International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 7 - Issue 5 - 2025
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
Francois Murinda1*, Theoneste Majyambere1, Delphine Nishimwe1,2, Athanase Nsengiyumva1, Clemence Muhayimana1, Boating Kwame3, Emmanuel Ndikumana1, Honore Harindintwali 4, Jean Paul Mvukiyehe1, Charles Kabano1, Vincent Sezibera5, Zephanie Nzeyimana6*
1Butare University Teaching Hospital, Huye, Rwanda.
2Cape Breton University, Toronto, Canada.
3Society of Critical Care Medicine, Chicago, USA.
4Michener Institute of Education, Toronto, Ontario, Canada.
5University of Rwanda, Huye, Rwanda.
6Rwanda Bimedical Centre, Kigali, Rwanda.
*Corresponding author: 1Francois Murinda (mulinda2020@gmail.com), Butare University Teaching Hospital, Huye, Rwanda,
6Zephanie Nzeyimana (zephanie2007@gmail.com and ORCID: https://orcid.org/0000-0002-4603-8050), Rwanda Bimedical Centre, Kigali, Rwanda.
Received: November 13, 2025 | Accepted: November 17, 2025 | Published: November 28, 2025
Citation: Murinda F, Majyambere T, Nishimwe D, Nsengiyumva A, Muhayimana C, Kwame B, Ndikumana E, Harindintwali H, Jean P Mvukiyehe, Kabano C, Sezibera V, Nzeyimana Z., (2025) “Factors associated with burnout core symptoms among healthcare providers at Butare University Teaching Hospital and District Hospitals under its catchment area, Rwanda”. International Journal of Epidemiology and Public Health Research, 7(5); DOI: 10.61148/2836-2810/IJEPHR/181.
Copyright: © 2025. Francois Murinda, Nzeyimana Zephanie. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Burnout remains a major occupational health concern globally, especially in healthcare services, where it affects the quality of service provision and customer satisfaction. This study aimed to determine the prevalence of burnout, identify associated factors, and assess effective coping strategies among healthcare providers at Butare University Teaching Hospital (BUTH) and its affiliated District Hospitals (DHs).
Methods: This cross-sectional study collected quantitative data from randomly selected healthcare providers (HCPs). A structured questionnaire was used to collect the data from August 28 to October 8, 2023. STATA v.17 was used to analyze the data at univariable, bivariable, and multivariable logistic regression levels.
Results: A total of 375 healthcare providers were interviewed, including Nurses (78.1%), physicians (8.0%), Midwives (5.6%), Anesthetists (3.5%), and paramedical professionals, including lab technologists, radiologists, and social workers (4.8%). This study found that approximately 22.4% of healthcare providers exhibited one or more core symptoms of burnout. A higher likelihood of burnout was observed among healthcare providers working in Gyneco-obstetric units compared to their counterparts in intensive care unit (aOR: 5.7, 95% CI: 1.1–29.9). Regarding coping practices, higher likelihoods of burnout were observed among healthcare workers who occasionally, seldom, or never sleep well at night for at least 8 to 9 hours (aOR: 2.7, 95% CI: 1.1–6.5) and those who occasionally, seldom, or never refuse inappropriate or excessive work demands (aOR: 2.1, 95% CI: 1.1–4.1), and those with moderately inadequate numbers of coping strategies (aOR: 3.2, 95% CI: 1.5–7.0).
Conclusion: This study reveals that approximately 1 in 5 healthcare providers at BUTH and its affiliated hospitals exhibit one or more core symptoms of burnout, with those in Gyneco-obstetric units facing relatively higher risks. The results emphasize the importance of HCPs implementing effective burnout coping strategies, such as having adequate sleep of at least 8 hours and being able to decline excessive work demands, particularly for those in labor and delivery units.
Key Points:
Burnout is known to affect the healthcare workforce worldwide, especially in low—and middle-income countries(LMICs).
This study was conducted to assess the prevalence and factors associated with burnout, along with burnout coping strategies that are associated with low likelihoods of having burnout among healthcare providers in hospitals referring to Butare university Teaching Hospital, southern province of Rwanda.
This study shows that about 12% of healthcare workers present one or more burnout core symptoms.
Healthcare providers (HCPs) working in Gyneco-obstetric units were most affected by burnout among other HCPs like those working in intensive care units (who are also known to be highly affected). They were 5.7 times higher risks of burnout than HCPs working in Paramedical units like Laboratory and medical imaging, among Others.
The findings highlight the importance of equipping healthcare providers—particularly those in labor and delivery units—with effective burnout coping strategies, such as the ability to set boundaries and decline excessive work demands.
Occupational health programs should pay special attention to staff working in gynecology and obstetrics, as they often operate under intense pressure to prevent maternal deaths and may fear legal consequences if adverse outcomes occur.
Burnout, occupational health, stress, burnout coping strategies
1. Introduction
Burnout is a psychological syndrome characterized by emotional exhaustion, feelings of helplessness, depersonalization, negative attitudes toward work and life, and a diminished sense of personal accomplishment [1]. It is increasingly recognized as a significant public health concern due to its detrimental effects on both mental and physical health, including chronic fatigue, musculoskeletal pain, gastrointestinal disturbances, and reduced quality of life [2]
Globally, the prevalence of burnout in the general working population of high-income countries ranges between 13% and 27% [3]–[5]. However, healthcare providers (HCPs) are particularly vulnerable due to their work's demanding and emotionally charged nature. Burnout rates among physicians have been reported as high as 70%, and nearly 50% among nurses. In the United States, studies indicate that 54% of physicians, 35% of hospital nurses, and 35.2% of medical students report experiencing burnout. Similar trends have been observed in other high-income countries [2].
Several factors within healthcare systems contribute to the high prevalence of burnout among healthcare professionals. These include excessive workload, time pressures, limited control over work processes, role ambiguity, and strained interprofessional relationships. The emotional demands of clinical care further exacerbate the risk. Burnout prevalence estimates among nurses range from 10% to 70%, and from 30% to 50% among physicians, nurse practitioners, and physician assistants. A 2015 study by the Mayo Clinic and the American Medical Association reported that over half of American physicians exhibited at least one symptom of burnout—an increase of 9% compared to a similar study conducted three years earlier [6].
Burnout has serious implications for the quality of care and patient safety. Clinicians experiencing burnout are more likely to report reduced patient safety, increased medical errors, and a decline in the quality of care delivered. Depersonalization in particular can lead to less empathetic patient interactions and diminished professional engagement [6].
In Sub-Saharan Africa, high levels of burnout among healthcare providers have also been documented. A study conducted in a Malawian referral hospital among maternal health staff found that 72% experienced emotional exhaustion, 43% reported depersonalization, and 74% indicated low personal accomplishment [7]. In Rwanda, Emeline (2017) reported that 61.7% of nurses working in the Emergency Department and Intensive Care Unit at Kigali University Teaching Hospital exhibited at least one indicator of burnout, with emotional exhaustion at 48.3%, depersonalization at 25.0%, and low personal accomplishment at 50.0% [8]. Another study conducted among anesthesia providers in 11 district and tertiary hospitals across Rwanda found a burnout prevalence of 26.3% [9].
In Rwanda, despite ongoing efforts by the Government of Rwanda to promote safe and healthy working environments through labor policies and workplace programs[10], healthcare providers continue to face high levels of occupational stress. Contributing factors include workforce shortages, extended working hours, and the inherently demanding nature of healthcare services.
In Rwanda, despite ongoing policy efforts by the Ministry of Public Service and Labour to improve workplace conditions [10], , healthcare providers remain vulnerable to occupational burnout. This is often attributed to systemic challenges such as workforce shortages, long working hours, and the emotionally demanding nature of healthcare services.
Therefore, this study aims to assess the determinants of burnout and explore the effective coping practices employed by healthcare providers working at Butare University Teaching Hospital (CHUB) and the District Hospitals (DHs) within its catchment area. The findings are expected to inform institutional and national strategies to mitigate burnout, enhance the resilience of Rwanda’s health workforce, and improve the quality of patient care.
2. Research methodology
5.1 Study design
This study was a cross-sectional study using a survey approach to collect quantitative data from the study participants.
5.2 Study Area
The research aimed to collect data from Butare Univeristy Teaching Hospital (BUTH) and 9 hospitals in its catchment areas including Kabutare DH (Huye), Kibilizi DH and Gakoma DH(Gisagara), Kabgayi DH (Muhanga), Bushenge and Kibogora DHs (Nyamasheke), Nyanza DH (Nyanza), Munini DH (Nyaruguru), and Gitwe and Ruhango DHs (Ruhango).
5.3 Study population and sample size
The study collected data from 374 healthcare providers including Nurses, General practitioners, Specialized Physicians, and Laboratory technologists working in selected services, including Critical care (CBUB), Emergency, labor and delivery (Maternity), Surgery, and internal medicine departments. This number is calculated using the following Yamane formula for a finite population.
n=N1+N(e)2 where:
where:
N: population size (2160),
e: margin of error held at 5%
n=21601+2160(0.05)2 = 337.5
= 337.5
Therefore, the current study will collect data from 337 HCPs. However, to adjust missing or incomplete responses, 10% of the sample size was added; equivalent to approximately 34 people. Thus, 374 Healthcare providers were recruited for this study.
5.4 Inclusion and exclusion criteria
Below are the inclusion and exclusion criteria for study participation.
5.5 Inclusion and exclusion criteria
Healthcare providers were included in the study if they were voluntarily willing to participate in the study, had been working in selected hospitals for at least 6 months, had at least two years of working experience, and were aged 18 years by the time of data collection.
5.6 Exclusion Criteria
All participants fulfilling inclusion criteria were excluded from the study if they had an illness that prevented them from correctly and accurately answering survey questions.
5.7 Data collection tools
This study used a questionnaire (Appendix B) to collect the required data. The questionnaire collects data on demography, burnout core symptoms to measure exhaustion, mental distance, cognitive impairment, and emotional impairment, and burnout secondary symptoms including psychological and psychosomatic complaints. It also captures information on stress-coping practices among the study participants. Questions were adapted from Maslash Burnout Inventory(MBI)[11], [12]
5.8 Data collection process
After receiving ethical approval from the CHUB Research committee, we planned to reach the participant for a face-to-face interview guided by a questionnaire (Appendix B). Data were collected using an open data kit (ODK) form. Data collection was conducted from August 28 to October 8, 2023.
5.9 Data analysis
After collecting data, we will analyze data using STATA 15 version for quantitative analysis while quantitative data were analyzed using thematic analysis. Data were analyzed at univariable, bivariable, and multivariable analysis levels. A Chi-square test was computed to test the significance of the association, which was assumed at a p-value less than 0.05 and a 95% confidence interval. Findings are presented in tables and figures.
5.10 Ethical Consideration and Confidentiality
Following the Helsinki declaration, this study adhered to ethical research considerations including ethical review and informed consent. An ethical clearance letter (Approval Notice: No: REC/UTHB/058 /2023) was obtained from Butare Univerity Hospital Institutional Review Board. and informed consent was obtained from the study participants before data collection. Moreover, collected data were kept confidential and used for research purposes only.
3. Results
This study was conducted to determine the prevalence of burnout syndrome and factors associated with having burnout core symptoms among healthcare providers. It was also conducted to determine coping strategies associated with less likelihood of having burnout core symptoms. Below are findings on the study objectives along with a description of the study participants.
3.1 Sociodemographic characteristics of the study participants
The larger proportion of the study participants had 11 to 28 years of working experience (43.5%), were catholic church members (58.6%), and were working in internal medicine or the emergency department (18.7%).
This study surveyed 374 healthcare workers across various hospitals, with the majority being nurses (78%) and highly educated (98.9% university level or higher). The workforce was predominantly female (62%), and the largest age group was 31-40 years (51.3%). Most participants had 1 to 3 children (59%), and 78.3% were satisfied with their marital status. Economic stability appeared strong, with 96.5% in economic category III, and only 10.7% had secondary jobs (mostly schooling or part-time work). Regarding work experience, 43.5% had over 11 years in the profession, and 43.6% had been at their current hospital for 1-5 years. The most commonly assigned wards were surgery (20.6%), emergency care (18.7%), and internal medicine (18.7%). Around 97.1% had not experienced intimate partner violence in the past year, and the workforce was largely religious, with 58.6% identifying as Catholic. Table 1 shows the socio-demographic characteristics. Table 1 provides further information about the socio-demographic characteristics of the study participants.
Table 1: Socio-demographic of the study participants
|
Participants' characteristics |
Frequency |
Percent |
Participants' characteristics |
Frequency |
Percent |
|
Hospital name |
If other occupation after work, which one? |
||||
|
CHUB |
88 |
23.5 |
Part-timing somewhere |
7 |
24.1 |
|
Kabutare DH |
38 |
10.2 |
I go to school |
18 |
62.1 |
|
Kibilizi DH |
32 |
8.6 |
Trade |
2 |
6.9 |
|
Gakoma DH |
22 |
5.9 |
Agriculture |
2 |
6.9 |
|
Nyanza DH |
18 |
4.8 |
Number of children |
||
|
Kabgayi DH |
44 |
11.8 |
Zero |
93 |
24.9 |
|
Munini DH |
27 |
7.2 |
1 to 3 |
221 |
59 |
|
Gitwe DH |
21 |
5.6 |
4 and above |
60 |
16.1 |
|
Ruhango PH |
27 |
7.2 |
Whether happy with/in your current marital status |
||
|
Bushenge PH |
29 |
7.8 |
Yes |
293 |
78.3 |
|
Kigeme DH |
28 |
7.5 |
No |
81 |
21.7 |
|
Age |
Experienced intimate partner violence in last 12 months |
||||
|
24 to 30 |
92 |
24.6 |
Yes |
11 |
2.9 |
|
31 to 40 |
192 |
51.3 |
No |
363 |
97.1 |
|
40 + |
90 |
24.1 |
Work experience |
||
|
Gender |
1 to 5 years |
112 |
30 |
||
|
Male |
142 |
38 |
6 to 10 years |
99 |
26.5 |
|
Female |
232 |
62 |
11 to 28 years |
163 |
43.5 |
|
Highest education attained |
How long have you been working in this hospital |
||||
|
Secondary |
4 |
1.1 |
1 to 5 years |
163 |
43.6 |
|
University and above |
370 |
98.9 |
6 to 10 years |
111 |
29.7 |
|
Economic category |
11 to 28 years |
100 |
26.7 |
||
|
I |
0 |
0(0) |
Religion |
||
|
II |
9 |
2.5 |
Catholic |
219 |
58.6 |
|
III |
361 |
96.5 |
Seventh-day Adventist |
60 |
16 |
|
IV |
4 |
1 |
Pentecost |
63 |
16.8 |
|
Occupation |
Muslim and others |
32 |
8.6 |
||
|
Nurses |
293 |
78 |
Assigned ward/service |
||
|
MD or Specialized P |
30 |
8 |
ICU |
22 |
5.9 |
|
Midwives |
21 |
5.9 |
Internal medicine |
70 |
18.7 |
|
Anesthetists |
13 |
3.5 |
Emergence |
70 |
18.7 |
|
Other occupations* |
17 |
4.6 |
Gyneco-obstetric |
61 |
16.3 |
|
Do you have another occupation after work? |
Surgery |
77 |
20.6 |
||
|
Yes, or prefer not to say |
40 |
10.7 |
Other occupations* |
74 |
19.8 |
|
No |
334 |
89.3 |
Total |
374 |
100 |
*Other occupation
3.2 Prevalence and categories of burnout among healthcare providers
Using a scale of 1 to 5, with 1 standing for lowest frequency and 5 for highest (1. Never, 2. Rarely, 3. Sometimes, 4. Often, and 5. Always), participants rated how they experience burnout core-symptoms listed in appendix B (e.g.: like When I exert myself at work, I quickly get tired for exhaustion). Participants who responded to experience the symptoms often or always were considered to have the core symptoms and thus, burnout.
Based on the participants’ responses to burnout assessment questions (Appendix B) assessing core symptoms of burnout core symptoms including those of exhaustion, cognitive impairment, emotional impairment, and mental distress. This study shows that about 22.4% of the interviewed healthcare providers reported sufficient or extreme amounts of burnout core symptoms. About 16.5% of the health care workers were having symptoms of exhaustion, while 9.3% had mental distress symptoms. Rates of cognitive impairment and emotional impairment symptoms were relatively lower, with 4.5% and 5.1%, respectively. Figure 1 and Table 2 show further information. Appendix A provides detailed information on participants' responses about felt burnout symptoms used to classify presence or absence of burnout for this research
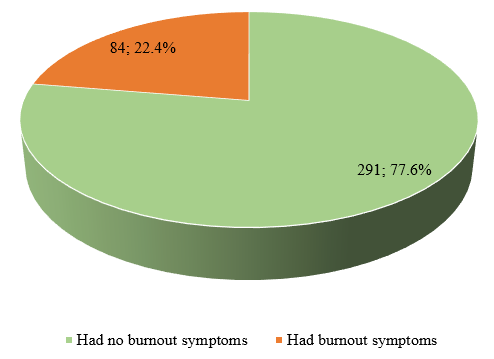
Figure 1: Prevalence of core burnout symptoms among healthcare workers
Table 2: Burnout core symptoms identified among healthcare providers
|
Burnout core symptoms |
Frequency (n) |
Percent (%) |
|
Exhaustion symptoms |
||
|
None to moderate |
313 |
83.5 |
|
Sufficiently or extremely |
62 |
16.5 |
|
Cognitive impairment symptoms |
|
|
|
None to moderate |
356 |
94.9 |
|
Sufficiently or extremely |
19 |
5.1 |
|
Emotional impairment symptoms |
|
|
|
None to moderate |
358 |
95.5 |
|
Sufficiently or extremely |
17 |
4.5 |
|
Mental distress symptoms |
|
|
|
None to moderate |
340 |
90.7 |
|
Sufficiently or extremely |
35 |
9.3 |
|
Total |
375 |
100 |
3.3 Factors associated with having one or more burnout core symptoms
To determine factors associated with burnout symptoms, participants’ characteristics were cross-tabulated with having burnout symptoms. Several variables showed statistical significance at p value less than 0.05. Statistically significantly higher proportions of healthcare workers with burnout core symptoms were among Midwives (66.67%), participants with secondary education (75%), 4 children and above (45.0%), happy in their current marital status (25.2%), working in their hospitals for 11 to 28 years (29.5%) and those working in Gyneco-obstetric unit (44.3%).
All variables associated with having one or more burnout core symptom(s) were put in one logistic regression model, and only one variable was statistically associated with having burnout core symptoms. Healthcare providers working in Gyneco-obstetric units were 5.7 times more likely to have burnout than those working in ICU units (aOR: 5.7 with 95% CI:1.1-29.9). Table 3 provides further information.
Table 3: Socio-demographic characteristics associated with burnout among healthcare workers
|
Had no Burnout |
Had burnout |
N |
Chi2 |
P Value |
aOR* |
95% CI Lower Upper |
p value |
||
|
Age band |
|
|
|
|
|||||
|
24 to 30 |
78(84.8) |
14(15.2) |
92 |
4.3378 |
0.114 |
|
|
|
|
|
31 to 40 |
147(76.6) |
45(23.4) |
192 |
|
|
|
|
||
|
40 + |
65(72.2) |
25(27.8) |
90 |
|
|
|
|
||
|
Gender |
|
|
|
|
|||||
|
Male |
115(81.0) |
27(19.0) |
142 |
1.5607 |
0.212 |
|
|
|
|
|
Female |
175(75.4) |
57(24.6) |
232 |
|
|
|
|
||
|
Highest education attained |
|
|
|
|
|||||
|
Secondary education |
1(25.0) |
3(75.0) |
4 |
6.4088 |
0.011 |
8.7 |
0.8 |
100.0 |
0.083 |
|
University and above |
289(78.1) |
81(21.9) |
370 |
Ref |
|
|
|
||
|
Economic category |
|
|
|
|
|
|
|
||
|
I |
0 (0) |
0 (0) |
0 |
2.5814 |
0.275 |
|
|
|
|
|
II |
5(55.6) |
4(44.4) |
9 |
|
|
|
|
|
|
|
III |
282(78.1) |
79(21.9) |
361 |
|
|
|
|
||
|
IV |
3(75.0) |
1(25.0) |
4 |
|
|
|
|
||
|
Occupation |
|
|
|
|
|||||
|
Nurses |
233(79.5) |
60(20.5) |
293 |
26.4818 |
<0.001 |
0.9 |
0.2 |
3.6 |
0.885 |
|
MD or Specialized P |
25(83.3) |
5(16.7) |
30 |
1.1 |
0.2 |
6.8 |
0.907 |
||
|
Midwives |
7(33.3) |
14(66.7) |
21 |
3.0 |
0.5 |
17.6 |
0.22 |
||
|
Anesthetists |
12(92.3) |
1(7.7) |
13 |
0.3 |
0.0 |
3.8 |
0.366 |
||
|
Other professions |
7(33.3) |
14(66.7) |
21 |
Ref |
|
|
|
||
|
Do you have other occupation after work? |
|
|
|
|
|||||
|
Yes, or prefer not to say |
31(77.5) |
9(22.5) |
40 |
0.0003 |
0.987 |
|
|
|
|
|
No |
260(77.6) |
75(22.4) |
335 |
|
|
|
|
||
|
If other occupation |
|
|
|
|
|||||
|
Part-timing somewhere |
17(94.4) |
1(5.6) |
18 |
7.8836 |
0.096 |
|
|
|
|
|
I go to school |
2(100.0) |
0(0.0) |
2 |
|
|
|
|
||
|
Trade |
1(50.0) |
1(50.0) |
2 |
|
|
|
|
||
|
Agriculture |
6(54.5) |
5(45.5) |
11 |
|
|
|
|
||
|
Prefer not to say |
1(50.0) |
1(50.0) |
2 |
|
|
|
|
||
|
Number of children |
|
|
|
|
|||||
|
Zero |
80(85.1) |
14(14.9) |
94 |
12.0 |
0.002 |
Ref |
|
|
|
|
1 to 3 |
178(80.5) |
43(19.5) |
221 |
0.6 |
0.2 |
1.7 |
0.393 |
||
|
4 children and above |
33(55.0) |
27(45.0) |
60 |
1.6 |
0.5 |
4.9 |
0.392 |
||
|
Whether happy with/in |
|
|
|
|
|||||
|
Yes |
220(74.8) |
74(25.2) |
294 |
6.0085 |
0.014 |
2.1 |
0.8 |
5.7 |
0.139 |
|
No |
71(87.6) |
10(12.4) |
81 |
Ref |
|
|
|
||
|
Experienced intimate partner |
|
|
|
|
|||||
|
Yes |
9(75) |
3(25) |
12 |
0.0482 |
0.826 |
|
|
|
|
|
No |
282(77.69) |
81(22.31) |
363 |
|
|
|
|
||
|
If IPV in last 12 months, was it sexual violence |
|
|
|
|
|||||
|
Yes |
2(100) |
0(0) |
2 |
0.9167 |
0.338 |
|
|
|
|
|
No |
6(66.67) |
3(33.33) |
9 |
|
|
|
|
||
|
How long have you been |
|
|
|
|
|||||
|
1 to 5 years |
139(84.8) |
25(15.2) |
164 |
10.3699 |
0.006 |
Ref |
|
|
|
|
6 to 10 years |
84(75.7) |
27(24.3) |
111 |
1.7 |
0.8 |
3.4 |
0.145 |
||
|
11 to 28 years |
68(68.0) |
32(32.0) |
100 |
1.8 |
0.8 |
3.8 |
0.133 |
||
|
Religion |
|
|
|
|
|||||
|
Catholic |
176(80) |
44(20) |
220 |
2.0328 |
0.566 |
|
|
|
|
|
Seventh day Adventist |
44(73.33) |
16(26.67) |
60 |
|
|
|
|
||
|
Pentecost |
48(76.19) |
15(23.81) |
63 |
|
|
|
|
||
|
Muslim and others |
23(71.88) |
9(28.13) |
32 |
|
|
|
|
||
|
Assigned ward/service |
|
|
|
|
|||||
|
ICU |
20(90.91) |
2(9.09) |
22 |
25.2314 |
<0.001 |
Ref |
|
|
|
|
Internal medicine |
51(72.86) |
19(27.14) |
70 |
3.5 |
0.7 |
17.1 |
0.122 |
||
|
Emergence |
60(85.71) |
10(14.29) |
70 |
2.0 |
0.4 |
10.3 |
0.407 |
||
|
Gyneco-obstetric |
34(55.7) |
27(44.3) |
61 |
5.7 |
1.1 |
29.9 |
0.038 |
||
|
Surgery |
60(85.71) |
10(14.29) |
70 |
2.5 |
0.5 |
12.9 |
0.268 |
||
|
Others ** |
34(55.74) |
27(44.26) |
61 |
2.9 |
0.6 |
14.9 |
0.206 |
||
|
*aOR: adjusted odd ratios **Other occupations include pediatrics, allied health professionals |
|||||||||
3.4 Stress-coping mechanisms and burnout among healthcare providers
To determine burnout coping strategies associated with less likelihood of burnout among healthcare symptoms, we cross-tabulated the frequency at which providers exercise various coping mechanisms and experience of burnout. Several coping mechanisms were found associated with less likelihood of burnout among the health care providers and they include taking a full day off frequently or weekly (16.4%), having frequent or daily time out to think, reflect, meditate, or pray (17.7%), doing aerobic exercise frequently or 3 to 5 times a week (8.9%), and ability to always or mostly say no to inappropriate or excessive demands (13.7.
All coping mechanisms were put in one logistic regression model to find the strength and direction of association with burnout. Only one variable showed significant association with burnout among the healthcare provides (HCPs). Inability to consistently or mostly say no to inappropriate or excessive demands was associated with a 2.1 times higher likelihood (aOR: 2.1, 95% CI: 1.1–4.1) of experiencing burnout core symptoms. Similarly, healthcare workers who occasionally, seldom, or never sleep well at night for at least 8 to 9 hours were 2.7 times more likely (aOR: 2.7, 95% CI: 1.1–6.5) to experience these symptoms compared to those who always or mostly sleep well.
Considering adoption range preventative measures to cope with burnout among healthcare providers, participants' score on several adopted coping mechanisms were grouped into a wide range (60-100), adequate (40-59), moderately inadequate (30 to 39), and moderate inadequate (0 to 29) coping mechanisms. The current study shows that the adoption of more burnout coping mechanisms is associated with a less likelihood of burnout among healthcare providers. HCPs with moderately inadequate coping mechanisms were 3.2 (aOR: 3.2 with 95% CI: 1.5-7.0) times more likely to present burnout than those with a wide range of coping mechanisms. Thus, this study shows that the risks of presenting one or more burnout core symptoms significantly decline with the number of stress-coping mechanisms. Table 4 provides further information.
Table 4: Association between stress-coping mechanisms and burnout among healthcare providers
|
Burnout Yes No |
N |
X2 |
p Value |
aOR* |
95% CI Lower Upper
|
p value |
||||
|
Do you have a full day off to do what you like? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Never |
122(70.52) |
51(29.48) |
173 |
9.1085 |
0.003 |
Ref |
|
|
|
|
|
Weekly/Mostly/Frequently |
168(83.58) |
33(16.42) |
201 |
|
|
0.6 |
0.3 |
1.2 |
0.185 |
|
|
Do you have time out for yourself to think, reflect, meditate and pray? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Seldom or never |
159(72.6) |
60(27.4) |
219 |
7.3967 |
0.007 |
Ref |
|
|
|
|
|
Daily/Frequently |
131(84.52) |
24(15.48) |
155 |
|
|
0.8 |
0.4 |
1.7 |
0.629 |
|
|
Do you have good vacations, about 3 - 4 weeks in each year? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Never |
131(72.38) |
50(27.62) |
181 |
5.2503 |
0.022 |
Ref |
|
|
|
|
|
Every year/Some years |
158(82.29) |
34(17.71) |
192 |
|
|
1.2 |
0.6 |
2.4 |
0.527 |
|
|
Do you do some aerobic exercise for at least half an hour at a time? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Seldom or never |
218(73.9) |
77(26.1) |
295 |
10.6357 |
0.001 |
Ref |
|
|
|
|
|
3 to 5 times a week/Frequently |
72(91.14) |
7(8.86) |
79 |
|
|
0.6 |
0.2 |
1.7 |
0.342 |
|
|
Do you do something for fun or enjoyment Eg. Game, movie, concert? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Seldom or never |
218(74.15) |
76(25.85) |
294 |
8.8231 |
0.003 |
Ref |
|
|
|
|
|
3 to 5 times a week/Frequently |
71(89.87) |
8(10.13) |
79 |
|
|
0.6 |
0.2 |
1.6 |
0.3 |
|
|
Do you practice any muscle relaxation or slow breathing technique? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Seldom or never |
243(76.18) |
76(23.82) |
319 |
2.3193 |
0.128 |
|
|
|
|
|
|
Daily/Frequently |
47(85.45) |
8(14.55) |
55 |
|
|
|
|
|
|
|
|
Do you listen to your body messages (symptoms, illnesses, etc)? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Seldom or never |
195(79.59) |
50(20.41) |
245 |
1.825 |
0.177 |
|
|
|
|
|
|
Always/Mostly |
94(73.44) |
34(26.56) |
128 |
|
|
|
|
|
|
|
|
IF SINGLE: Do you have friends with whom you can share at a feelings level? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/ Seldom or never |
108(72) |
42(28) |
150 |
3.7835 |
0.052 |
|
|
|
|
|
|
Regularly/Frequently |
153(80.95) |
36(19.05) |
189 |
|
|
|
|
|
|
|
|
IF MARRIED (or in a relationship): how often do you share intimately? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Seldom or never |
117(82.98) |
24(17.02) |
141 |
4.2806 |
0.039 |
Ref |
|
|
|
|
|
Daily/Frequently |
168(73.68) |
60(26.32) |
228 |
|
|
1.7 |
1 |
3 |
0.069 |
|
|
Do you share your stressors [cares, problems, struggles, needs] with others & God? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Seldom or never |
187(76.02) |
59(23.98) |
246 |
0.9584 |
0.328 |
|
|
|
|
|
|
Regularly/Frequently |
103(80.47) |
25(19.53) |
128 |
|
|
|
|
|
|
|
|
How would you describe your ability to communicate with others? |
|
|
|
|
|
|
|
|
|
|
|
Difficult/Poor |
14(70) |
6(30) |
20 |
0.6776 |
0.41 |
|
|
|
|
|
|
Excellent/Fair |
275(77.9) |
78(22.1) |
353 |
|
|
|
|
|
|
|
|
Do you sleep well (8-9 hours per night)? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Seldom or never |
246(75.69) |
79(24.31) |
325 |
4.8633 |
0.027 |
Ref |
|
|
|
|
|
Frequently |
44(89.8) |
5(10.2) |
49 |
|
|
2.7 |
1.1 |
6.5 |
0.028 |
|
|
Are you able to say "No!" to inappropriate or excessive demands on you ? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Seldom or rare |
114(67.06) |
56(32.94) |
170 |
19.6601 |
<0.001 |
Ref |
|
|
|
|
|
Always/Mostly |
176(86.27) |
28(13.73) |
204 |
|
|
2.1 |
1.1 |
4.1 |
0.006 |
|
|
Do you set realistic goals for your life, both long and short term? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Seldom or rare |
92(68.15) |
43(31.85) |
135 |
10.4187 |
0.001 |
Ref |
|
|
|
|
|
Regularly/Frequently |
196(82.7) |
41(17.3) |
237 |
|
|
0.8 |
0.4 |
1.5 |
0.441 |
|
|
Are you careful to eat a good balanced diet? |
|
|
|
|
|
|
|
|
|
|
|
Not often/A lot of junk food |
11(73.33) |
4(26.67) |
15 |
0.1588 |
0.69 |
|
|
|
|
|
|
Always/Mostly |
279(77.72) |
80(22.28) |
359 |
|
|
|
|
|
|
|
|
Is your weight appropriate for your height? |
|
|
|
|
|
|
|
|
|
|
|
Overweight |
22(78.57) |
6(21.43) |
28 |
0.0185 |
0.892 |
|
|
|
|
|
|
Consistently/A battle |
268(77.46) |
78(22.54) |
346 |
|
|
|
|
|
|
|
|
How would you describe the amount of touch you get in your life? |
|
|
|
|
|
|
|
|
|
|
|
I miss out/I am rarely |
132(75.86) |
42(24.14) |
174 |
0.4892 |
0.484 |
|
|
|
|
|
|
Plenty/Just enough |
157(78.89) |
42(21.11) |
199 |
|
|
|
|
|
|
|
|
Can you deal with anger without repressing or dumping it on others? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Rarely/Never |
11(57.89) |
8(42.11) |
19 |
4.5256 |
0.033 |
Ref |
|
|
|
|
|
Always/Mostly |
278(78.75) |
75(21.25) |
353 |
|
|
2 |
0.7 |
5.5 |
0.188 |
|
|
Do you have a good "belly laugh"? |
|
|
|
|
|
|
|
|
|
|
|
Seldom/Never |
121(72.46) |
46(27.54) |
167 |
4.4799 |
0.034 |
Ref |
|
|
|
|
|
At least daily/Frequent |
169(81.64) |
38(18.36) |
207 |
|
|
1.5 |
0.7 |
3.1 |
0.299 |
|
|
Do you have a creative hobby time ( E.g. Gardening, reading, music)? |
|
|
|
|
|
|
|
|
|
|
|
Rarely/Never |
193(74.23) |
67(25.77) |
260 |
5.1925 |
0.023 |
Ref |
|
|
|
|
|
Weekly/Occasionally |
96(84.96) |
17(15.04) |
113 |
|
|
1.4 |
0.6 |
3 |
0.458 |
|
|
Do you nurture your self-esteem (E.g. with self-affirmations)? |
|
|
|
|
|
|
|
|
|
|
|
Occasionally/Rarely |
21(67.74) |
10(32.26) |
31 |
1.8634 |
0.172 |
|
|
|
|
|
|
Regularly/Frequently |
269(78.43) |
74(21.57) |
343 |
|
|
|
|
|
|
|
|
Do you practice forgiveness of others who have hurt you? |
|
|
|
|
|
|
|
|
|
|
|
Rarely/Never |
25(69.44) |
11(30.56) |
36 |
1.4991 |
0.221 |
|
|
|
|
|
|
Regularly/Occasionally |
265(78.4) |
73(21.6) |
338 |
|
|
|
|
|
|
|
|
Have you dealt with old hurts and "baggage" from the past? |
|
|
|
|
|
|
|
|
|
|
|
A lot left yet |
104(68.87) |
47(31.13) |
151 |
10.9204 |
0.001 |
Ref |
|
|
|
|
|
All that you are aware of |
186(83.41) |
37(16.59) |
223 |
|
|
1.4 |
0.7 |
2.6 |
0.305 |
|
|
Overall coping practice score /100** |
|
|
|
|
|
|
|
|
|
|
|
0 to 29 |
17 (73.9) |
6(26.1) |
23 |
11.4 |
0.010 |
2.4 |
0.8 |
7.5 |
0.133 |
|
|
30 to 39 |
78 (67.8) |
37(32.2) |
115 |
|
|
3.2 |
1.5 |
7.0 |
0.003 |
|
|
40 to 59 |
128(80.5) |
31(19.5) |
159 |
|
|
1.6 |
0.8 |
3.6 |
0.205 |
|
|
60 to 100 |
68(87.2) |
84(22.8) |
78 |
|
|
Ref |
|
|
|
|
|
*aOR: Adjusted odd ratio. **wide range (60-100), adequate (40-59), moderately inadequate (30 to 39), and moderate inadequate (0 to 29) coping mechanisms |
||||||||||
4. Discussion
This study highlights that burnout remains a significant public health concern, affecting approximately 22.4% of healthcare providers (HCPs) who reported experiencing at least one core symptom of burnout. The analysis identified one key occupational factor associated with higher likelihood of burnout risk; healthcare providers working in Gyneco-obstetric units were 5.7 times more likely to have burnout than those working in ICU units (aOR:5.7 with 95% CI:1.1-29.9). Additionally, inadequate coping strategies were significantly linked to burnout; HCPs who could not consistently refuse inappropriate or excessive demands were 2.1 times more likely to show core burnout symptoms (aOR: 2.1, 95% CI: 1.1–4.1), while those with moderate inadequate coping mechanisms faced 3.2 fold increased risk compared to those employing a wide range of coping strategies (aOR: 3.2, 95% CI: 1.5–7.0). Overall, the study suggests that the likelihood of experiencing burnout symptoms decreases with the use of diverse and effective stress-coping mechanisms.
4.1 Prevalence and categories of burnout among healthcare providers
Burnout among healthcare providers (HCPs) has emerged as a critical occupational health concern worldwide, with particularly profound implications in low- and middle-income countries (LMICs) where healthcare systems are often overstretched. In this context, the finding is that approximately 22.4% of reported experiencing at least one core symptom of burnout HCPs at Butare University Hospital and Hospitals under its catchment area in southern province, Rwanda [13] warrants serious attention. Burnout is typically characterized by emotional exhaustion, depersonalization, and reduced personal accomplishment[14], and is known to compromise both the well-being of providers and the quality of care delivered to patients.
This reported prevalence aligns with estimates from similar resource-constrained settings. For example, studies from sub-Saharan Africa have documented burnout rates ranging from 15% to over 40%, often linked to high workloads, limited staffing, and emotional strain associated with caring for populations with complex health needs [1], [15]. In Rwanda, health professionals continue to navigate demanding workloads related to communicable diseases such as outpatient diagnosis, reproductive, labor and delivery, HIV, tuberculosis, and malaria while also addressing a growing burden of non-communicable and mental health conditions.
4.2 Factors associated with having one or more burnout core symptoms
Gyneco-obstetric department often involves emotionally complex patient interactions, frequent exposure to reproductive loss, high patient turnover, and the provision of care in time-sensitive or emergency situations such as labor complications and miscarriages [16]. These settings also demand high levels of empathy and emotional labor, particularly when dealing with culturally sensitive issues around reproductive health and gender-based violence, which may not be as prevalent in ICU settings [17].
Furthermore, unlike ICUs, which may benefit from more structured team protocols and continuous monitoring equipment, Gyneco-obstetric wards—especially in resource-limited settings—often face shortages of specialized staff and equipment, leading to role overload and increased stress [18]. The burden is compounded by night shifts, insufficient staffing, and a high volume of patients, all of which contribute to emotional exhaustion, a key component of burnout [19].
The significant adjusted odds ratio and its relatively narrow confidence interval suggest a robust association that warrants attention from health system managers and policymakers. Targeted mental health interventions, supportive supervision, and the integration of psychosocial support services are urgently needed in Gyneco-obstetric units. In addition, ongoing professional development and debriefing sessions may help providers process emotionally challenging experiences, thereby reducing the risk of burnout and improving the quality of patient care.
4.3 Stress-coping mechanisms and burnout among healthcare providers
The present study reveals a strong association between inadequate coping strategies and the presence of burnout symptoms among healthcare providers (HCPs) in Rwanda. Specifically, HCPs who were unable to consistently refuse inappropriate or excessive demands were 2.1 times more likely to exhibit core burnout symptoms (aOR: 2.1; 95% CI: 1.1–4.1). More strikingly, those reporting moderate inadequate coping mechanisms had a 3.2-fold increased risk of burnout compared to their peers who utilized a broad range of coping strategies (aOR: 3.2; 95% CI: 1.5–7.0). These findings underscore the crucial role of adaptive coping in mitigating occupational stress and preventing burnout in resource-constrained healthcare settings.
The study found that healthcare workers who rarely or never slept 8–9 hours per night were 2.7 times more likely to experience symptoms of burnout. This is consistent with existing research showing a strong link between inadequate sleep and mental health issues in healthcare workers[20]. During the COVID-19 pandemic, a meta-analysis revealed prevalence rates of approximately 35% for depression, 37% for anxiety, and 43% for sleep disturbances among nursing staff[21]. Numerous studies have also shown that sleep disruption due to shift work, common in healthcare settings, is associated with higher risks of depression, anxiety, and stress. Dysfunctional sleep can disrupt the circadian rhythm, affect stress-related hormones (such as cortisol and melatonin), impact energy levels, and hinder emotional regulation, all contributing to an increased vulnerability to psychological distress[22]. Therefore, the findings of your study are in line with existing evidence and underscore the importance of prioritizing sleep health among healthcare workers as a potentially modifiable factor to reduce the risk of mental health issues.
Coping strategies—both adaptive (e.g., seeking support, problem-solving) and maladaptive (e.g., avoidance, withdrawal)—are key moderators of stress and burnout risk. In this context, the inability to set boundaries or decline unreasonable work demands reflects poor assertiveness and impaired self-regulation, which have been consistently linked to higher burnout levels in healthcare providers [23].
The observed dose-response relationship between coping adequacy and burnout—especially the markedly higher odds among those with severely limited coping options—suggests that burnout is not solely a function of workload or environment, but also of individual resilience and psychosocial skillsets[24]. In Rwanda, where health systems are often overstretched, HCPs may internalize systemic pressures, leading to overcommitment and emotional depletion in the absence of effective coping mechanisms [25].
These findings support the integration of structured psychosocial support interventions into healthcare institutions. This could include resilience training, communication and assertiveness workshops, regular mental health screening, and access to counseling services. Moreover, fostering a workplace culture that normalizes help-seeking behavior and promotes psychological safety is essential in reducing the stigma around mental health and encouraging adaptive coping [26].
5. Conclusion
This study underscores burnout as a pressing public health issue among healthcare providers in Rwanda, with 22.4% reporting at least one core symptom of burnout. The findings highlight significant occupational and psychosocial determinants of burnout, with Healthcare providers working in Gyneco-obstetric units being disproportionately affected. Critically, the ability to employ diverse and effective coping strategies emerged as a protective factor, whereas inadequate coping strategies increased burnout risk. These results call for targeted interventions that address workplace stressors, strengthen coping capacities, and promote mental well-being—particularly among high-risk groups such as nurses and Gyneco-obstetric staff—to enhance resilience and ensure sustainable healthcare delivery.
6. Recommendations
The findings underscore the need to avail a wide range of stress coping mechanisms to help healthcare workers cope with work-related stress focusing on Midwives and other staff working Gyneco-obstetric department. Strengthen Coping Skills Training: Regular workshops on stress management, emotional resilience, assertive communication, and time management should be integrated into continuous professional development programs, particularly targeting nurses and staff in Gyneco-obstetric units. Ministry of Health and health facilities should regularly train the healthcare workforce on work-related stress coping strategies and time management. They should also normalize conversations around mental health and create safe spaces where healthcare providers can express concerns, seek help without stigma, and participate in organizational improvements. Lastly, this study also highlights the need for further studies aiming to understand why Nurses and Gyneco-obstetric healthcare workers are disproportionately affected by burnout in Rwanda.
7. Supplementary Information
None
8. Acknowledgements
The authors are so grateful to the data collectors to the Butare University Teaching hospital for the research grant and all its support to successfully conduct this study. They are also thankful to selected district hospitals and study participants for their contribution in this study.
9. Authors’ contributions
FM conceptualized the study. FM and ZN produced the first draft of the study protocol. FM, ZN, TM, DN, and CM contributed in the final version of the study protocol and data collection materials. TM, DN, CM conducted data collection. ZN and MF analyzed the data and drafted study manuscript. BK, CK, EM, HH, JPM, AN, and VS revised the manuscript. All Authors contributed in the final version of the manuscript.
10. Funding
This research received funding from Butare university Teaching Hospital Research Center
11. Data Availability
All raw data and other processed data can be obtained from the corresponding author upon request.
12. Supplementary file
None
13. Declarations
Ethics approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. This research was conducted after obtaining ethical approval from the ethical research committee of Mount Kenya University (approval number: REF: MKU/ETHICS/023/2022) and subsequent approval from the Ministry of Health-Rwanda National Ethics Committee/RNEC (approval number: FWA Assurance No. 00001973. IRB00001497 of IORG0001100). In addition, approval from health centers was sought before embarking on data collection.
Participants were informed about the aim of the study, and participation was voluntary. Informed consent was obtained from all subjects who participated in this
the consent entails. Afterwards, a signature or print was gotten from the participant before participation.
14. Consent for publication
Not applicable.
15. Competing interests
The authors declare no competing interests.