International Surgery Case Reports
OPEN ACCESS | Volume 8 - Issue 1 - 2026
ISSN No: 2836-2845 | Journal DOI: 10.61148/2836-2845/ISCR
Samantha Esposito, BS1*, Claudia Perez, DO, FACOS2
1Rush Medical College, Rush University Medical Center.
2Division of Surgical Oncology, Rush University Medical Center.
*Corresponding Author: Samantha Esposito, BS Rush University Medical Center, 600 S Paulina St, Chicago, IL, 60612 USA.
Received Date: June 17, 2024
Accepted Date: June 24, 2024
Published Date: July 30, 2024
Citation: Esposito S, Perez C. (2024) “Rare Presentation of Pilomatrixoma as a Fungating Breast Mass.”, International Surgery Case Reports, 6(2); DOI: 10.61148/2836-2845/ISCR/077
Copyright: © 2024. Samantha Esposito. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Pilomatrixomas are rare tumors arising from the cellular matrix of hair follicles and manifest as subcutaneous nodules, most commonly of the head and neck region. This case report highlights a more rare presentation in the breast of a 68-year-old female, who presented with a protruding painful left breast mass. The mass underwent core biopsy and pathology confirmed a benign pilar cyst with keratin material. Over the next 2 months, the tumor exhibited progressive growth, resulting in skin fistulas and calcified material exuding from the skin. Her symptoms were further complicated by infection and progressive pain. After surgical excision, the final pathology revealed a benign pilomatrixoma of the breast. This case acknowledges the importance of timely diagnosis and surgical treatment of this rare tumor to prevent symptoms of tumor growth, erosion into the skin and secondary infection.
Introduction
A pilomatrixoma is a rare subcutaneous benign tumor originating from the cellular matrix of hair follicles.1 Clinically, these lesions present as superficial skin nodules that are firm and well-circumscribed.2 They are predominantly found in females and occur in the first and second decade of life, with few occurrences reported in the 5th and 6th decade.1-2
Only a handful of reports have documented pilomatrixomas arising from the breast tissue ranging from 3 mm to 30 mm in size.1 Because these lesions are rare, they are often first encountered on mammography masquerading as breast neoplasm requiring biopsy and eventually surgical excision.1,3 To our knowledge, there have been no reports of a breast pilomatrixoma that have fungated through the skin following core needle biopsy.
Case
A 68-year-old female presented to the Emergency Department (ED) for complaints of headache, back pain and urinary urgency. She had a Computed Tomography (CT) scan of the chest and was incidentally noted to have an enhancing 3.7 cm x 2.4 cm mass in the left inferior breast. A diagnostic breast ultrasound was recommended. She followed up with her primary care physician and by history she reported first noticing a small left breast mass several years prior. It was not bothersome, and she only recently noted a gradual increase in size. She denied tenderness to palpation or associated lymphadenopathy.
Diagnostic mammography and ultrasound revealed a large, oval, heterogeneous mass at the 7:00 position and 5 cm from the nipple, for which biopsy was recommended with BIRADS 4B rating and moderate suspicion for malignancy (Image 1).
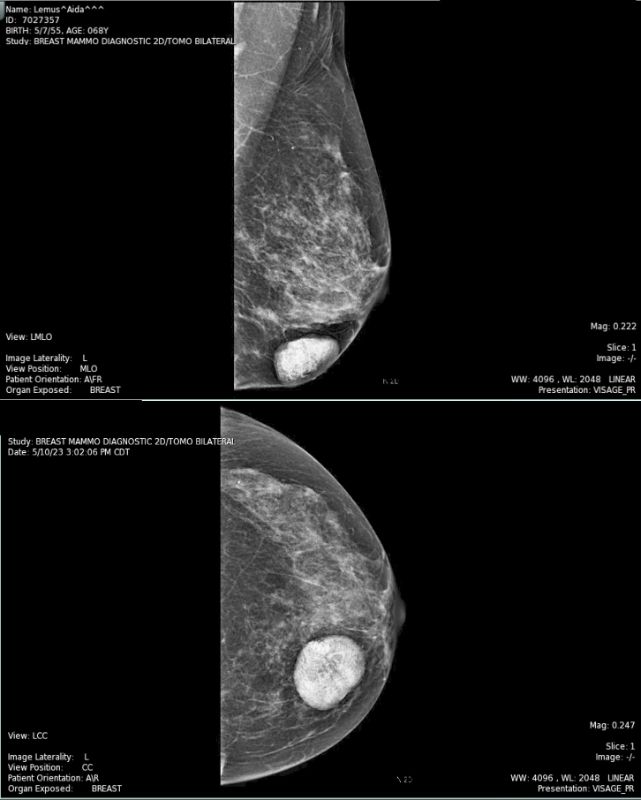
Image 1: Diagnostic Mammography of Left Breast A) Mediolateral view demonstrating well circumscribed calcified mass in the inferior location B) Craniocaudal view demonstrating the same mass in the medial aspect of the breast
The patient underwent ultrasound guided core biopsy, which revealed fragments of compact keratin material, suggestive of possible pilar cyst (Image 2).
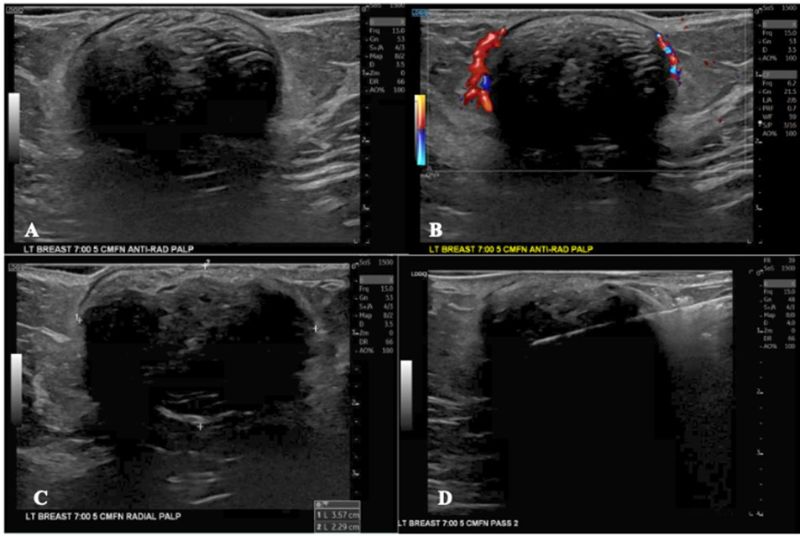
within the mass
Image 2: Ultrasound and Core Needle Biopsy A) Left breast mass at the 7 o’clock position, 5 cm from the nipple B) Doppler imaging without blood flow within the mass C) Mass measurements are 3.57 cm in width and 2.29 cm in height D) Demonstration of fine needle biopsy with needle
One month following the core biopsy, the patient reported worsening breast pain, swelling and drainage around biopsy skin site. On exam, the biopsy site was clean and well healed, however, there was spontaneous clear drainage through a cutaneous fistula adjacent to the biopsy site and appeared to communicate with the breast mass itself. Conservative management with clinical observations was recommended at that time, as there was no sign of abscess or infection.
The patient returned to the ED 2 weeks later with worsening breast pain, and now purulent drainage from skin opening requiring antibiotic therapy. On physical exam, the left breast was induratedwith erythematous and peeling skin. A calcified mass was noted in the lower inner breast, exuding from the skin. The cutaneous fistula was now a larger wound, with yellow fibrinous material (Image 3). An incision and drainage procedure was not performed as there was no evidence of a fluctuant abscess. She was treated with one dose of IV Cefazolin 2g/100mL and discharged home with Trimethoprim-Sulfamethoxazole for 7 days. The patient was counseled regarding the need for surgical excision given her symptoms and for definitive tissue diagnosis, however she declined at that time.

Image 3: Photograph from ED visit with fistulas and signs of purulent infection prior to treatment with 7 days of trimethoprim-sulfamethoxazole
The patient returned for follow up in the breast surgery clinic, with persistent pain and the palpable calcified mass. On exam, the skin was normal with no erythema, and the mass, with a calcified component eroding through the skin measured 4 cm in the lower inner breast (Image 4).
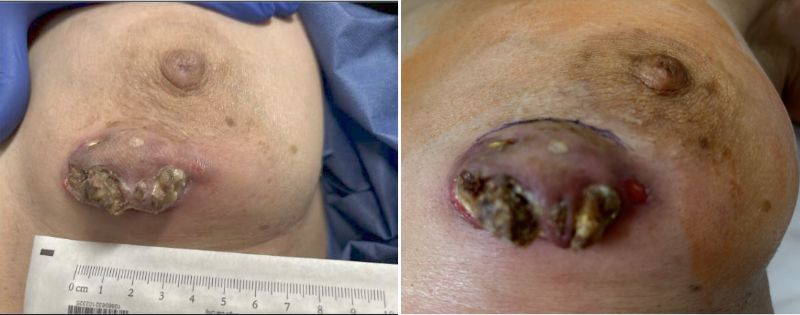
Image 4: Pre-operative photograph of mass with fistulas and expressing calcified material. Measuring 2.5x4.5 cm
After discussion, the patient agreed to surgical excision. The patient underwent left breast lumpectomy, at which time the entire mass and overlying affected skin was excised (Image 5).

Image 5: Left breast mass following lumpectomy A) Kubtech image specimen image with biopsy clip measuring 4.5 cm x 5.8 cm x 2.2 cm B) Gross image of lumpectomy specimen with skin area measuring 5.2 cm x 2.4 cm with central defect measuring 4.0 cm x 1.5 cm
The final pathology revealed a benign cystic pilomatrixoma measuring 3.5 cm with a central calcified defect in the skin (Images 6-9). There was no evidence of carcinoma. The mass was excised in its entirety. The patient returned 1 week later for post-operative exam and was healing well without complaints.
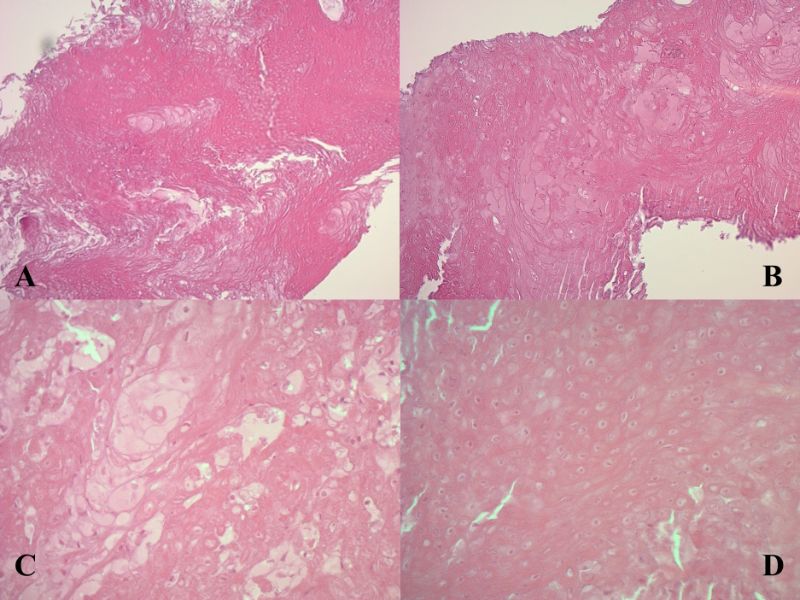 Image 6: Anucleated ghost (shadow) cells at various magnifications (A – 10x; B – 20x; C and D – 40x)
Image 6: Anucleated ghost (shadow) cells at various magnifications (A – 10x; B – 20x; C and D – 40x)
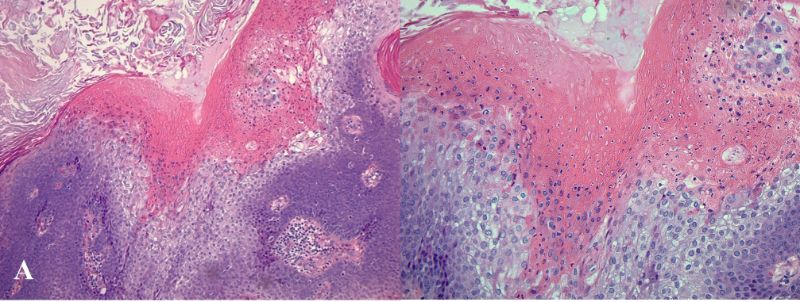
Image 7: Basaloid cells transforming into ghost (shadow) cells without granular layer (A – 10x magnification; B – 20x magnification)
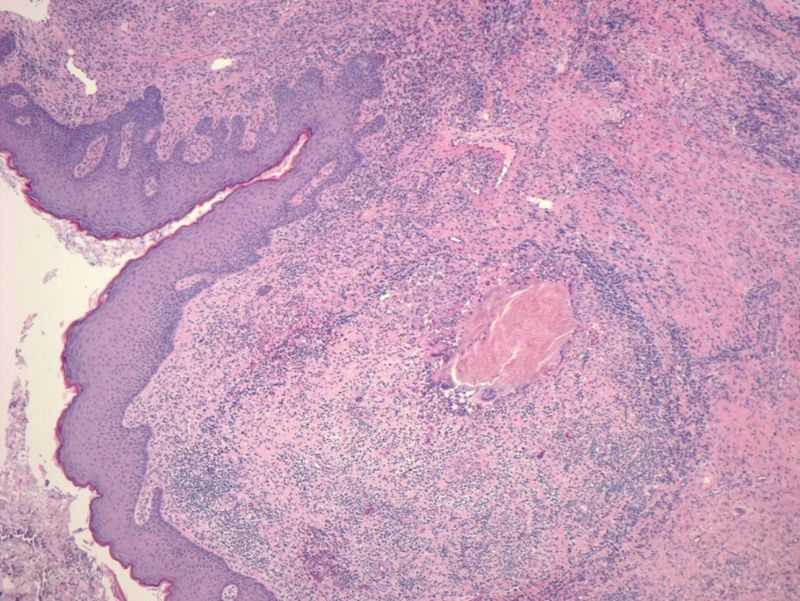 Image 8: Intact epidermis with dermal tumor composed of mixed cell types (4x)
Image 8: Intact epidermis with dermal tumor composed of mixed cell types (4x)
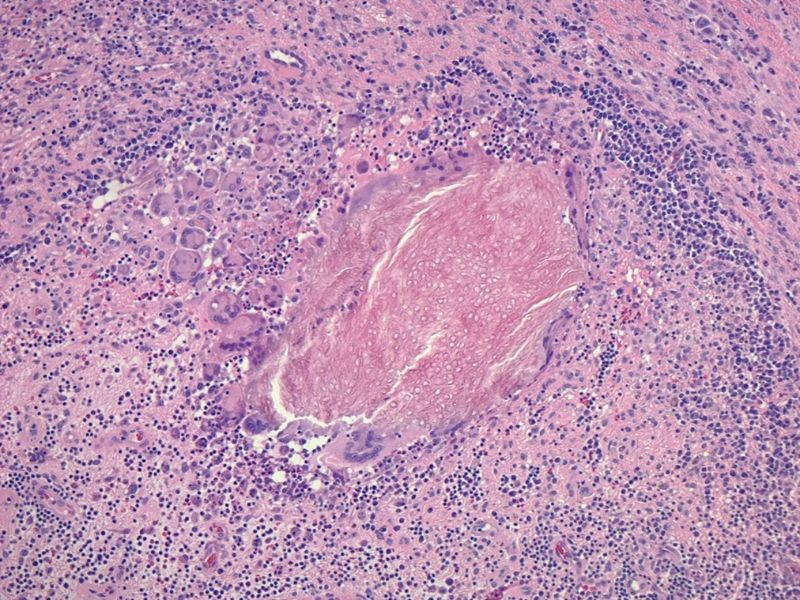 Image 9: Nest of anucleated ghost (shadow) cells with inflammation and foreign giant cells in the stroma (10x)
Image 9: Nest of anucleated ghost (shadow) cells with inflammation and foreign giant cells in the stroma (10x)
Discussion
Although pilomatrixomas are rarely found in the breast, this diagnosis should be considered when evaluating patients that present with a palpable breast mass, at all ages.1-2 Pilomatrixomas are likely caused by an inflammatory response precipitating overgrowth in the hair follicle matrix.1 In the breast specifically, these masses are thought to originate from peri-areolar piliferous bulbs.1 As evident in our review of case reports, a breast pilomatrixoma commonly presents with a firm, palpable mass below the skin surface at various depths, usually painless at initial presentation, and slow growing.3-4 The differential diagnosis is broad including fibrocystic changes, papilloma, calcified fibroadenoma, fat necrosis, or invasive carcinoma. This tumor is most often seen on mammography and ultrasound, and can mimic a mass of malignancy. Table 1 reports known cases of pilomatrixomas of the breast that have been reported in the literature thus far.
|
Reference # |
Sex |
Age |
Presenting Symptoms |
Location & Imaging Details |
Treatment |
Other notes |
|
1 |
M |
53 |
Pea-sized lump in right breast near nipple that was first noticed 3 months earlier |
Medial right breast |
Surgical excision |
|
|
3 |
F |
33 |
Palpable and painless nodule in left breast for 2 years |
lower outer quadrant of left breast |
Treatment not reported |
BIRADs IV |
|
4 |
F |
55 |
Superficial lump in a subcutaneous location |
Axillary tail of left breast |
Surgical excision |
|
|
7 |
M |
56 |
Slow growing, firm lump |
Left breast at 9 o’clock, 12 cm from the nipple. Circumscribed mass within superficial subcutaneous fat, abutting the skin undersurface. 1.8 cm inseparable from skin surface |
Treatment not reported |
|
|
8 |
M |
48 |
Left breast lump for 2 months |
Lower outer quadrant of left breast. 5x3x2 cm |
Surgical excision |
BIRADs II |
|
9 |
M |
48 |
Progressively enlarging, painless lump in left breast for 3 months with normal overlying skin |
Periareolar region at the 6–7 o'clock position in the subcutaneous tissues of the left breast. Well-defined oval, hypoechoic solid mass measuring 1.0 × 0.8 cm |
Surgical excision |
BIRADSs IVA |
|
10 |
F |
13 |
Palpable lump in left breast that first appeared as small erythematous papule 3 months prior. Gradually enlarged with bluish discoloration |
Lower outer left breast 2cm in diameter |
Surgical excision |
|
|
11 |
M |
51 |
Swelling of the left breast for 6 months |
Two o’clock position in the periareolar region of the right breast attached to unremarkable skin. Measuring 1.6 × 1.0 cm |
Surgical excision |
|
|
12 |
M |
43 |
Painless enlarging breast mass for one year |
Inferomedial mass in subcutaneous location of left breast measuring 3 cm with blue discoloration of skin |
Surgical excision |
BIRADs IV |
|
13 |
M |
36 |
Palpable pea-size lump in left breast that increased in size over last 6 months |
Upper outer quadrant of the left breast parallel to the skin and chest well measuring 1.0 cm × 0.8 cm × 0.6 cm |
Surgical excision recommended, but not completed |
BIRADs IVb |
|
14 |
M |
65 |
Painless lump in right breast noted to be growing bigger over the last 3 years |
Upper inner quad of righ breast extending to anterior chest wall measuring 12 cm with discolored overlying skin without ulceration |
Surgical excision |
Too firm to biopsy |
|
15 |
F |
43 |
Nontender breast lump that was firm in the deep layers of the breast |
Periareolar area at the confluence of the outer quadrant of the left breast measuring 12x11 mm |
Surgical excision |
BIRADs IV-V |
|
16 |
M |
58 |
Palpable, painless nodule in left breast for 4 years |
Upper outer quadrant left breast located 0.4 cm from surface |
Surgical excision |
Table 1: Previously reported pilomatrixoma of the breast
Current diagnostic and treatment recommendations include ultrasound guided biopsy of the mass followed by excision. On ultrasound, the mass appears hyperechoic or isoechoic with a peripheral halo and a posterior shadow (Image 2).5 The mainstay of treatment is surgical excision regardless of location in the body, however, since this tumor is exceedingly rare in the breast, there is no current consensus on margins or technique.5 CT scans have not been reported to be used for diagnosis, and in the current case, did not provide any additional diagnostic information.
Pilomatrixomas can be challenging to diagnose due to the variation histologically. There are four stages of pilomatrixomas including the early stage, with small cystic lesions composed of shadow cells originating from a faulty hair matrix; the fully developed stage, with rapid tumor growth as a foreign body reaction to the exposed shadow cells, usually from inflammation or trauma; the early regressive stage, demonstrating granulation tissue surrounding the shadow cells; and the late regressive stage, characterized by calcification, ossification, and desmoplastic stroma replacing granulation tissue (Image 9).6
In our patient’s case, the initial biopsy demonstrated a pilar cyst, likely representing the early stage of pilomatrixoma. As these tumors grow, it has been reported that the shadow cells provoke a foreign body reaction allowing for containment of the aberrant keratinization.6 In cases that did not report skin protrusion, the histological findings represented the early stage of pilomatrixomas characterized by limited tumor proliferation.3
We note that the overall time from biopsy to surgical removal was prolonged in this case, therefore allowing the tumor to progress. It is possible that the trauma caused by biopsy, allowed for shadow cells to evade the foreign body reaction instigating rapid growth of the tumor. When the foreign body reaction is not adequate in containing the shadow cells, calcification or ossification can occur to contain the proliferation.6 This phenomenon was noted in this case of breast pilomatrixoma, as it created cutaneous fistulas expressing calcified material.
This case supports the current clinical management of breast pilomatrixomas through ultrasound guided core biopsy, followed by wide local excision. We encourage timely excision of a palpable mass proven to be pilar cysts or pilomatrixomas to avoid possible erosion of calcified tissue through the skin which can be complicated by infection and need for larger excision, as evident in our case.
Conclusion
Breast pilomatrixoma is exceedingly rare and can masquerade as malignant neoplasm. Mammogram and ultrasound are the gold standard imaging to evaluate this type of mass. Although biopsy is imperative for definitive diagnosis, we highlight the clinical changes that can occur after trauma from biopsy. This case emphasizes the importance of timely excision of the mass, to prevent fungating or erosion through the skin, increasing risk for infection and possible need for more extensive surgical excision.
Author Contributions: Samantha Esposito conducted a literature search, wrote the original draft of the case report, and edited and labeled the figures. Dr. Claudia Perez assisted with writing the original draft and edited the final case report.
Funding: There is no funding for this case report
Conflicts Of Interest: There are no conflicts of interest to disclose.