International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 5 - Issue 1 - 2025
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
Abdala Kingwengwe Aimé1,2,3,4*, Wete Walombua Keneth4, Shongo Ya Pongombo Mick5, Shindano Mwamba Etienne1,2,3, Wembonyama Okitotsho Stanislas5
1University of Kindu, Faculty of Medicine, Department of Pediatrics.
2University of Kindu, Faculty of Medicine, Disease Prevention and Control Unit.
3Kindu General Referral Hospital, Pediatrics Department.
4Kimbanguiste Hospital of Kimbanseke, Pediatrics Department.
5University Clinics of Lubumbashi, Department of Pediatrics, University of Lubumbashi.
*Corresponding author: Abdala Kingwengwe Aimé, University of Kindu, Faculty of Medicine, Department of Pediatrics.
Received: November 13, 2025 | Accepted: November 17, 2025 | Published: November 20, 2025
Citation: Abdala K Aimé, Wete W Keneth, Pongombo Mick SY, Shindano M Etienne, Wembonyama O Stanislas., (2025) “Pediatric Hospital Mortality in the Democratic Republic of Congo: A Multicenter Retrospective Study of Causes and Determinants (2019–2021)”. International Journal of Epidemiology and Public Health Research, 7(4); DOI: 10.61148/2836-2810/IJEPHR/180.
Copyright: © 2025. Abdala Kingwengwe Aimé. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background
Pediatric morbidity and mortality are major indicators for assessing the quality of health services and planning public health interventions. Despite global progress, sub-Saharan Africa and South-East Asia continue to bear the heaviest burden of preventable child deaths. In the Democratic Republic of Congo (DRC), few recent multicenter studies have analyzed the hospital mortality profile of children.
Objective
To describe the clinical profile and determinants of pediatric hospital mortality in five health facilities in the DRC between 2019 and 2021.
Methods
We conducted a multicenter, retrospective cross-sectional study of 146 pediatric deaths recorded in five hospitals across the DRC. Sociodemographic, clinical, and therapeutic variables were analyzed. Proportional mortality rate (PMR), specific mortality rate (SMR), and case fatality rate (CFR) were calculated. Univariate and bivariate analyses were performed using Pearson’s chi-square test, with a significance threshold of p-value<0.05.
Results
The crude hospital mortality rate was 7%. The mean age of deceased children was 3.7 years, with a male-to-female ratio of 1.14. Children under five accounted for 71.2% of deaths. The leading causes of death were malaria (PMR=52.1%; SMR=3.6%), anemia (PMR=21.9%; SMR=1.5%), meningitis (PMR=18.5%; SMR=1.3%), pneumonia (PMR=15.8%; SMR=1.1%), and sepsis (PMR=12.3%; SMR=0.9%). The most lethal conditions were acute kidney injury (CFR=40.6%), meningitis (CFR=15.1%), pneumonia (CFR=11.3%), and malaria (CFR=5.7%). Mortality was significantly associated with age <5 years (p=0.001), admission in April (p=0.008), presence of chronic disease (p=0.005), late consultation (p<0.0001), and length of hospital stay (p<0.0001).
Conclusion
Pediatric hospital mortality in the DRC remains high compared to other sub-Saharan African settings and is predominantly driven by infectious diseases. This study highlights key risk factors, including delayed consultation and the presence of chronic illness, which can inform targeted interventions. Strengthening vaccination coverage, early detection of chronic and non-communicable diseases, and improving diagnostic capacities for congenital anomalies are essential strategies to reduce preventable hospital deaths among children in the DRC.
Pediatric hospital mortality, risk factors, Democratic Republic of Congo
Pediatric morbidity and mortality remain major indicators for evaluating the performance and quality of health systems. Despite a global decline in child mortality over the past two decades, the burden remains disproportionately high in low- and middle-income countries. In 2022, nearly five million children worldwide died before reaching their fifth birthday, equivalent to one death every six seconds, with the majority of these preventable deaths occurring in sub-Saharan Africa and South-East Asia [1].
Hospital mortality data provide crucial insights into the quality of pediatric care. They allow healthcare managers and providers to identify the main causes of death and adjust clinical and public health strategies accordingly. While many countries in sub-Saharan Africa have reported pediatric hospital mortality trends, there is a paucity of multicenter studies in the Democratic Republic of Congo (DRC), where most available data are single-center and often outdated [2–6].
The DRC faces multiple health system challenges, including high prevalence of infectious diseases, delays in health-seeking behavior, limited diagnostic capacities, and insufficient coverage of preventive programs such as immunization. Understanding the clinical patterns and determinants of pediatric hospital mortality in this context is essential for guiding national strategies aimed at reducing preventable deaths and achieving the Sustainable Development Goals (SDGs) related to child survival.
The objective of this study was therefore to provide an updated profile of pediatric hospital mortality across five reference hospitals in the DRC and to identify key risk factors associated with in-hospital deaths among children.
Methods
Study design and setting
We conducted a multicenter, retrospective cross-sectional study based on pediatric deaths recorded between January 2019 and December 2021. Data were collected from five reference hospitals located in four major regions of the Democratic Republic of Congo (DRC):
Study population
The study population included all children aged 1 month to 20 years who were admitted to the pediatric wards of the participating hospitals during the study period and subsequently died. Neonates (0–28 days) and children admitted for severe acute malnutrition were excluded. These exclusions were made because neonatal and malnutrition-related deaths are typically analyzed separately, given their distinct etiological profiles and specialized management protocols.
Sample size and sampling
A total of 2,097 pediatric admissions were recorded across the five hospitals, of which 146 deaths were documented and included in the analysis. All eligible cases during the study period were considered, thus no sampling technique was applied.
Data collection
Data were extracted from hospital records using a standardized questionnaire developed on the KoboCollect platform by the Unit of Prevention and Disease Control at the University of Kindu. Variables collected included:
Definitions of indicators
Data analysis
Data were analyzed using SPSS version 25 and Microsoft Excel 2017. Descriptive statistics were computed as frequencies, percentages, means, and standard deviations. Bivariate analyses were performed using Pearson’s chi-square test to assess associations between independent variables and mortality. A p-value <0.05 was considered statistically significant.
Ethical considerations
Prior authorization was obtained from the administrative boards of all participating hospitals before data collection. Ethical approval was granted by the institutional ethics committee of the University of Kindu. All data were anonymized, and confidentiality was strictly maintained throughout the study.
Table I: Proportional mortality, specific mortality and lethality.
|
Pathologies |
Deaths (n=146) |
Admissions (n=2097) |
TPM |
TSM |
Lethality |
p -value |
|
Malaria |
76 |
1325 |
52.1 |
3.6 |
5.7 |
0.004 |
|
Anemia |
32 |
607 |
21.9 |
1.5 |
5.3 |
0.052 |
|
Meningitis |
27 |
179 |
18.5 |
1.3 |
15.1 |
0.0001 |
|
Pneumonia |
23 |
204 |
15.8 |
1.1 |
11.3 |
0.011 |
|
Septicemia/Sepsis |
18 |
257 |
12.3 |
0.9 |
7.0 |
0.978 |
|
Urinary tract infection |
15 |
223 |
10.3 |
0.7 |
6.7 |
0.884 |
|
Acute kidney injury |
13 |
32 |
8.9 |
0.6 |
40.6 |
0.0001 |
|
Gastroenteritis |
13 |
223 |
8.9 |
0.6 |
5.8 |
0.482 |
|
Intestinal parasitosis |
9 |
147 |
6.2 |
0.4 |
6.1 |
0.678 |
|
ENT infections |
8 |
133 |
5.5 |
0.4 |
6.0 |
0.657 |
|
Bronchiolitis |
6 |
56 |
4.1 |
0.3 |
10.7 |
0.263 |
|
Coma |
5 |
32 |
3.4 |
0.2 |
15.6 |
0.052 |
|
Typhoid fever |
3 |
208 |
2.1 |
0.1 |
1.4 |
N / A |
|
Digestive hemorrhage |
1 |
8 |
0.7 |
0.04 |
12.5 |
N / A |
NA: not applicable
Table I: Sociodemographic, anamnestic, therapeutic and outcomes characteristics of deceased children.
|
Variables |
Frequency (n=146) |
Percentage |
Statistics |
|
Age |
|
|
p -value = 0.199 |
|
1 to 59 months |
104 |
71.2 |
Average = 3.7 years |
|
5 to 10 years |
26 |
17.8 |
|
|
11 to 15 years old |
12 |
8.2 |
|
|
16 to 20 years old |
4 |
2.7 |
|
|
Sex |
|
|
p -value = 0.959 |
|
Female |
68 |
46.6 |
|
|
Male |
78 |
53.4 |
|
|
Months of hospitalization |
|
|
p -value = 0.008 |
|
January |
11 |
7.5 |
|
|
February |
3 |
2.1 |
|
|
March |
6 |
4.1 |
|
|
April |
21 |
14.4 |
|
|
May |
16 |
11.0 |
|
|
June |
10 |
6.8 |
|
|
July |
7 |
4.8 |
|
|
August |
13 |
8.9 |
|
|
September |
18 |
12.3 |
|
|
October |
16 |
11.0 |
|
|
November |
9 |
6.2 |
|
|
December |
16 |
11.0 |
|
|
Chronic disease |
|
|
p -value = 0.005 |
|
Absent |
127 |
87.0 |
|
|
Presents |
19 |
13.0 |
|
|
Consultation deadline |
|
|
p -value = 0.0001 |
|
≤ 3 days |
58 |
39.7 |
Average = 6 days |
|
> 3 days |
88 |
60.3 |
Standard deviation = 3 |
|
Length of stay |
|
|
p -value = 0.0001 |
|
≤ 3 days |
93 |
63.7 |
Average = 5 days
|
|
4 to 7 days |
26 |
17.8 |
|
|
> 7 days |
27 |
18.5 |
Table III: Common Complaints of deceased children.
|
Reasons for consultation |
Frequency (n=146) |
Percentage |
p -value |
|
Fever |
73 |
50.0 |
0.0001 |
|
Dyspnea |
29 |
19.9 |
0.0001 |
|
Physical asthenia |
23 |
15.8 |
0.004 |
|
Convulsions |
22 |
15.1 |
0.0001 |
|
Cough |
19 |
13.0 |
0.453 |
|
Vomiting |
18 |
12.3 |
0.001 |
|
Pallor |
17 |
11.6 |
0.470 |
|
Emission of loose stools |
11 |
7.5 |
0.067 |
|
Loss of consciousness |
8 |
5.5 |
0.002 |
|
Abdominal pain |
7 |
4.8 |
0.01 |
|
Incessant crying |
5 |
3.4 |
0.165 |
|
Headaches |
4 |
2.7 |
N / A |
|
Abdominal bloating |
3 |
2.1 |
N / A |
|
Hustle |
2 |
1.4 |
N / A |
|
Osteoarticular pain |
2 |
1.4 |
N / A |
|
Weight loss |
1 |
0.7 |
N / A |
|
Facial puffiness |
1 |
0.7 |
N / A |
|
Chest pain |
1 |
0.7 |
N / A |
NA: Not applicable
Results
Overall hospital mortality
During the study period, 2,097 pediatric admissions were recorded across the five hospitals. Among these, 146 deaths occurred, corresponding to a hospital mortality rate of 7.0%. The mean age at death was 3.7 years (±2.4), with 71.2% occurring in children under five years (OR=2.4; 95% CI: 1.5–3.9; p=0.001). This distribution is shown in Figure 3, where children under five represented more than two-thirds of all deaths. The male-to-female ratio was 1.14, with no significant difference observed (p=0.959).
Causes of death
Five conditions accounted for more than four out of five pediatric deaths: malaria (52.1%), anemia (21.9%), meningitis (18.5%), pneumonia (15.8%), and sepsis (12.3%). When case fatality was considered, the most lethal conditions were acute kidney injury (CFR=40.6%), meningitis (15.1%), pneumonia (11.3%), and malaria (5.7%). These results highlight that while malaria contributed the largest share of deaths, acute kidney injury, although less frequent, was associated with the highest lethality. These findings are illustrated in Figure 1, which compares the proportional mortality rate and case fatality rate across the leading causes of death.
Temporal distribution
Analysis of the monthly distribution of deaths revealed three distinct seasonal peaks: April–May, September–October, and
December (p=0.008). These peaks coincided with periods of high malaria transmission in the DRC. As shown in Figure 2, mortality curves followed a bimodal pattern, reinforcing the influence of environmental and seasonal factors on pediatric hospital deaths.
Clinical presentation
The most common presenting complaints among deceased children were fever (50%), dyspnea (19.9%), physical asthenia (15.8%), convulsions (15.1%), vomiting (12.3%), loss of consciousness (5.5%), and abdominal pain (4.8%) (all p<0.05). Fever was almost universal and often associated with severe malaria or sepsis, while dyspnea and convulsions reflected the burden of severe respiratory and neurological infections.
Health-seeking behavior and chronic conditions
The average delay before consultation was 6 days (±3). Notably, 60.3% of deceased children presented after more than three days of illness onset (OR=3.1; 95% CI: 1.9–5.2; p<0.0001). Chronic disease was identified in 13% of cases and was significantly associated with mortality (p=0.005). This suggests that both delayed health-seeking behavior and underlying chronic morbidity substantially contributed to the risk of in-hospital death.
Length of hospital stay
The mean duration of hospitalization among deceased children was 5 days. However, the majority of deaths (63.7%) occurred within the first 72 hours of admission (OR=2.9; 95% CI: 1.7–4.8; p<0.0001), reflecting both the severity of cases at admission and delays in accessing care.
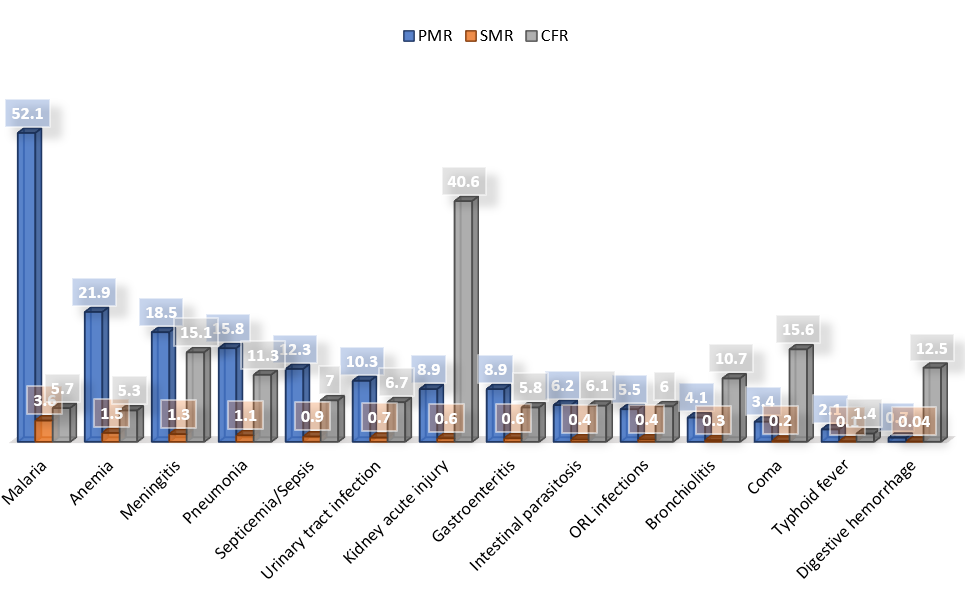
Figure 1: Graphical comparison of mortality indicators
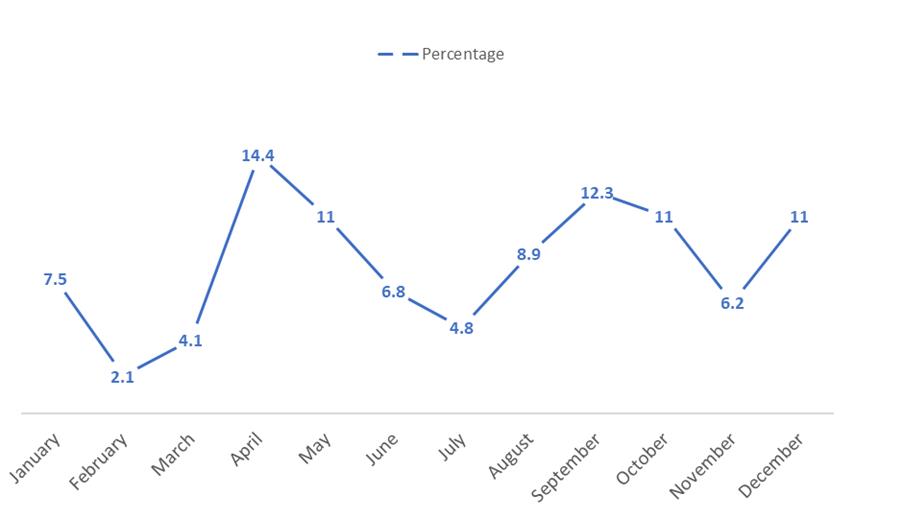
Figure 2: Illustration of the monthly evolution of mortality
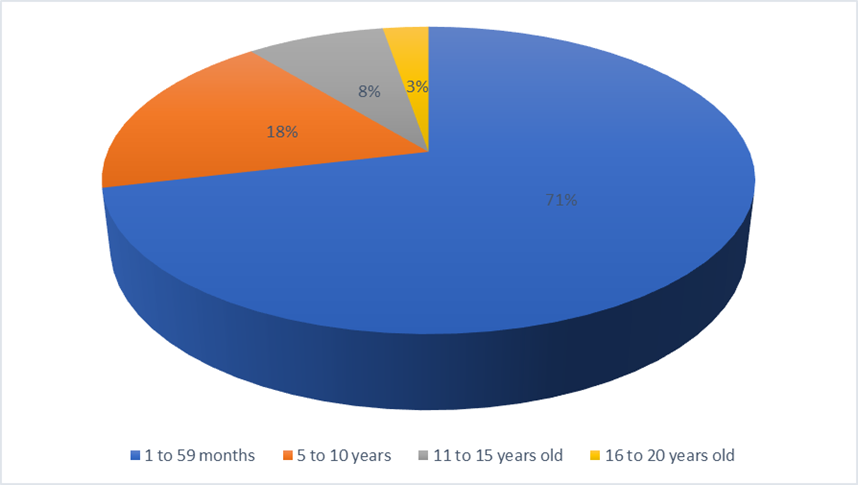
Figure 3: Illustration of the distribution of mortality by age group.
Discussion
This multicenter study conducted in five hospitals across the Democratic Republic of Congo (DRC) provides an updated overview of pediatric hospital mortality and its associated factors. The overall hospital mortality rate of 7.0% observed in our series is higher than the average reported for sub-Saharan Africa, approximately 4% [1]. It close to findings from other single-center studies in the region which have ranged a pediatric mortality between 2.1% and 13.4% with a average of 6.8% [2–11]. These results underscore the urgent need for targeted interventions to reduce preventable pediatric deaths in DRC.
Children under five years accounted for more than 70% of deaths, a proportion consistent with previous African studies [3,5,8]. This reflects the increased vulnerability of this age group to infectious diseases, malnutrition, and limited access to timely care. The predominance of male deaths, although not statistically significant, aligns with some regional findings but remains a subject of debate [4].
The leading causes of death in our study malaria, anemia, meningitis, pneumonia, and sepsis are comparable to those reported in other sub-Saharan African settings [7–9]. Malaria was the most frequent cause of death, reflecting its continued high burden in the DRC. However, when lethality was considered, acute kidney injury, meningitis, and pneumonia were the most fatal conditions, highlighting that frequency and lethality do not necessarily overlap. This observation is important for prioritizing training and resource allocation in pediatric services.
We also identified three seasonal mortality peaks (April–May, September–October and December), which are consistent with high malaria transmission periods in the DRC and similar patterns observed in Gabon, Togo, and other tropical countries [2,8,9]. These findings emphasize the need for seasonal reinforcement of preventive and curative measures, such as intensified malaria control campaigns and improved hospital preparedness during high-risk months.
The common presenting complaints associated with cases of death are fever, dyspnea, physical asthenia, convulsions, vomiting, loss of consciousness and abdominal pain. These reasons recorded in our series corroborate the observation made by Akolly in a Togolese hospital [8]. Fever was among the most reported reason of consultation in Balenga’s series with 92% [9]. The frequency of all these common presenting complaints would be linked to the major causes of hospital mortality in children. They can be included in a model for predicting hospital mortality in children area.
Late consultation emerged as a strong risk factor for mortality, with 60% of children presenting after more than three days of illness onset. This delay has also been reported in Mali, Togo, and Kinshasa [5,8,9]. It reflects sociocultural, economic, and geographic barriers to timely care. Public health strategies should therefore focus on improving parental awareness, reducing financial barriers, and strengthening community-based referral systems.
The contribution of chronic diseases to mortality, although reported in only 13% of cases, was statistically significant. This suggests that many children may have undiagnosed chronic conditions that predispose them to fatal outcomes during acute illnesses. Active screening programs for chronic diseases such as sickle cell disease, HIV, and tuberculosis should be integrated into pediatric care in the DRC.
Another notable finding is that nearly two-thirds of deaths occurred within the first 72 hours of admission, a pattern also observed in studies from Togo and Nigeria [7,8, 11]. This indicates that many children arrive at the hospital in critical condition, and that early management during the first hours of admission is crucial. Strengthening emergency and intensive care units, as well as ensuring availability of essential medicines and diagnostics, is therefore a priority.
Strengths and limitations
The strengths of this study include its multicenter design and the inclusion of hospitals from four major regions of the DRC, which increases its representativeness. However, several limitations should be noted. First, the retrospective design relied on hospital records, which may have incomplete data or misclassified diagnoses. Second, laboratory confirmation was not always available, especially for congenital anomalies and chronic diseases, which may have been underdiagnosed. Third, the absence of neonatal and severe malnutrition cases, excluded by design, limits comparability with studies that include these populations. Despite these limitations, our findings provide valuable insights for policymakers and clinicians in the DRC.
Implications for practice and policy
This study highlights the urgent need to strengthen pediatric care in the DRC. Priorities should include improving vaccination coverage, expanding early detection and management of chronic diseases, reinforcing diagnostic capacities, and implementing timely referral and treatment pathways. Seasonal reinforcement of malaria control and hospital preparedness could significantly reduce preventable deaths. Moreover, investment in pediatric emergency care, with emphasis on the first 72 hours of admission, should be a cornerstone of hospital strategies.
Conclusion
Pediatric hospital mortality in the Democratic Republic of Congo remains high compared to other sub-Saharan African settings and is largely driven by infectious diseases. Children under five years are the most affected, with malaria, anemia, meningitis, pneumonia, and sepsis accounting for the majority of deaths. Acute kidney injury, meningitis, and pneumonia were the most lethal conditions.
Key risk factors identified include young age, delayed consultation, underlying chronic illness, admission during high-transmission months, and early death within 72 hours of hospitalization. These findings highlight the urgent need for targeted interventions, including timely access to care, improved vaccination coverage, early detection of chronic and non-communicable diseases, and enhanced diagnostic and emergency care capacities.
Strengthening hospital preparedness during seasonal peaks and reinforcing pediatric emergency management in the first hours of admission could significantly reduce preventable child deaths in the DRC.
Authors' contribution to the study
Abdala KA: conception, data collection, analysis, and writing. Wete WK: data collection and writing. Shongo YPM: writing and formatting. Shindano ME: conception and writing. Wembonyama OS: writing. All authors reviewed and approved the final version of the manuscript.
Conflicts of interest
No competing interests are associated with this work or with the authors in the context of this study.