International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 5 - Issue 1 - 2025
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
S. Kalpana*, K. Narayanasamy** and Jasmine S Sundar***
*Research Officer **Vice Chancellor*** Assistant Professor
The Tamil Nadu Dr.MGR Medical University, Chennai, India.
*Corresponding author: S. Kalpana, The Tamil Nadu Dr.MGR Medical University, Chennai, India.
Received: August 15, 2025 | Accepted: August 25, 2025 | Published: August 28, 2025
Citation: S. Kalpana, K. Narayanasamy and Jasmine S Sundar., (2025) “Impact of Climate Change on Human Health: A Systematic Review”. International Journal of Epidemiology and Public Health Research, 7(1); DOI: 10.61148/2836-2810/IJEPHR/164.
Copyright: © 2025. S. Kalpana. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Climate change is an escalating global crisis with profound public health consequences. This systematic review synthesizes evidence from 2005 to 2025 regarding both direct and indirect health effects. We screened 312 records from major databases and included 6 high-quality studies spanning both global and Indian contexts. Health impacts identified included increased heat-related mortality, respiratory and cardiovascular disease, infectious illnesses, mental health effects, and accelerated biological aging. Particularly vulnerable populations such as the elderly, children, low-income groups, and informal sector workers were disproportionately affected. The findings emphasize the urgent need for climate-resilient health systems, improved surveillance of environmental exposures, mental health integration, and targeted heat action plans.
Climate change, health, heat waves, mental health effects
Climate change, characterized by rising temperatures, erratic rainfall, and extreme weather events, has emerged as a critical driver of global morbidity and mortality [1]. The Intergovernmental Panel on Climate Change (IPCC) has projected with high confidence that climate-related health burdens will disproportionately affect low- and middle-income countries, including India [2]. Direct health consequences include heat stress and heatstroke, while indirect effects encompass worsened air quality, food insecurity, and increased spread of vector-borne and waterborne diseases [3,4].
Over the last decade, growing evidence has linked climate extremes with noncommunicable diseases (NCDs) such as cardiovascular diseases, respiratory illnesses, and adverse mental health outcomes [5]. Populations most at risk include the elderly, children, persons with chronic conditions, and those residing in climate-sensitive geographies such as coastal zones and urban heat islands [6].
Despite increased attention, there remains a lack of consolidated evidence linking specific climate factors (e.g., temperature rise, pollution, humidity) to health outcomes in vulnerable populations. Therefore, this review aims to systematically evaluate recent studies on the health consequences of climate change and highlight gaps for public health preparedness.
2. Methods
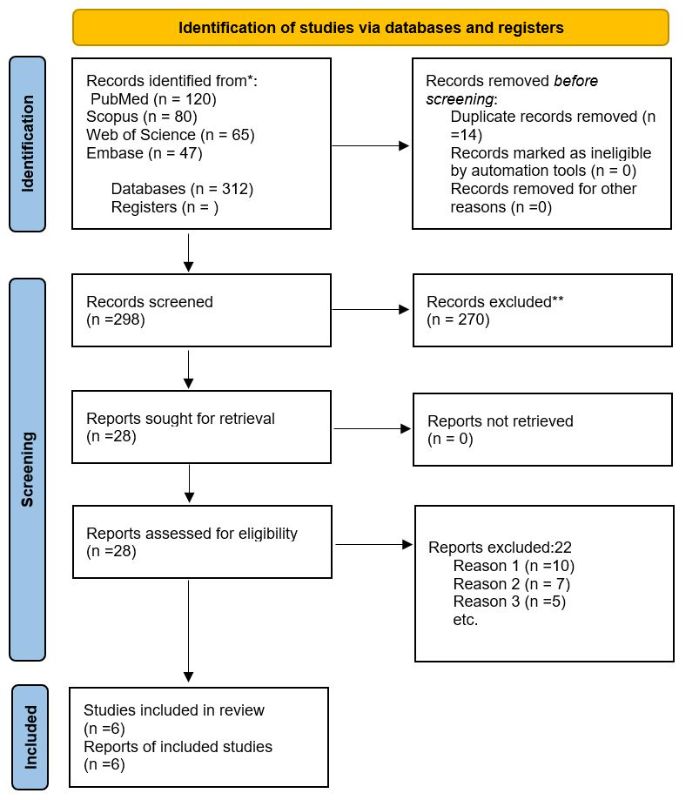
This systematic review followed PRISMA 2020 guidelines and was registered with PROSPERO. A total of 312 records were identified through database searching. After removing duplicates (n = 14), 298 records were screened by title and abstract. Of these, 270 were excluded. The remaining 28 full-text articles were assessed for eligibility, and 6 studies were included in the final synthesis. The detailed screening process is presented in the PRISMA 2020 flow diagram (Figure 1)
2.1 Eligibility Criteria
We included studies that:
Exclusion criteria included editorials, conference abstracts, animal studies, and modeling-only studies without health outcomes.
2.2 Search Strategy
A literature search was conducted in PubMed, Scopus, Web of Science, Embase, and Google Scholar using combinations of keywords and MeSH terms including:
"Climate change", "Heatwaves", "Air pollution", "Health effects", "Mortality", "Infectious diseases", "Mental health", and "Cardiovascular diseases".
2.3 Data Extraction and Risk of Bias Assessment
Data extracted included: authors, year, country, population, exposure variable, health outcome, and findings. Quality appraisal was conducted using the Newcastle-Ottawa Scale.
Results
Overview
Out of 312 articles screened, 6 met the inclusion criteria. The included studies spanned both global (n=2) and Indian (n=4) contexts. A narrative synthesis was performed due to heterogeneity in study design and outcomes.
Health Impacts Identified
Table 1. Summary of Included Studies and Health Impact Findings
|
Study |
Country |
Study Design |
Population |
Exposure |
Health Outcome |
Key Findings |
|
[7] The Lancet Countdown (2020) |
Global |
Review |
Older adults |
Heat |
Mortality |
167% rise in heat-related deaths (1990–2020) |
|
[8] US Cohort Study |
USA |
Cohort |
Adults |
Chronic Heat |
Biological Aging |
~14 months accelerated aging, comparable to smoking |
|
[9] Indian Environmental Study |
India |
Ecological |
Children |
PM2.5 & Temperature |
Respiratory Disease |
Increased asthma, COPD, and childhood stunting |
|
[10] Rural Heat-Infection Study |
India |
Time Series |
General Population |
Extreme Heat |
Infectious Disease |
4.7% rise in intestinal infections per extreme heat day |
|
[11] Indian Mental Health Survey |
India |
Cross-Sectional |
Low-income adults |
Wet Bulb Temperature |
Mental Health |
Heat stress linked to depressive symptoms |
|
[12] Informal Workers Heat Risk |
India |
Observational |
Informal workers |
Heatwaves |
Occupational Health |
Higher hospitalization and mortality during heatwaves |
A total of six studies were included in this systematic review, comprising a mix of cohort, cross-sectional, ecological, and time-series designs. Geographically, three studies were conducted in India and three in high-income countries or globally. The population groups studied included children, older adults, low-income populations, and informal sector workers — all particularly vulnerable to climate-related exposures.
Heat exposure was the most frequently examined climatic factor, reported in four studies. Health outcomes observed across these studies included:
The data are summarized in Table 1, and the distribution of studies by health outcome is visualized in Figure 1.
Discussion
Summary of Findings
The studies confirm that climate change leads to serious adverse health outcomes across multiple domains. Heat-related deaths, respiratory illnesses, mental health disorders, and infections are closely tied to rising temperatures and air pollution levels [7–12].
Justification and Comparison with Literature
Our findings support earlier conclusions by Patz et al. [1] and Haines & Ebi [3], who highlighted climate-sensitive disease burdens. Watts et al. emphasized inadequate preparedness of global health systems [4], which remains evident, especially in low-resource settings.
A 2021 study by Kumar et al. confirmed high vulnerability in Indian districts, especially among women and children [6]. The recent findings extend this by linking climate to biological aging and mental health, previously underexplored.
Policy Implications
This evidence emphasizes the need for:
Limitations
Future Directions
Conclusion
Climate change is an urgent public health threat with wide-ranging consequences for human health. The review reveals strong associations between climate variables such as rising temperatures, extreme heat, and air pollution and multiple health outcomes including heat-related mortality, respiratory illnesses, infectious diseases, mental health disturbances, and indicators of biological ageing. Vulnerable populations, particularly children, the elderly, low-income communities, and informal sector workers, bear a disproportionate burden due to limited adaptive capacity and exposure to adverse environmental conditions. The findings highlight the urgent need for integrated public health policies tailored to climate vulnerabilities, including the development of heat action plans, climate-informed disease surveillance, urban cooling strategies, and targeted mental health support. Occupational protections for at-risk workers and investments in resilient infrastructure must also be prioritized. Furthermore, interdisciplinary research incorporating longitudinal and geospatial approaches is essential to better understand causal pathways and emerging risks such as neurodegenerative conditions, fertility decline, and chronic disease progression. Strengthening adaptive capacity and public health infrastructure especially in low- and middle-income settings like India is imperative to safeguard health in the face of accelerating climate change.
Conflict of interest: Nil