaneous by retroinjections (0.1 – 0.2 mL per wrinkle), using a 22G cannula (TSK Laboratory Europe B.V., The Netherlands), with entry points positioned laterally to the wrinkles. This process was followed by digital accommodation with gentle pressure (Supplementary Information – digital content/video procedure: https://youtu.be/r7RtNTPIDMw). The procedures did not involve any pre- or post-operative medication, and only topical anesthesia was applied at puncture sites. Follow-up assessments, documented through photographic registers and stereophotogrammetry quantification (3D-LifeViz™ Quantificare) were conducted before, immediately after, and 30 days after the procedure.
Graphical Abstract – Forehead Rejuvenation Technique
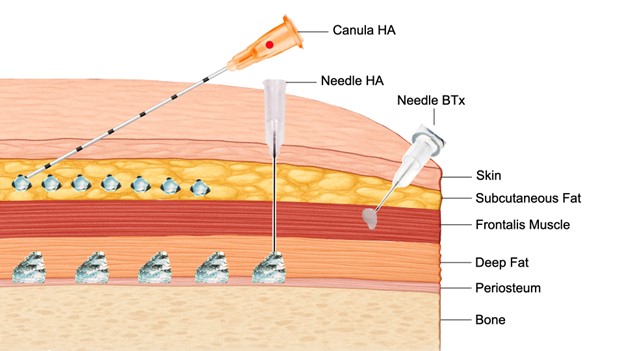
Graphical representation of a multi-layer forehead rejuvenation technique using botulinum toxin (BTx) and hyaluronic acid (HA). BTx is injected into the frontalis muscle to reduce dynamic lines. HA is delivered supraperiosteally with a needle for structural support and into the subcutaneous fat with a cannula to improve skin quality. This anatomical approach enables natural and harmonized results.
Case 1 (Figure 1): A 33-year-old male received a total of 195 speywood units (sU) of Abo. Thirty minutes later, 0.65 mL of Restylane® (Galderma, Upsala, Sweden) was injected supraperiostially, and 0.69 ml of Restylane Skinboosters® Vital were injected subcutaneoslly. Additionally, a HA treatment was also administered to address the tear trough and midface regions.
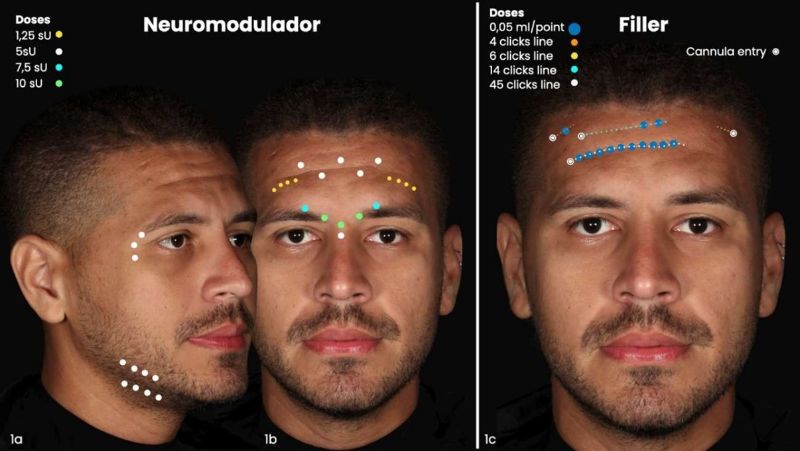
Figure 1: Case 1 methods description. (a and b) Schematic representation of botulinum toxin injection, (c) Schematic representation of filler injection.
Case 2 (Figure 2): A 32-year-old male received a total of 97.5 sU of Abo. Then, 0.2 mL of Restylane® were injected in the supraperiosteal region, and 0.1 mL of Restylane Skinboosters® Vital were injected subcutaneosly. Additionally, the tear trough and malar regions were also treated with HA.
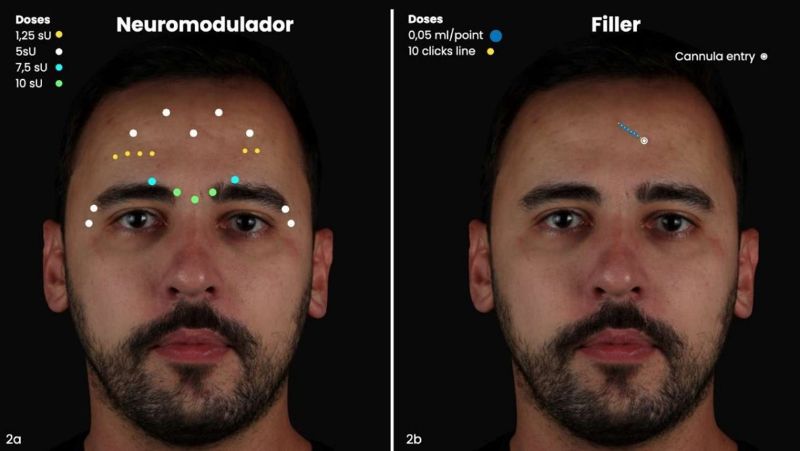 Figure 2: Case 2 methods description. (a) Schematic representation of botulinum toxin injection, (b) Schematic representation of filler injection.
Figure 2: Case 2 methods description. (a) Schematic representation of botulinum toxin injection, (b) Schematic representation of filler injection.
Results
Patients reported minimal pain and no complications, during and after the procedure. Transient erythema, edema, and some irregularities, were observed immediately after the procedure, and softened in the next few days. In the 30-day follow-up, a noticeable enhancement in depression and a smoother post-procedure contour, with minimal volume and natural appearance, were observed and confirmed by stereophotogrammetry assessment (Figures 3 and 4). In Case 1, there was an increase in forehead volume by 7.42 mL immediately post-treatment, attributed to injected products and procedure-related swelling. After 30 days, the depression marks became nearly imperceptible, and the forehead volume retain an increased by 1.58 mL compared to the pre-treatment state, indicating the resolution of the acute inflammatory response and a reduction in edema (Figure 3).
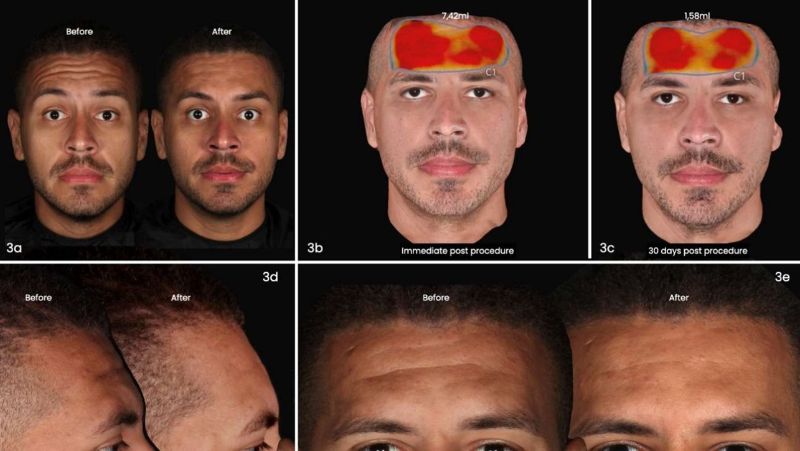
Figure 3: Case 1 outcomes (a) dynamic frontal photo 30 days post procedures, (b) stereophotogrammetry* right after the procedure, (c) stereophotogrammetry* 30 days post procedure, (d) static lateral photo 30 days after the procedure (d) static frontal photo 30 days after the procedure (* 3D-SQ LifeViz™ Quantificare)
In Case 2, there was an increase in forehead volume by 0.33 mL immediately post-treatment, attributed to injected products and procedure-related swelling. After 30 days, there was improved scarring, a smoother contour, and the forehead volume retain an increased by 0.17 mL compared to the pre-treatment state, indicating the resolution of the acute inflammatory response and a reduction in edema (Figure 4).
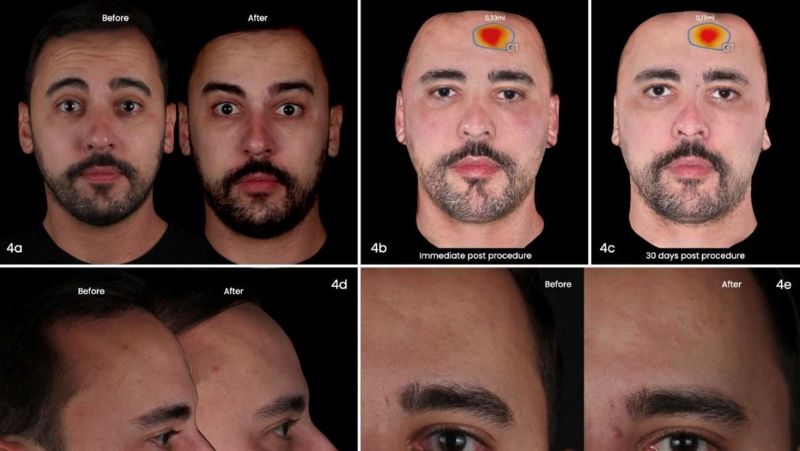
Figure 4: Case 2 outcomes. (a) dynamic frontal photo 30 days post procedures, (b) stereophotogrammetry* right after the procedure, (c) stereophotogrammetry* 30 days post procedure, (d) static lateral photo 30 days after the procedure (d) static frontal photo 30 days after the procedure (* 3D-SQ LifeViz™ Quantificare).
Discussion
A significant challenge for forehead procedures lies in the high risk of potential blindness due to the frontal branch of superficial temporal artery and its transversebranch, that runs on the superficial surface of the galea aponeurotica. In addition, the supraorbital and supratrochlear vessels are found deep in the lower one-third of the forehead and travels superficially on the upper two-thirds of the forehead.1,2 To mitigate this complication, a safety line was established located 2 cm above the orbital rim, opting for a needle just at deep planes to steer clear of vessels, injecting slowly and injecting with canula in the superficial layers.3–6 Additionally, we employ the pinch maneuver, to pull tissues upward (epidermis, dermis, superficial fat pads and aponeurosis), enhancing the available space within the loose areolar tissue and reducing the possibility of vascular and nerve injury during the procedure.5,7 Technically, the procedure was efficiently completed with minimal discomfort reported by patients. In certain areas, pinching was only achievable during needle entry. Maintaining the pinch proved challenging during supraperiosteal injection. The pinch for the cannula passing through the subcutaneous layer was comparatively more straightforward, with some resistance encountered. The increase in the volume immediately after the procedure was attributed to injected products but also to inflammatory response due to the trauma and procedure-related swelling. It may explain why the first case that received a total of 1.35 ml, 13 supraperiostal points of injection and 4 canula entry points showed a much higher increase in the volume right after the procedure compared to the second case that was injected a total of 0.3 ml, 4 supraperiostal points of injection and 1 canula entry point. HA offers notable advantages such as durability, biocompatibility, biodegradability, plasticity, and reversibility in case of patient dissatisfaction or complications. Given the unique characteristics of the thin frontal area, limited skin elasticity, minimal subcutaneous tissue, and a focus on achieving optimal tissue projection, Restylane® was deliberately selected due to its composition featuring small particles (330-430μm), a low swelling factor, elevated G', and notable lifting capacity.8 The injection technique involved deep microbolus injections to prevent irregular and visible marks. Restylane Skinboosters Vital was selected for the superficial layer for its composition featuring micro-particles (50-220μm), a medium to high G', and a low swelling factor.8 This choice aims to enhance skin quality and structure without significant volumizing, effectively minimizing the risk of irregularities.It's crucial to emphasize that the procedure was performed by a highly experienced injector. Additional studies are necessary to ensure the replicability and safety of this technique.
Conclusion
The combination of BTx and HA, employing in a multi-layer approach, yielded a satisfactory and safe aesthetic outcome for frontal filling, showcasing numerous benefits. This combination should be considered for addressing frontal deep wrinkles in clinical practice.
Acknowledgements
The authors thank the patients for their trust and the Let’s HOF Academy team for supporting the publication of this manuscript.
Conflict of Interest
Victor Rogerio, Viviane Rabelo and Marcelo Germani are speakers from Galderma; Thiago Gomes Teixeira is a speaker from Merz. The authors declare no conflict of interest regarding the publication of this manuscript.