International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 5 - Issue 1 - 2025
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
Anumita Mallick1, Sandip Sarkar2, Sanzida Shams3, Prakash C. Dhara4, Tamjida Hanfi5, Shafi U. Bhuiyan6, 7*
1Department of Nutrition, Belda College, and Research Scholar, Vidyasagar University, India.
2Department of Mathematics, Bethun College, West Bengal, India.
3Department of Health Research Methods, Evidence, and Impact (HEI), McMaster University.
4Directorate of Distance Education, Ex Professor, Vidyasagar University.
5Faculty of Public Health, Mahidol University, Thailand.
6School of Public Health, University of Memphis, TN, USA
7Dalla Lana School of Public Health, University of Toronto, Canada.
*Corresponding author: Shafi Bhuiyan, PhD, MBBS, MPH, MBA
School of Public Health, University of Memphis, TN, USA.
Received: June 20, 2025 | Accepted: June 30, 2025 | Published: July 21, 2025
Citation: Mallick A, Sarkar S, Shams S, Prakash C. Dhara, Hanfi T, Shafi U. Bhuiyan. (2025) “From Stigma to Self-Care: Addressing Menstrual Health Challenges Among Rural Girls in West Bengal, India”. International Journal of Epidemiology and Public Health Research, 6(5); DOI: 10.61148/2836-2810/IJEPHR/156.
Copyright: © 2025. Shafi U. Bhuiyan. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited., provided the original work is properly cited.
Menstruation represents a fundamental physiological milestone in the lives of adolescent girls; however, it continues to be a stigmatized and inadequately addressed aspect of reproductive health, particularly in the rural areas of the Midnapore district in West Bengal. The present study was conducted to evaluate key parameters associated with menstrual health, specifically the age of onset of menarche, duration and nature of menstrual flow, prevalence of premenstrual symptoms, menstrual hygiene practices, and the regularity of menstrual cycles among adolescent girls residing in rural settings. A total of 232 participants were surveyed, revealing a mean age at menarche of 12.7 years (with an observed range between 12.3 and 12.9 years). While most respondents reported regular menstrual cycles and flow durations within the normative range, a considerable proportion experienced a spectrum of distressing physical symptoms. It continued to adopt suboptimal hygiene practices, including the use of improvised absorbents. These findings underscore the urgent need for comprehensive menstrual health education, coupled with enhanced accessibility to affordable and hygienic menstrual products, to promote menstrual well- being and dignity among rural adolescent populations.
Literature Review
Menstruation, a biological hallmark of female puberty, is often enshrouded in silence and misconceptions, particularly in developing countries. Despite being a natural physiological process, menstruation remains inadequately discussed due to persistent cultural taboos, stigma, and insufficient reproductive health education. These issues are especially acute among adolescent girls in rural India, where healthcare access, hygienic products, and accurate menstrual knowledge remain limited.
Age of Menarche and Menstrual Patterns
Age at menarche varies significantly among populations, influenced by genetic, nutritional, and environmental factors. The National Family Health Survey-5 (NFHS-5, 2020–21) reports that Indian girls typically attain menarche between ages 12 and 14, with rural girls often experiencing delays attributed to undernutrition and chronic illnesses. For instance, Patil et al.
(2014) reported a mean age of 13.4 years among rural schoolgirls in Maharashtra, noticeably delayed compared to urban areas. Delayed or early menarche significantly impacts physical and mental health, necessitating targeted health interventions (Chandra-Mouli et al., 2017).
Menstrual Symptoms and Health Complications
Menstrual symptoms such as dysmenorrhea (painful menstruation), backache, fatigue, and emotional disturbances are common yet widely neglected. Over 70% of adolescent girls studied by Ahuja and Tewari (1995) reported moderate-to-severe menstrual pain, yet fewer than 15% sought medical help. Such symptoms have a direct impact on school attendance, concentration, and academic performance, particularly among rural communities (Rigon et al., 2012).
Premenstrual Syndrome (PMS) and Mental Health Premenstrual symptoms, frequently underreported due to normalization of menstrual suffering, significantly impact adolescents' mental health. Adolescents experiencing PMS show increased susceptibility to anxiety, irritability, and depressive episodes, which caregivers and educators often overlook (Balaha et al., 2010). Effective school-based mental health programs linking menstrual health to psychological well-being remain essential (Shiferaw et al., 2014).
Menstrual Hygiene Management (MHM)
The use of sanitary products varies considerably across regions, influenced significantly by geography, socioeconomic status, and cultural practices. A recent report by NFHS-5 (2021) noted significant improvements in sanitary napkin usage nationally; however, substantial disparities persist, especially in rural areas. Garg and Anand (2015) identified inadequate access to hygienic menstrual products as a leading cause of urogenital infections among adolescent girls. Previously, Khanna et al. (2005) reported harmful practices such as using ash, husk sand, and dirty rags, resulting in reproductive tract infections (RTIs). Moreover, Balamurugan and Bendigeri (2012) emphasized that over half of adolescent girls in Karnataka relied on old clothes, frequently reused without proper sterilization, highlighting inadequate sanitation facilities in rural schools as a key barrier to hygienic practices.
Knowledge, Awareness, and Sources of Information
Girls frequently approach menarche with minimal or no prior understanding, exacerbating their vulnerability. Verma et al. (2020) reported that over 60% of adolescent girls in Uttar Pradesh had no menstrual awareness at menarche. Often, mothers serve as primary sources of menstrual knowledge but themselves lack accurate information, perpetuating misconceptions (Narayan et al., 2001). Dhingra et al. (2009) noted that 83% of girls in Jammu received no formal menstrual education, often viewing menstruation negatively, either as a disease or punishment. These findings underscore the urgent need for structured, curriculum- based menstrual education integrated into the school system.
Cultural Taboos and Restrictions
Cultural taboos substantially affect adolescent girls' menstrual experiences, contributing to significant psychological distress. Chikarmane (2015) described restrictions in Indian communities such as exclusion from religious activities, cooking, and attending school during menstruation, reinforcing shame and isolation. Mahon and Fernandes (2010) documented school absenteeism in rural Tamil Nadu, attributed to inadequate toilet facilities, disposal challenges, and stigma associated with menstrual staining, thus reinforcing long-term educational setbacks.
Menstrual Cycle Regularity and Medical Neglect
Irregular menstruation, typical in initial years after menarche, can also signal underlying health concerns like polycystic ovarian syndrome (PCOS) or thyroid dysfunction. Sharma et al. (2013) observed that many rural adolescents viewed irregular menstruation as "normal" and seldom sought medical attention, highlighting significant gaps in awareness and accessibility to adolescent-friendly health services in rural settings.
Global Perspectives and Policy Interventions
Globally, menstrual health management (MHM) is increasingly recognized as a critical component of adolescent well-being, explicitly addressed within the UN Sustainable Development Goals—Goal 3 (Good Health and Well-being) and Goal 5 (Gender Equality). India's Rashtriya Kishor Swasthya Karyakram (RKSK) and Menstrual Hygiene Scheme (MHS) exemplify policy efforts aiming to improve MHM through education, sanitary napkin provision, and adolescent-friendly health services. However, the impact of such programs remains uneven, especially in remote rural areas, highlighting the need for region-specific implementation strategies.
Synthesis and Research Gap
Although substantial literature addresses menstruation-related challenges among rural adolescents in India, gaps persist concerning the intersection of menstrual health with emotional well-being, educational impact, and infrastructural inadequacies. Furthermore, literature specifically addressing the Midnapore district is notably sparse, despite the unique cultural and geographical attributes of this region. This highlights the need for focused, region-specific studies that incorporate both qualitative and quantitative methodologies to generate actionable insights into menstrual health management practices.
Menstruation is a fundamental physiological process signifying reproductive maturity in females, marking a crucial phase in pubertal development and serving as an indicator of reproductive and hormonal health. Despite being a natural biological phenomenon, menstruation continues to be misunderstood and stigmatized, particularly in low- and middle-income countries such as India. Socio-cultural taboos, religious prohibitions, gender- based discrimination, and generational silence contribute significantly to misinformation and discomfort surrounding menstruation (Garg & Anand, 2015; Chikarmane, 2015).
In rural India, these issues are exacerbated by limited access to menstrual health education, inadequate sanitation infrastructure, unaffordable sanitary products, and deficient healthcare services. Consequently, adolescent girls frequently enter menarche unprepared and unsupported, leading to inadequate hygienic menstrual management practices. This lack of preparedness adversely impacts their physical and mental health, educational attendance, self-esteem, and overall life quality, and increases the risk of reproductive tract infections (RTIs) and chronic gynecological conditions (Khanna et al., 2005; Mahon & Fernandes, 2010).
Studies consistently indicate that rural adolescent girls commonly resort to traditional or unhygienic methods—such as old cloths, rags, or unsafe absorbents—due to economic constraints and social pressures. Moreover, societal normalization of menstrual pain and discomfort discourages adolescents from seeking medical attention or emotional support, leading to prolonged health complications and psychological distress (Balaha et al., 2010; Sharma et al., 2013).
Given these conditions, there is an urgent need to examine menstrual health in context-specific settings comprehensively. This study aims to explore various dimensions of menstrual health among rural adolescent girls, focusing explicitly on age at menarche, menstrual cycle duration and regularity, menstrual and premenstrual symptoms, and menstrual hygiene management practices. By identifying key patterns and gaps in menstrual health awareness and management practices, the study aims to inform the development of targeted educational, medical, and culturally sensitive policy interventions for rural adolescent girls in India.
This study aims to critically investigate menstrual health and hygiene practices among adolescent girls residing in rural regions. Specifically, the study seeks to:
These articulated objectives aim to generate comprehensive, context-specific insights that inform future interventions and policies designed to enhance menstrual health and overall well- being among rural adolescent girls.
This study employed a cross-sectional descriptive research design to assess various aspects of menstrual health among adolescent girls residing in rural areas. A total of 232 participants, aged 10–16 years and having experienced menarche, were selected through purposive sampling, a method justified by the need to include respondents specifically meeting defined inclusion criteria relevant to rural adolescent menstrual health research (WHO, 2020).
Data collection employed a pre-tested and structured questionnaire designed to gather comprehensive and reliable information on menstrual health and hygiene practices. The questionnaire covered the following domains:
Ethical approval and informed consent were obtained prior to the commencement of data collection. For participants under 16 years of age, parental or guardian consent was obtained. Confidentiality and anonymity were strictly maintained.
Descriptive statistical analyses, including frequencies, percentages, and measures of central tendency, were applied to identify patterns and prevalent menstrual health issues within the studied population.
The average age at menarche among the surveyed girls was 12.7 years, with a range of 12.3 to 12.9 years. A notable proportion (22.84%) reported delayed menarche at 16 years. Other reported ages were 15 years (19.40%), 14 years (18.97%), 13 years (18.10%), and 12 years (20.69%) (Table 1).
Table 1: Distribution of Age at Menarche among Rural Adolescent Girls (n=232)
|
Age at Menarche (years) |
No. of samples(n) |
Percentage (%) |
|
12 |
48 |
20.69 |
|
13 |
42 |
18.10 |
|
14 |
44 |
18.97 |
|
15 |
45 |
19.40 |
|
16 |
53 |
22.84 |
|
Total |
232 |
100 |
These variations align with previous research, which highlights nutrition, socioeconomic status, geographic location, and genetic factors as influencing menarche timing (Ameade & Garti, 2016; Meng & Duan, 2017). For example, overweight and obese girls reach menarche earlier than their typical-weight peers (Meng & Duan, 2017; Shaw et al., 1977), and girls from urban or higher-income backgrounds tend to attain menarche sooner than those in rural or lower-income settings (Ameade& Garti, 2016; Meng & Duan, 2017).
The menstrual duration among participants predominantly ranged from 3 to 5 days (56.47%), with fewer reporting longer durations (23.28% for 6–7 days, 9.48% for >7 days) or shorter durations (10.77% for <3 days) (Table 2).
Table 2: Duration of Menstrual Bleeding among Participants(n=232)
|
Days of the menstrual cycle |
Number of samples (n) |
Percentage (%) |
|
<3 |
25 |
10.77 |
|
3-5 |
131 |
56.47 |
|
6-7 |
54 |
23.28 |
|
>7 |
22 |
9.48 |
These results fall within the expected adolescent range, although a minority of girls report prolonged bleeding that may warrant medical evaluation. Early post-menarcheal cycles are often anovulatory and irregular, with most initial menses lasting 2–7 days (Flug et al., 1984; Widholm et al., 1971). Approximately 90% of cycles occur within 21–45 days during the first two years after menarche (WHO, 1986), and by the third post-menarcheal year, 60–80% of cycles normalize to 21–34-day intervals typical of adult menstruation (Widholm et al., 1971; WHO, 1986; Hickey & Balen, 2003).
Multiple menstrual symptoms were prevalent among participants, notably abdominal pain (76.29%), cramps (24.57%), general discomfort (9.91%), and backache (8.62%) (Table 3).
|
Menstrual symptoms |
Number of samples (n) |
Percentage (%) |
|
Abdominal pain |
177 |
76.29 |
|
Cramp |
57 |
24.57 |
|
Uncomfortable |
23 |
9.91 |
|
Backache |
20 |
8.62 |
|
Body ache |
7 |
3.02 |
|
Headache |
11 |
4.74 |
|
Irritability |
6 |
2.59 |
|
Depression |
5 |
2.16 |
|
No symptoms |
12 |
5.17 |
|
Multiple symptoms |
232 |
100 |
Table 3: Prevalence of Menstrual Symptoms in Rural Adolescents(n=232)
This high prevalence of menstrual discomfort underscores the urgent need for education on effective pain management. Dysmenorrhea usually begins 1–2 days before bleeding and lasts 2–4 days, manifesting as lower abdominal and back cramps. Primary dysmenorrhea results from uterine prostaglandin release, whereas secondary dysmenorrhea stems from conditions such as endometriosis or fibroids (O’Connell, 2006). Emotional stress can amplify cramps, which are often accompanied by nausea, headache, dizziness, and sweating. Non-pharmacological remedies reported include rest, heat application, and herbal teas (e.g., fennel, ginger, cinnamon). Pharmacological approaches were likewise common: most girls used at least one analgesic, 31% used two, and 15% used three medications—often at sub-therapeutic doses—yet few sought formal medical care (O’Connell, 2006).
Hygiene practices varied widely among the girls. Approximately 39.66% used sanitary pads, while 19.83% used new cloth, 29.74% used old cloth, and 10.78% reported using all types interchangeably (Table 4).
Table 4: Types of Menstrual Absorbents Used by Participants(n=232)
|
Type of Napkin Used |
Number of samples (n) |
Percentage (%) |
|
Sanitary pads |
92 |
39.66 |
|
New cloths |
46 |
19.83 |
|
Old cloths |
69 |
29.74 |
|
All |
25 |
10.78 |
|
Total |
232 |
100 |
The low uptake of commercial sanitary products and extensive reuse of cloth-based alternatives mirror rural patterns documented elsewhere: in two North Indian villages, only 0.4% of women used market-purchased pads, 51.25% lacked awareness of sanitary pads, 11.25% used pads exclusively, 42.5% relied on old cloths, 6.25% on new cloths, 40% on both, and 73.75% reused cloths (Rajagopal & Mathur, 2017). Similarly, 66% of rural Nepalese schoolgirls reported using reusable cloths (Garg et al., 2012). These statistics underscore the urgent need for affordable product distribution and menstrual hygiene education to reduce infection risks and promote dignity and respect.
Regular menstrual cycles were reported by 67.24% of respondents, while 32.76% experienced irregular cycles (Table 5). Irregular menstruation can result from hormonal imbalances, nutritional deficiencies, or stress, necessitating further medical evaluation. A normal menstrual cycle spans 21–35 days with bleeding lasting 2– 7 days (total blood loss 30–80 mL), and any interval exceeding three months between cycles is classified as a missed cycle (Patil et al., 2009).
Table 5: Regularity versus Irregularity of Menstrual Cycles
This highlights the need for regular health screenings to manage and address menstrual irregularities effectively (Patil et al., 2009).
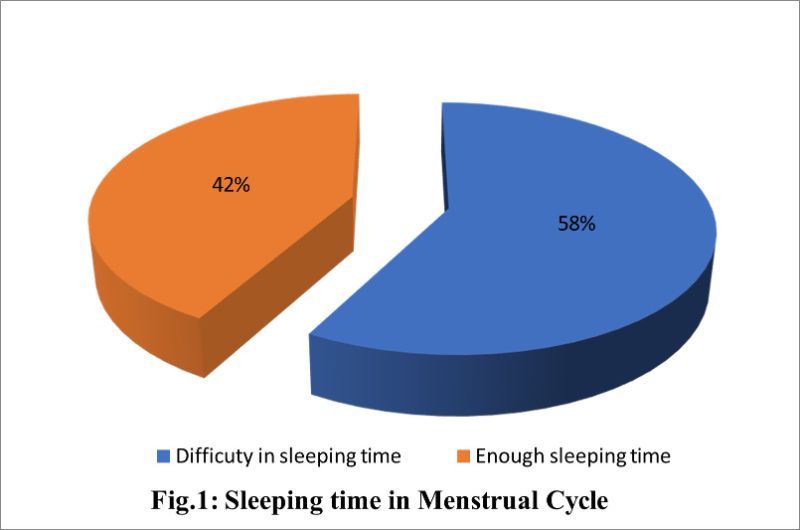
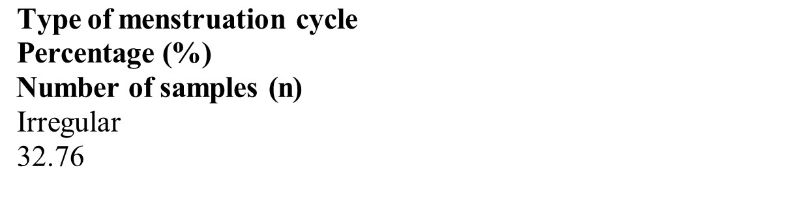
Figure 1 indicates that 58% of respondents experience sleep disturbances during menstruation, significantly impacting their overall well-being and daily functioning. Menstrual-related symptoms such as cramps, bloating, and hormonal fluctuations substantially contribute to sleep disruptions (Jenner, 2017; Sharma et al., 2008). Moreover, hormonal fluctuations—declining estrogen and progesterone levels before menstruation—further contribute to sleep issues (Jenner, 2017).
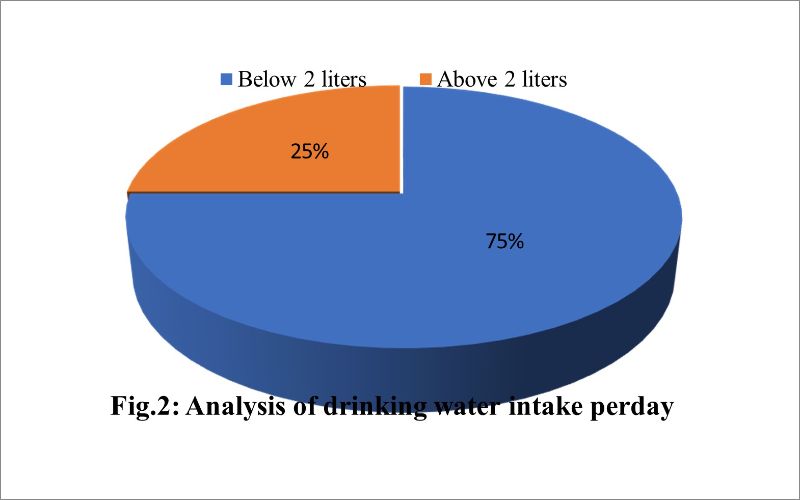
Figure 2 indicates that 75% of respondents consume less than two liters of water per day, while 25% exceed this amount. Adequate hydration is crucial for menstrual comfort and overall health, as it helps regulate bodily functions and can alleviate cramps (CDC, 2011; Markus et al., 2018). Reported self-care measures also include warm water baths, balanced nutrition (with ample fruits and vegetables), sufficient rest, regular physical activity, and limiting caffeinated beverages, alongside a recommended daily intake of 8–10 glasses of water (Aboushady & El-saidy, 2016).
Figure 3 shows that 85% of respondents change napkins every six hours, while 9% do so every two hours and 6% once per day. Although six-hourly changes align with standard recommendations, frequency varies according to product absorbency and individual menstrual flow. Night-time changes were practiced by 79.1% of girls, compared with only 20.6% who changed pads at school. Overall, 78.3% changed their napkins 2–3 times daily, and 16.6% changed them once daily. These hygiene practices differed by age group (Omidvar & Begum, 2010).
This study underscores a critical need for comprehensive menstrual health interventions explicitly tailored for rural Midnapore. Key recommendations for local authorities and health programs include:
Implementing these targeted policy interventions can significantly improve menstrual hygiene practices, reduce discomfort and stigma, and enhance overall health outcomes among adolescent girls in rural Midnapore.