International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 9 - Issue 1 - 2026
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
Arati C. Koregol1, Nagaraj B. Kalburgi1, Uzma Parveen Sulthana1*, Anjaly Roy1
1P.M.N.M. Dental College and Hospital, India.
*Corresponding author: Uzma Parveen Sulthana, 1P.M.N.M. Dental College and Hospital, India.
Received: June 20, 2025
Accepted: June 30, 2025
Published: July 08, 2025
Citation: Arati C. Koregol, Nagaraj B. Kalburgi, Uzma P Sulthana, Roy A., (2025) “Assessing the Synergistic Benefits of Low-Level Laser Therapy (LLLT) and Photodynamic Therapy (PDT)as Adjuncts to Scaling and Root Planning in Chronic Periodontitis”. International Journal of Epidemiology and Public Health Research, 6(5); DOI: 10.61148/2836-2810/IJEPHR/152.
Copyright: © 2025. Uzma Parveen Sulthana. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited., provided the original work is properly cited.
Introduction:
Low level laser therapy (LLLT) promotes wound healing, reduces pain, and suppresses inflammation by affecting mitochondrial activity, increasing ATP production, and modulating immune responses. LLLT enhances collagen synthesis, growth factor releases without causing thermal effects. Photodynamic therapy (PDT) uses visible light, a nontoxic photosensitizer, and oxygen to produce singlet oxygen and reactive agents that selectively kill target cells and bacteria without harming distant tissues. Green photosensitizers, such as indocyanine green (ICG), are now available used with diode laser.
Objective
To evaluate, compare and correlate Plaque index, Gingival index, Sulcular bleeding index, Pocket probing depth, Clinical attachment loss at baseline,1 and 3 months after non-surgical periodontal therapy (NSPT)alone and NSPT along with LLLT and PDT.
Methodology:
25 subjects (Split-mouth study) aged 30-60 years were selected. Each quadrant categorized into control group (SRP alone; two quadrants per patient), test group 1 (SRP + LLLT), and test group 2 (SRP + PDT).
Results>
Test groups showed significantly reductions in PI, GI, SBI, PPD, and CAL at 1 and 3 months compared to control group. (p<0.001)
Conclusion:
PDT using indocyanine green as dye and LLLT as an adjunct to SRP was significantly more effective than SRP alone.
Periodontitis is a microbially associated host-mediated inflammatory disease that results in the loss of periodontal attachment. Inflammation is caused by a dysbiotic ecological shift in the microbial biofilm, which is strongly associated with teeth and interacts with the human immune system. Periodontitis affects more than 65% of individuals globally, making it one of the most prevalent diseases. Periodontitis can be successfully controlled using both surgical and non-surgical scaling and root planing (SRP) techniques, as well as with appropriate biofilm management and periodontal maintenance therapy (PMT).1,2
To overcome shortcomings of SRP and further reduce the subgingival bacterial burden, photodynamic therapy (PDT) has been suggested as a helpful addition. Three nontoxic components are essentially used in photodynamic treatment (PDT): oxygen, nontoxic photosensitizer, and visible light. The photosensitizer (photoactivatable material) that attaches itself to the target cells activates them when light is applied. Once the photosensitizer is triggered, reactive chemicals such as singlet oxygen are produced, which are extremely detrimental to some bacteria and cells. The cytotoxic product, usually singlet oxygen, cannot travel more than 0.02 mm after synthesis.2 Therefore, PDT wouldn't endanger distant organs, cells, or molecules. Two PDT dyes that are commonly used are methylene blue and toluidine blue. But now that green photosensitizers, such as indocyanine green (ICG), are available, the dye was successfully activated by employing ICG between 810 and 940 nm.3
Low-level laser therapy (LLLT) or photobiomodulation is advised due to its anti-inflammatory, wound-healing, and pain-relieving properties.4 It has been proposed that LLLT can promote collagen synthesis, angiogenesis, and growth factor release, all of which ultimately speed up wound healing, and that modifies cellular activity by influencing the mitochondrial respiratory chain or membrane calcium channels. Through its action on the mitochondrial respiratory chain, 5LLLT increases adenosine triphosphate generation, which in turn promotes fibroblast proliferation, growth factor release, and collagen synthesis.6 By modifying the local immunological response and lowering the synthesis and release of specific proinflammatory cytokines, including prostaglandin E, interleukin-1b (IL-1b), and tumor necrosis factor alpha, LLLT reduces inflammation in periodontal tissue.2,7 The advantages of LLLT and photodynamic therapy for individuals with chronic periodontitis, however, are not well documented by literature.
Therefore, this study aims to explore the effectiveness of LLLT and Photodynamic Therapy using Indocyanine green in chronic periodontitis.
Materials and Methods:
A total of 25 subjects; with Chronic Periodontitis aged between 30-60years, were selected from the outpatient department, department of Periodontics, P.M.N.M. Dental College and Hospital, Navanagar, Bagalkote.
With the following inclusion criteria: Subject willing to participate in the study and given written consent for the same, Patients aged 30-55 years, Patients diagnosed as periodontitis having atleast PD ≥ 5 mm in each quadrant, Minimum number of 20 teeth present, Patients who have not received any antimicrobial treatment for the past three months.
Following patients were excluded from the study: Patients on any systemic antibiotics, anti-inflammatory, hormonal therapy or Corticosteroid therapy for any other reasons which is known to affect the periodontal status, Subjects immunosuppressed by medication, Periodontal therapy within the past 6 months, Subjects with systemic disease and condition, Pregnant and lactating women, Subjects who are using chemical plaque control agents, Subjects having other infections or pathology in oral cavity other than periodontitis.
Following a thorough explanation of the technique, the patients provided written informed consent, and the study protocol was approved by the institutional ethics committee. After receiving advice on proper oral hygiene, each patient had full-mouth scaling and root planing (SRP) performed with manual and ultrasonic instruments.
The present Study was carried out on 25 patients using a split-mouth study design. Two quadrants make up the control group (SRP only), test groups 1 (SRP + LLLT), and test groups 2 (SRP + PDT) for each patient. Full-mouth scaling and root planing (SRP) was performed on each patient using hand and ultrasonic instruments. A lidocaine-adrenaline ratio of 1:200,000 was used to anesthetize the test site. Test groups 1 and 2 sites with PD ≥ 5 mm were then administered a single LLLT and PDT episode, respectively. For areas where PD < 5 mm, no further therapy was administered.
LLLT
For test group 1, a 0.1 W (100 MW) laser beam with a wavelength of 940 nm was used to laser-irradiate the inner and outer pocket mucosa in all ≥ 5mm pockets. It was a GaAlAs diode laser. The optical fiber was gently introduced into the pocket, moved for one minute in a circular motion from the deepest area of the pocket towards the cervical edge, and then for another minute it was moved smoothly along the outer gingiva.
PDT
For test group 2, periodontal pockets ≥ 5 mm was filled with indocyanine green (ICG) using a blunt needle. The inner and outer pocket mucosa was laser-irradiated using a laser beam of 0.1 W (100 MW) and 940 nm after the ICG has been activated for two minutes and the pocket has rinsed with saline solution. employed the same GaAIAs diode laser. After being carefully inserted into the pocket, the optical fiber was moved in a circular motion for one minute from the deepest area of the pocket toward the cervical margin.
Clinical Parameters such as Gingival index (Loe & Silness, 1963), Plaque index (Silness & Loe, 1964), Sulcular bleeding index (Muhlemann & son, 1971), Pocket probing depth (PPD), Clinical attachment loss (CAL) was recorded in all the 3 groups at baseline,1 and after 3 months.
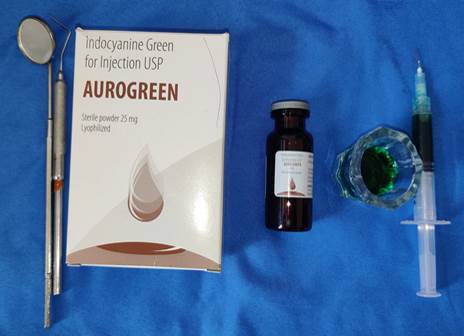

Fig 1: Indocyanine green Fig 2: indocyanine green delivery

Figure 3: Laser irradiation
RESULTS:
The present study systematically explored the adjunctive effects of Low-Level Laser Therapy (LLLT) and Photodynamic Therapy (PDT) when combined with Scaling and Root Planing (SRP), compared to SRP alone, in the management of chronic periodontitis. A total of 25 participants aged between 30 and 60 years, all presenting with probing depths of ≥5 mm and clinically diagnosed with chronic periodontitis, were included in the analysis.
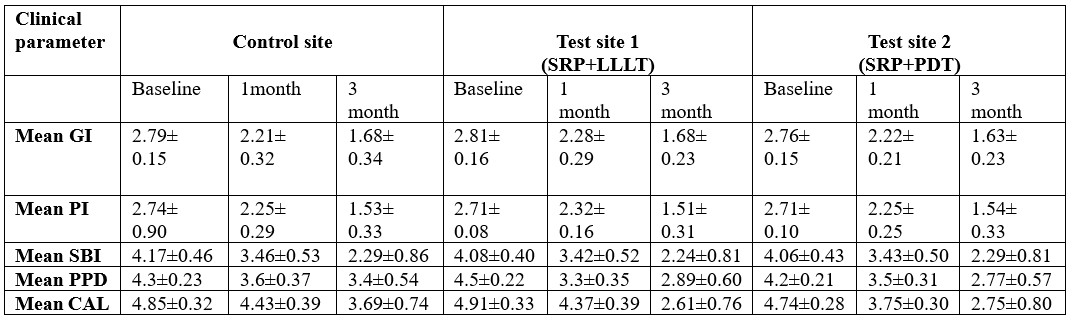
Clinical parameters—Plaque Index (PI), Gingival Index (GI), Sulcular Bleeding Index (SBI), Pocket Probing Depth (PPD), and Clinical Attachment Level (CAL)—were evaluated across all groups at baseline, 30 days, and 3 months. Each treatment group demonstrated a statistically significant intragroup improvement in all clinical indices from baseline to the 1- and 3-month follow-ups (p < 0.05), indicating a positive therapeutic response over time.
In terms of intergroup comparisons, PI, GI, and SBI showed statistically significant reduction by the 3-month follow-up, particularly in the LLLT and PDT groups compared to the control. Moreover, both adjunctive treatment groups test site 1 and test site 2 achieved significantly greater reductions in PPD and gains in CAL at 3 months when compared to SRP alone, with a highly significant p-value (p = 0.0001), reinforcing the enhanced clinical efficacy of LLLT and PDT as adjunctive modalities in periodontal therapy. (table 1)
Table 1: Comparison of clinical parameters in control and test sites
Discussion:
During the first stage of periodontal therapy, mechanical SRP uses manual or power-driven tools to non-surgically treat the diseased root surface debridement. However, using traditional mechanical therapy alone does not always result in the whole elimination of bacterial deposits and associated toxins from the root surface within the periodontal pockets.14 Recent reports have indicated that lasers can be used to treat periodontal pockets due to their ablation, bactericidal, detoxifying, and photo biomodification properties. Lasers have also been proposed as an alternative or adjunctive treatment to traditional periodontal mechanical therapy.8
PDT produces free radicals that may be harmful to bacteria, and recently it has been utilized to treat localized microbial infection. In the literature, biostimulation has been documented at therapeutic concentrations ranging from 0.001 to 10 J/cm2. 9 Additionally, by altering the expression of genes that produce inflammatory cytokines in vivo, LLLT reduces inflammation and speeds up wound healing.10
To treat chronic periodontitis, this study examines the long-term therapeutic effects of PDT and LLLT as a supplement to nonsurgical mechanical therapy. To our knowledge, there are no studies which investigated all the three treatment modalities (SRP, PDT, and LLLT) clinically on a long‑term basis, and thus prompted us to explore further to find their efficacy in the treatment of chronic periodontitis.
All groups showed significant reduction in GI and PI values from baseline to 3 months, reflecting reduced gingival inflammation. However, the test sites showed slightly greater improvement than control. This implies that LLLT and PDT display anti-inflammatory effects, with PDT exhibiting a somewhat improved outcome, presumably due to its direct antimicrobial activity through reactive oxygen species production.8 In line with this study, Qadri et al.11 reported a significant drop in PI values on the laser-treated side.
Sulcular Bleeding Index improved across all groups which is in accordance with the study done by Suryakanth Malgikar et al.4 Again, the combination of PDT and LLLT may have promoted improved cellular and vascular healing responses in gingival tissues, most likely through PDT bacterial inactivation and LLLT photobiomodulation.12
A key indicator of periodontal healing, PPD showed improved results in Test site 2 that is SRP along with PDT compared to that of test site 1 (SRP+LLT) and control site. These findings support the idea that deeper pocket resolution was made possible by additional therapy. Because PDT reduced the bacterial burden in periodontal pockets better, it was marginally more effective.13 The reason for the greater CAL increase in test locations as opposed to control sites could be that PDT and LLT stimulate tissue regeneration by promoting fibroblast proliferation, collagen formation, and angiogenesis.14
Therefore, this study aims to explore the effectiveness of benefits of Low-Level Laser Therapy (LLLT) and Photodynamic Therapy (PDT)as adjuncts to Scaling and Root Planing in Chronic Periodontitis.
Conclusion:
The present study was meticulously crafted to assess and juxtapose the impact of PDT and LLLT which has a potent anti-inflammatory, wound healing property when administered in conjunction with scaling and root planing, as opposed to scaling and root planing alone, in the management of patients with chronic periodontitis. This approach helps in the enhancement of periodontal health—an elegant and promising adjunctive treatment modality. This approach is an easy, non-invasive, secure and advantageous method. The present clinical trial suggests that all the three treatment strategies seem to benefit the patients with chronic periodontitis but combination of a single application of PDT (using Diode laser and indocyanine green) and LLLT provide additional benefit to SRP in terms of clinical parameters at 1 and 3 months.