International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 5 - Issue 1 - 2025
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
Eduardo Toledo de Aguiar*, Daniele D. Carvalho, Henrique Capistrano dos Santos, Igor Assumpção Baisch, Danúbia Cristina da Silva Godoy, Michel Nasser, Vascular Space
Avenida Angélica, 2447, room 51 01227-200 São Paulo Brazil.
*Corresponding author: Eduardo Toledo de Aguiar, Avenida Angélica, 2447, room 51 01227-200 São Paulo Brazil.
Received: June 15, 2025 |Accepted: July 26, 2025 |Published: August 04, 2025
Citation: Eduardo Toledo de A, Daniele D. C, Henrique Capistrano dosS, Igor Assumpção B, Danúbia Cristina da Silva G, Michel N, Vascular S. (2025) “Ultrasound-Guided Foam Sclerotherapy for the Treatment of Venous Ulcers: Immediate and 5-Year Results”. International Journal of Epidemiology and Public Health Research, 6(4); DOI: 10.61148/2836- 2810/IJEPHR/135.
Copyright: © 2025. Eduardo Toledo de Aguiar. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited., provided the original work is properly cited.
Introduction. Venous ulcers are a serious public health issue. Its prevalence is approximately 1% globally, reaching 3% in the population over 65 years old in the United Kingdom. It is estimated that in Brazil there are approximately 3.1 million patients. Compression therapy associated with dressings is the most common treatment, but the healing delay and ulcer recurrence are the problems. Immediate treatment of chronic venous disease in an outpatient setting may speed up resolution and decrease recurrence. Foam sclerotherapy is a quick and simple alternative.
Objective. To evaluate the outcome of patients classified as C5/C6 (CEAP classification) treated with foam sclerotherapy. The main outcome is wound healing, while secondary outcomes include gender differences, factors influencing healing, and recurrence of venous disease and/or ulcer.
Method. Clinical, retrospective study based on the records of C5/C6 patients (CEAP classification) during the period from 2004 to 2014. Inclusion criteria were records of patients classified as C5 or C6 (CEAP classification) with primary or secondary etiology and venous reflux detected by duplex ultrasound. Exclusion criteria were patients with incomplete diagnostic data, deep venous system obstruction, patients not treated with foam sclerotherapy, and follow-up less than 30 days. All were treated with endovenous injection of polidocanol foam (1% or 3%) prepared by the Tessari method.
Result. After exclusions, 221 records remained, being 172 female and 49 male patients. The follow-up time ranged from 1 to 185 months (average: 26.22 months). There was a significant difference in the average age between women and men: women are 12 years older. The percentage of healed ulcers is lower in men; healing time ranged from less than 30 days to more than 360 days; patients with a history of ulcer for more than 7.5 years are 2.4 times more likely not to heal; the chance of a male patient not healing is 3.85 times higher than a woman with similar age characteristics, clinical stage of the limb and secondary CVD; 50% of patients presented wound recurrence and/or need for re-treatment of CVD at 51 months.
Conclusion. The treatment of venous insufficiency should be done early, together with the venous ulcer treatment. Foam sclerotherapy is quick, safe, and suitable for outpatient treatment. Factors hindering healing include male gender, ulcer history time, and secondary etiology. The high recurrence requires follow-up and periodic reassessment of patients to keep their legs healthy in the long term.
Public health; Venous Ulcers
Venous ulcers are a serious public health issue. Their prevalence is approximately 1% globally, reaching 3% in the population over 65 years of age in the United Kingdom.1 Scuderi et al. (2001) conducted a study in rural and urban populations of Campinas and Sorocaba (Brazil) and found a prevalence of venous ulcers (CEAP classification C5/C6) of 2%.2 Based on the Brazilian adult population (156,454,011 voters) and this prevalence, it is estimated that approximately 3.1 million Brazilians suffer from venous ulcers, with recurrence being an aggravating factor.3
Treatment of venous ulcers typically involves compression therapy associated with open wound dressings. Including treatment for venous insufficiency, such as venous ablation, can accelerate healing and prevent recurrence.4 Outpatient treatment using an effective and safe technique can treat many patients classified as C5/C6 and avoid hospital admissions. Ultrasound-guided foam sclerotherapy meets these criteria and has been successfully used to treat Chronic Venous Disease (CVD).5
Objective
The aim of this study is to evaluate the treatment outcomes of patients classified as C5/C6 (CEAP classification) using ultrasound-guided foam sclerotherapy. The primary outcome is wound healing, while secondary outcomes include gender differences, factors influencing healing, and recurrence of venous disease and/or ulcer.
Method. Study design
This is a retrospective clinical study. A database was created with information such as patient name, date of birth, gender, age, associated diseases, wound duration, CEAP classification, ultrasound mapping data, etiology, treatment dates and final evaluation, and treatment outcomes.
Data source
Data were obtained from medical records of consecutive patients treated in a private service specializing in CVD using ultrasound- guided foam sclerotherapy, from January 2004 to December 2014. Inclusion and exclusion criteria
The inclusion criteria were medical records of patients classified as C5 or C6 (CEAP classification), with primary or secondary etiology and venous reflux detected by duplex ultrasound. Exclusion criteria were: patients with incomplete diagnostic data, obstruction of the deep venous system, patients not treated with ultrasound-guided foam sclerotherapy and follow-up of less than 30 days.
Treatment technique
Patients were treated with intravenous injection of polidocanol foam (1% or 3%) prepared by the Tessari method. The injected volume varied between 10 and 15 mL per limb, with a maximum of 20 mL per patient. The average number of sessions was 2.02 ±
1.08. Initially, 2-3 punctures were made in the limb; from March 2010 onwards, the puncture was made directly in the great or small saphenous vein and, if these were normal or absent, in dilated and insufficient tributaries. All patients signed an informed consent form.
Statistical analysis
The profile of the patients was analyzed by comparing age and comorbidities between genders, using the t-test for continuous variables and the Chi-square/Fisher test for categorical variables (significance 0.05).
Clinical stage, etiology and healing were compared between genders using Chi-square/Fisher (significance 0.05). Logistic regression evaluated factors that influence healing (age, gender, comorbidities, clinical stage and etiology). ROC analysis determined the cutoff point for the time of ulcer history before treatment. Healing time was compared between genders using the Mann-Whitney test (significance 0.05). Wound recurrence was analyzed with Kaplan-Meier curves, comparing genders, using Log Rank, Breslow and Tarone-Ware tests (significance 0.05).
Results
A total of 233 medical records of patients classified as C5 and C6 were found. Twelve medical records were excluded: 6 due to treatment abandonment before 30 days, 3 due to incomplete data, 2 due to obstruction of the deep venous system revealed during previous ultrasound venous mapping, and one for not having been treated with ultrasound-guided foam sclerotherapy. After these exclusions, 221 medical records remained, 172 of which were female patients and 49 were male patients. The follow-up time of the patients ranged from 1 to 185 months, with a mean of 26.22 months.
Table 1 shows the profile of patients according to gender. A significant difference in mean age was observed between women and men: women, on average, are 12 years older than men. There was no significant difference in comorbidities between genders.
|
Table 1: Patient profile |
||||
|
Characteristics |
Female |
Male |
p-value |
Test used |
|
N (%) |
172 (78%) |
49 (22%) |
|
|
|
Age (mean ± standard deviation) |
63 ± 11,5 |
51,4 ± 13,6 |
0,000 |
t-Test |
|
Associated Disease (any) |
|
|
0,225 |
|
|
No |
71 (41%) |
25 (51%) |
|
Chi-square |
|
Yes |
101 (59%) |
24 (49%) |
|
|
|
DM |
|
|
0,687 |
Fisher's exact |
|
No |
164 (95%) |
48 (98%) |
|
|
|
Yes |
8 (5%) |
1 (2%) |
|
Chi-square |
|
HTN |
|
|
0,240 |
|
|
No |
89 (52%) |
30 (61%) |
|
Fisher's exact |
|
Yes |
83 (48%) |
19 (39%) |
|
|
|
Hypothyroidism |
|
0,212 |
Fisher's exact |
|
No |
163 (95%) |
49 (100%) |
t-Test |
|
Yes |
9 (5%) |
0 (0%) |
|
|
Obesity |
|
1,000 |
Chi-square |
|
No |
166 (97%) |
47 (96%) |
|
|
Yes |
6 (3%) |
2 (4%) |
|
A total of 276 lower limbs were treated, of which 85 were classified as C5 and 191 as C6. Venous disease was classified as secondary in 11 limbs (4%), all with recanalized deep venous system with reflux. Table 2 shows the distribution of limbs by gender in relation to severity and etiology of chronic venous disease, and no significant differences were observed.
|
Table 2: Distribution of members by gender in relation to severity and etiology of CVD |
||||
|
|
Female |
Male |
p-value |
Test used |
|
Lower Limbs |
|
|
0,64 |
Chi-Square |
|
C5 |
68 (31%) |
17 (28%) |
|
|
|
C6 |
148 (69%) |
43 (72%) |
|
|
|
Secondary CVD |
|
|
0,709 |
Fisher's exact |
|
No |
208 (96%) |
57 (95%) |
|
|
|
Yes |
8 (4%) |
3 (5%) |
|
|
Of the total number of limbs treated, 199 belonged to patients with associated comorbidities: arterial hypertension (121), diabetes mellitus (34), hypothyroidism (15), obesity (10), coronary artery disease (8), vasculitis (7), breast cancer (3) and Parkinson's disease
(1). Table 3 shows the percentage of healing by gender. A significant difference was observed between men and women: the percentage of healed ulcers was lower in men compared to women. One patient included in the study was followed for more than 60 days. The wound area decreased significantly, but was lost to follow-up, and there is no data in the medical records indicating complete healing.
|
Table 3: Distribution of members by gender in relation to wound healing. |
|||
|
|
Feminino |
Masculino |
|
|
Healing |
|
0,003 |
Chi-Square |
|
Scarred |
178 (82%) |
39 (65%) |
|
|
Unhealed |
37 (17%) |
21 (35%) |
|
|
Not informed |
1 (0%) |
0 (0%) |
|
The time for ulcer healing ranged from less than 30 days to more than 360 days (Figure 1).
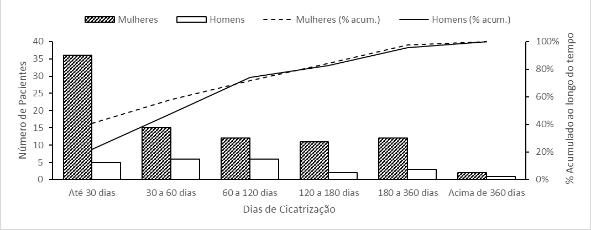
Figure 1: Healing time according to patient gender.
One patient with a circumferential wound in the lower third of her leg took 2 years to heal after sclerotherapy, and she maintained compression therapy throughout this period. Table 1 shows the number of patients who healed, the time for healing, and the difference between men and women.
|
Table 1: Healing time of venous wounds in relation to gender. |
|||
|
Healing Time (days) |
Total (N = 111) |
Women (N = 88) |
Men (N = 23) |
|
Up to 30 days |
41 (36,9%) |
36 (40,9%) |
5 (21,7%) |
|
30 to 60 days |
21 (18,9%) |
15 (17%) |
6 (26,1%) |
|
60 to 120 days |
18 (16,2%) |
12 (13,6%) |
6 (26,1%) |
|
120 to 180 days |
13 (11,7%) |
11 (12,5%) |
2 (8,7%) |
|
180 to 360 days |
15 (13,5%) |
12 (13,6%) |
3 (13%) |
|
Over 360 days |
3 (2,7%) |
2 (2,3%) |
1 (4,3%) |
There was no statistical difference between the mean healing times for men and women (Table 4).
|
Table 4: Mean and standard deviation of venous wound healing time in relation to gender. |
|||||
|
|
Total (N = 111) |
Women (N = 88) |
Men (N = 23) |
p-valor |
Teste carried out |
|
Healing time (days), mean ± standard deviation |
91,1 ± 103,6 |
90,1 ± 104,6 |
94,7 ± 102 |
0,648 |
Mann-Whitney |
We sought to establish the relationship between the time of history of venous ulcers until the time of treatment and healing. The ROC curve was constructed, which establishes the relationship between sensitivity and specificity in the study of the time from wound to treatment in relation to healing. The statistical test evaluates whether the area under the curve is different from 0.5, and this test does not reject the hypothesis (Figure 2). This indicates that the cutoff point found may be fragile, without discriminatory power (Table 2).
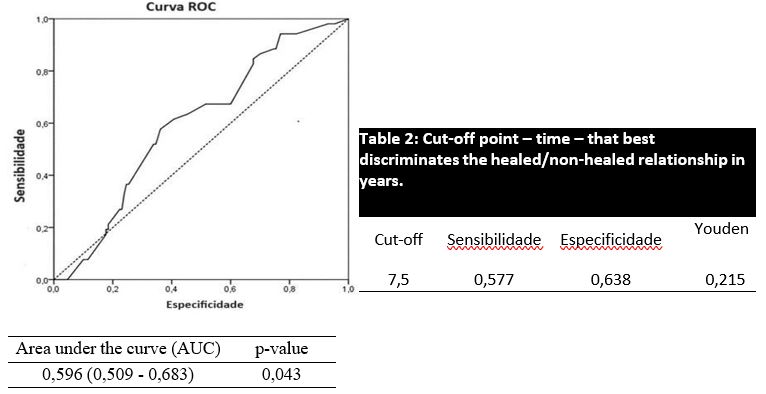
Figure 2: ROC curve: relationship between sensitivity and specificity in the study of wound healing time
Considering the cutoff point found, it is possible to state that patients with ulcers for more than 7.5 years are 2.408 times (1.249- 4.642) more likely to not heal than patients with less than 7.5 years (Table 5).
|
Table 5: Relationship between wound healing time |
|||||
|
Wound Time (years) |
Healing |
|
|
|
|
|
|
|
Total |
Odds Ratio |
p-value |
|
|
|
Scarred |
Unhealed |
|
|
|
|
< 7,5 |
83 (64%) |
22 (42%) |
105 |
1* |
|
|
≥ 7,5 |
47 (36%) |
30 (58%) |
77 |
2,408 (1,249 - 4,642) |
0,009 |
|
Total |
130 |
52 |
182 |
|
|
Univariate and multivariate analyses revealed other factors that influence healing: gender, clinical stage and etiology (primary and secondary). Patients with healed ulcers (stage C5) are more likely to remain without a wound, while patients with secondary etiology have greater difficulty in healing. The chance of a male patient not healing is 3.85 times greater than that of a woman with similar characteristics of age, clinical stage of the limb according to the CEAP classification and secondary CVD (Table 3).
Table :3 Univariate and multivariate analysis of factors influencing healing
Univariate Analysis Multivariate Analysis (Non-Healing)
|
|
|
|
|
Test Used o |
|
OR (IC95%) |
|
|
|
Characteristics |
Healed |
Not Healed |
p-value |
OR |
|
|
p-value |
|
|
|
|
|
|
|
Inferior |
Superior |
|
|
|
N (%) |
217 (79%) |
58 (21%) |
|
|
|
|
|
|
|
Age (mean ± standard deviation) |
60 ± 12,9 |
62,6 ± 12,3 |
0,179 |
Teste t |
1,030 |
1,003 |
1,058 |
0,028 |
|
Gender |
|
|
0,003 |
Qui- quadrado |
|
|
|
|
|
Female |
178 (82%) |
37 (64%) |
|
|
1** |
|
|
|
|
Male |
39 (18%) |
21 (36%) |
|
|
3,848 |
1,783 |
8,301 |
0,001 |
|
Associated Disease (any)* |
|
|
0,090 |
Qui- quadrado |
|
|
|
|
|
No |
98 (45%) |
19 (33%) |
|
|
|
|
|
|
|
Yes |
119 (55%) |
39 (67%) |
|
|
|
|
|
|
|
Lower Limbs |
|
|
0,000 |
Qui- quadrado |
|
|
|
|
|
C5 |
80 (37%) |
5 (9%) |
|
|
1** |
|
|
|
|
C6 |
137 (63%) |
53 (91%) |
|
|
5,758 |
2,098 |
15,802 |
0,001 |
|
Secondary CVD |
|
|
0,000 |
Exato de Fisher |
|
|
|
|
|
No |
214 (99%) |
50 (86%) |
|
|
1** |
|
|
|
|
Yes |
3 (1%) |
8 (14%) |
|
|
13,917 |
3,161 |
61,284 |
0,000 |
|
DM |
|
|
0,470 |
Exato de Fisher |
|
|
|
|
|
No |
206 (95%) |
57 (98%) |
|
|
|
|
|
|
|
Yes |
11 (5%) |
1 (2%) |
|
|
|
|
|
|
|
HTN |
|
|
0,472 |
Qui- quadrado |
|
|
|
|
|
No |
120 (55%) |
29 (50%) |
|
|
|
|
|
|
|
Yes |
97 (45%) |
29 (50%) |
|
|
|
|
|
|
|
Hypothyroidism |
|
|
0,705 |
Exato de Fisher |
|
|
|
|
|
No |
209 (96%) |
55 (95%) |
|
|
|
|
|
|
|
Yes |
8 (4%) |
3 (5%) |
|
|
|
|
|
|
|
Obesity |
|
|
1,000 |
Exato de Fisher |
|
|
|
|
|
No |
208 (96%) |
56 (97%) |
|
|
|
|
|
|
|
Yes |
9 (4%) |
2 (3%) |
|
|
|
|
|
|
*evidence of systemic inflammatory disease: 7 patients **reference categories
Figure 3 shows the recurrence and/or need for retreatment of CVD. It was found that 50% of patients presented wound recurrence and/or need for retreatment of CVD after 51 months, with no significant difference between women (after 51 months) and men (after 48 months).
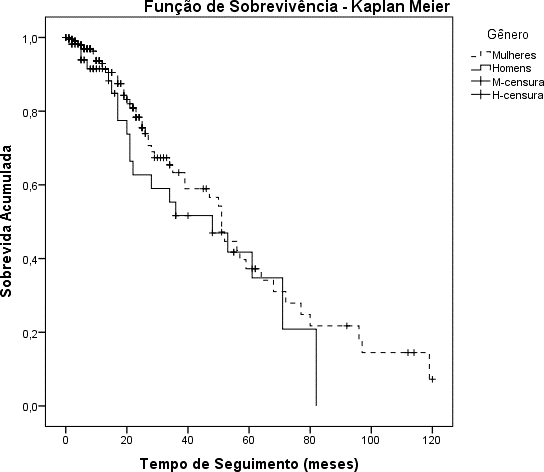
|
p-valor |
|
|
Log Rank (Mantel-Cox) |
0,168 |
|
Breslow (Generalized Wilcoxon) |
0,167 |
|
Tarone-Ware |
0,166 |
Figure 3: Survival time free of venous wound and/or retreatment.
Discussion
Ultrasound-guided foam sclerotherapy (UGFS) has been used for the treatment of Chronic Venous Disease in this service since 2004, covering all patients classified as C2 to C6 in the CEAP classification. This approach was chosen due to the practicality, speed and safety of the method, in addition to being an outpatient treatment.6 Venous ulcers affect millions of people in Brazil, as mentioned above. Compression therapy combined with wound care is the most common technique, but recent studies have not concluded that compression therapy alone improves the quality of life of patients with venous ulcers.7 This reinforces the importance of studies that seek regional solutions to accelerate healing and prevent recurrence.
Treating venous disease through conventional surgery has been shown to reduce ulcer healing time and decrease recurrence.8 In the United Kingdom, a randomized clinical trial studied the efficacy of early venous ablation in ulcer healing, and UGFS was the most widely used method due to its safety, speed, and outpatient nature.9 The data from this study are consistent with other publications regarding the higher prevalence of women and the similar distribution of associated diseases between genders. There was a difference in relation to chronic venous disease of secondary etiology: Pugina et al. (2021) found a rate of 14% of cases of secondary etiology in Brazil, closer to European data.4,10
In this study, the frequency was lower, at 3.9%. According to the literature, important factors for venous ulcer healing include secondary etiology, clinical stage (C6) and recurrent ulcers. This study found no notable differences in relation to other publications.3,11
An important aspect of this study is the significant difference in mean age between men and women, with men being, on average, 12 years younger. Publications generally report the mean age of C6 patients as 60 years, with no gender differences as observed here.12 Furthermore, 17.1% of women and 35% of men did not have their wounds healed, a significant difference that was not found in other studies consulted.
These data suggest a lack of knowledge about CVD: patients with a primary etiology often do not seek early treatment and men, in particular, seek treatment late. Other factors include poor adherence to compression therapy and a sedentary lifestyle. Multidisciplinary care is essential for better long-term outcomes.13 Venous ulcers take a long time to heal, ranging from 30 to over 360 days. This study revealed that 80% of wounds healed within six months, similar to other studies.14 The mean healing time was 91.1± 103.6 days, with no difference between men and women. Associated diseases, such as hypertension, diabetes, and rheumatologic diseases, influence healing, suggesting a mixed etiology of the wound due to microangiopathy. Venous ulcers are chronic and recurrent, with patients alternating between open and healed ulcers. The history of venous ulcers before treatment was analyzed to verify its influence on healing. The ROC curve showed that the AUC is not different from 0.5, indicating a weak cutoff point. The best Youden index was 7.5 years. Patients with a history of wounds greater than 7.5 years have greater difficulty healing. In the literature, the difference between first-occurring and recurrent ulcers is a predisposing factor for non-healing.14 Abbade et al. demonstrated that a time since the first venous wound greater than 2 years is a factor for non-healing and recurrence.15
Univariate and multivariate analyses highlighted three main factors: male gender, clinical stage, and secondary etiology. Men seek treatment at more advanced stages of the disease; secondary etiology, such as post-thrombotic syndrome, causes more severe and difficult-to-correct venous hypertension, requiring endovascular or surgical restoration of the deep venous system.16 Limited mobility of the tibiotarsal joint also aggravates venous hypertension.17
The study showed that 50% of patients required retreatment after 51 months, with no difference between genders. Wound or CVD recurrence is high, and patients should be closely followed. This result is comparable to others in the literature.18 Criticism of ultrasound-guided foam sclerotherapy is the high rate of recanalization of the great saphenous vein, but studies indicate that recanalization does not influence the recurrence rate.19
Conclusion
Treatment of venous insufficiency should be performed early, together with that of venous ulcers. Ultrasound-guided foam sclerotherapy is fast, safe and suitable for outpatient treatment. Factors that hinder healing include male gender, history of venous wound and secondary etiology. High recurrence requires monitoring and periodic reassessment of patients to maintain healthy legs in the long term.