International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 9 - Issue 1 - 2026
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
J Shanmugapriya1*, Swati Garg2, Seema Mehta3, Tanjul Saxena4, Ms. Geetika Goswami5
1Associate professor, Mahatma Gandhi college of Hospital Administration, Mahatma Gandhi University of Medical Sciences and Technology, Jaipur.
2Department of OB&G, Mahatma Gandhi University of Medical Sciences and Technology, Jaipur.
3Department of Public Health, IIHMR University, Jaipur.
4Mahatma Gandhi college of Hospital Administration, Mahatma Gandhi University of Medical Sciences and Technology, Jaipur.
5Assistant professor, Mahatma Gandhi college of Hospital Administration, Mahatma Gandhi University of Medical Sciences and Technology, Jaipur.
*Corresponding author: J Shanmugapriya, Associate professor, Mahatma Gandhi college of Hospital Administration, Mahatma Gandhi University of Medical Sciences and Technology, Jaipur.
Received: June 10, 2025
Accepted: June 30, 2025
Published: July 08, 2025
Citation: J Shanmugapriya, Garg S, Mehta S, Saxena T, Goswami G., (2025) “A Comprehensive Review of Under Five Malnutrition in India: Pattern, Progress and Challenges (2020-2023)”. International Journal of Epidemiology and Public Health Research, 6(6); DOI: 10.61148/2836-2810/IJEPHR/157.
Copyright: © 2025. J Shanmugapriya. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited., provided the original work is properly cited.
Introduction: India faces significant under-five malnutrition rates with disparities among tribal, non-tribal, rural, urban, and migrant populations despite government initiatives like POSHAN, Millet program, and AMMA. The burden remains high, especially in EAG states, prompting extensive primary and secondary research efforts. NFHS 5 provides insights into malnutrition, with NFHS 6 anticipated soon. Mapping literature from 2020-2023 can aid in understanding the prevailing prevalence in the Indian context.
Aim: The study's prime focus was to synthesize the prevalence, socio-economic conditions and maternal factors for under-five malnutrition identified in scholarly articles.
Methods: Following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA Framework), a comprehensive review was conducted. Multiple databases were systematically searched, and the retrieved records were organized and stored in a Mendeley library. Subsequently, the analysis focused on extracting and evaluating the relevance of the findings from the included studies.
Results: The review synthesized the prevalence of under-five malnutrition within the Indian context. It also examined comparisons made across different studies and highlighted various socio-economic factors and maternal influences identified by authors as contributors to malnutrition. This comprehensive analysis provides insights into the multifaceted nature of under-five malnutrition and the underlying determinants within India.
Conclusion: This review highlights a notable gap in the literature on millet-based research using appropriate methodology & importance of evidence-based interventions to address under-five malnutrition.
India has long faced the burden of child malnutrition and remaining persistent public health challenges. In response, Government of India launched the National Nutrition Mission- “POSHAN Abhiyaan” in March 2018 with the objective of accelerating improvements in nutritional outcomes levels in India. The mission has set annual targets for reducing levels of stunting, undernutrition, anemia, and low birth weight, to be achieved by 2022. The government has taken initiatives in the last decade to increase access to public health and nutrition services for children under five to address the immediate causes of undernutrition. These include relaxing population norms for the establishment of “Anganwadi” and “Mini-Anganwadi” centers, setting up health centers, and introducing state-specific schemes. [1] Despite these efforts, it remains uncertain whether the proposed targets have been achieved or not.
India has a high prevalence of childhood stunting globally, with an estimated 40.6 million children affected -approximately 35% of all children under the age of five. This is responsible for almost half of all child deaths globally, and stunting is linked to long-term harmful effects such as reduced mental ability and learning capacity, poor school performance, lower earnings, and higher risks of nutrition-related chronic diseases in the future. The POSHAN Abhiyaan was designed to reduce childhood stunting by 6% over three years through a life cycle approach, with UNICEF as a significant implementing partner. [2]This program aimed to make India malnutrition-free by 2022 by reducing stunting by at least two percent every year. There are also concerns that the program's focus on women's health largely revolves around pregnant and lactating mothers and ignores non-pregnant women. [3] India alone is home to 20 million of the world's 51 million wasted children. With 21% of children under five in India suffering from wasting, and an even higher prevalence in certain areas and tribal populations, such efforts are crucial. [4]. in addition to these issues, parents often face barriers to securing safe, nutritious, and affordable, age-appropriate food for their children in their early lives. These challenges are even greater during conflicts, disasters, and other humanitarian crises. [5]
India's latest National Family Health Survey (NFHS 5) reveals that children in several states are more undernourished than they were five years ago, stunting among children under five has increased from 44% to 55%, and the proportion of severely underweight children has risen from 7.8% to 13.4%. The survey was conducted in only 22 states before the COVID-19 pandemic, and experts fear the results will be worse in the remaining states surveyed after the lockdown ended. [6] The Global Nutrition Report reveals that inequalities exist within countries due to factors such as geographic location, age, gender, education, and wealth. Fragility and conflict worsen the issue, creating a significant urban-rural divide and larger differences across communities. Children under five are particularly affected. These inequalities stem from unjust systems that limit access to healthy, affordable food and quality nutrition care. The report uses the concept of nutrition equity to identify these inequities and proposes key actions to end malnutrition in all its forms. [7] "Stronger commitments for greater action" highlights the transformative role of accountability in addressing the nutrition crisis. It emphasizes the need for coordinated efforts among all stakeholders and analyzes the progress made so far. The report underscores the importance of accountability in delivering sustainable nutrition outcomes. [8]
NGOs have partnered with the government to address social issues to eliminate malnutrition, including Jan Swasthya Sahyog's crèches, PRIA and Gram Vikas' water and sanitation infrastructure, and the Fluoride Network of India's reduction of fluoride toxicity. UNICEF's #I. The COMMIT campaign emphasizes continued public advocacy and coordination between departments and states to address undernutrition. [9] It remains unclear whether these initiatives have been successful in achieving their intended goals and whether they have had a positive and sustained impact on the lives of the children and communities they are targeting. To determine the effectiveness of these initiatives, it is important to conduct rigorous evaluations that assess their impact on various aspects of malnutrition, such as stunting, wasting, and underweight, as well as other factors related to child health and development. Only then can we have a clear understanding of the effectiveness of these initiatives and make informed decisions on how to improve and scale up successful interventions.
Many Indian studies on under-five malnutrition have primarily focused on analyzing data from NFHS 1 to NFHS 5. However, after 2020-21, the COVID-19 pandemic shifted research priorities towards COVID-related studies. With NFHS 6 underway, efforts are being made to establish sampling procedures and guidelines for states. [10] In the absence of NFHS 6 data, research conducted between 2020-2023 has been crucial in understanding the prevalence and causal factors of under-five malnutrition across various Indian states and districts. These studies would be helpful to fill the gap until NFHS 6 data becomes available, providing insights into the complex dynamics of under-five malnutrition. By synthesizing findings from these research, policymakers and stakeholders can better comprehend regional variations and design targeted interventions to address under-five malnutrition effectively. The study's prime focus was to synthesize the existing scholarly literature on the prevalence and causal factors for under-five malnutrition in India. And the objective of this review is to quantify the reported rate of
Methods
Design: A review was performed following guideline, the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA Framework) [11].
Search methods:
Researchers used search engines like Google Scholar and EBSCO's SCOPUS as well as electronic databases including MEDLINE (PubMed), CINAHL-EBSCO, SCOPUS, and ProQuest's Health and Medical Complete. Initially, the database was searched using the Medical Subject Headings (MeSH) phrases (such as “Child Malnutrition), and then other terms surfaced as “Under five Malnutrition” “Infant Malnutrition”, “0-3 Malnutrition”. To extend the search, the authors used all MeSH/keyword combinations related to medication errors. The terms “Stunting”, “Wasting”, “Underweight”, “Diarrhea”, “Anemia” was used by the researchers.
In accordance with PCC – “Population, Concept and Context” framework [12], the following categories qualified for studies: Population (e.g., Under five children”), (2) primary and secondary research on the concept of “Stunting”, “Wasting”, “Diarrhea”, “Anemia” (3) contexts (e.g., “Indian states”, “Indian districts”) and published in English. Then, to broaden the scope of the search, we looked through the cited works of the included studies and added those that met our criteria.
Study selection process: The results of the literature search were saved in a reference manager (Mendeley). The reference manager software and human review were able to identify and eliminate duplicate studies. Once the duplicates were eliminated, there were two phases of selection for the studies. Two reviewers first checked all possibly relevant papers' titles, abstracts, and keywords for inclusion. Two reviewers read the whole articles chosen in the previous stage. After reviewing reference lists, studies were added.
Data extraction: The following components made up the final data extraction grid, that was accepted by the whole research team and used to collect data from the qualifying studies: Author details, Region, purpose, type of research, guidelines/tools followed, data utilized (Primary data as survey details /NFHS reports as secondary data) results based on prevalence of stunting, wasting and underweight, along with associated diseases. In addition, causal factors are classified under socio economic factors and mother’ antenatal and health factors. The studies selected are the works published between 2020-2023.
Prisma Framework: Selection of St:UDIES: FIG 1
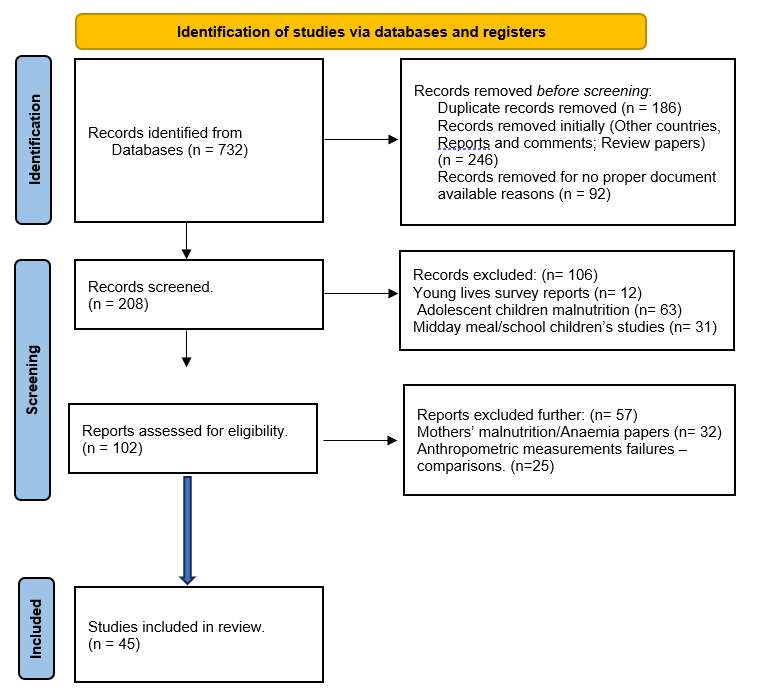
Figure 1: shows the study selection process, through the PRISMA framework.
RESULTS
Prevalence Of Stunting, Wasting and Underweight :
Out of 45 studies, 23 utilized cross-sectional primary data collection methods, as indicated in Table 1. These investigations focused on assessing the prevalence rates of stunting, wasting, and underweight among children under five years old. The remaining studies relied on secondary data sourced from NFHS surveys.
|
Region |
Stunting |
wasting |
Under Weight |
|
Western Maharashtra [13] |
33.5 |
12.4 |
35.5 |
|
West Bengal [14] |
45.7 |
9.8 |
24.9 |
|
Mandla district-Madhya Pradesh [15] |
46.74 |
24.72 |
51.81 |
|
Northeastern states of India [16] |
22 |
9 |
12 |
|
Rural Haryana [17] |
30.2 |
8.9 |
21.5 |
|
Jharkhand [18] |
25.3 |
12 |
31.8 |
|
South Delhi [19] |
27.3 |
17.8 |
29.1 |
|
Across India (ICDS)[20] |
36 |
19 |
32 |
|
Trivandrum [21] |
38 |
- |
19 |
|
Rural Haryana [22] |
41.3 |
18.4 |
38.3 |
|
Southern India [23] |
32 |
26.4 |
16.4 |
|
Western Ghats hills of India [24] |
40.9 |
27.4 |
48.3 |
|
Villupuram District, Tamil Nadu [25] |
38 |
54.2 |
61.8 |
|
Wayanad district of Kerala.[26] |
51.7 |
31 |
54.8 |
|
Across India [27] |
44.2 |
- |
39.5 |
|
Across India [28] |
35.9 |
23.8 |
32 |
|
Rural Rajasthan [29] |
58 |
45 |
54 |
|
Urban slum of Kolkata [30] |
59 |
44 |
12 |
|
Gwalior -Madhya Pradesh [31] |
59.45 |
22.18 |
53.09 |
|
Uttar Pradesh [32] |
45.2 |
13.4 |
- |
|
Across India [33] |
32.65 |
18.56 |
29.84 |
|
Rural belt- Rajasthan. (Tribal)[34] |
51.4 |
36.52 |
40.12 |
|
Rural belt- Rajasthan. (Non- tribal)[34] |
26.77 |
26.1 |
28.82 |
|
Rural Northern India [35] |
15.71 |
14.14 |
19.22 |
Table 1: Prevalence of stunting, wasting and underweight identified from studies.
Prevalence Of Moderate Acute Malnutrition (Mam) And Severe Acute Malnutrition (Sam) :
Three of the investigations underscored the acute malnutrition issues affecting children. A cross-national study comparing Tanzania and India underscored the malnutrition risk linked with diarrhea. The study evaluated the prevalence of moderate acute malnutrition (MAM) both before and after treating diarrhea with oral rehydration and zinc supplementation. Particularly among Indian children, the prevalence of acute malnutrition was recorded at 13.2% initially, decreasing to 2.5% post-treatment.[36]
In Dungarpur, Rajasthan, a separate study disclosed that 4.25% of children aged 6-59 months suffered from acute malnutrition. Among them, 4.07% were classified as moderate acute malnutrition (MAM) cases, while 0.18% were severe acute malnutrition (SAM) cases. This study was specifically conducted to pinpoint participants suitable for the Acute Malnutrition Management Action (AMMA) program. [37]
In the third study conducted in Vadodara, the differences between WHZ (Weight-for-Height Z-score) measures and MUAC (Mid-Upper Arm Circumference) measures in identifying cases of Acute Malnutrition were explained. While 67 cases of moderate acute malnutrition (MAM) were identified through WHZ measures, only 17 cases were revealed as MAM through MUAC measures. [38]
Prevalence Of Undenutrition and Associated Diseases:
Two studies have demonstrated a strong association between undernutrition and anemia in children, reporting prevalence rates of 66% [39] and 50% [24]respectively. An additional study [40]has underscored the significance of anemia as a major causal factor contributing to the burden of malnutrition among children. The widespread incidence of diarrheal diseases poses a significant risk factor for malnutrition, [41]particularly among children with a history of acute diarrheal infections. [23]
Four studies have examined the trend of overweight among children, revealing nuanced findings. One study reported a prevalence of 1.4% of children classified as overweight or obese,[24] indicative of a concerning trend of excess weight gain among certain populations. Moreover, another study observed a notable 1.9% increase in overweight prevalence over the course of a decade (2006-2016), suggesting a concerning trajectory.[42] Furthermore, dual studies have identified 4% [43]and 5% [19] of children as overweight when analyzing malnutrition indicators.
Both Kochupurackal Ulahannan et al. (2023) and Abedi et al. (2021) shed light on the relationship between symptoms like cough and fever and childhood undernutrition. Former reported a significant association between a history of cough and fever and a higher risk of undernutrition in children, with an adjusted odds ratio (AOR) of 2.93 and a 95% confidence interval (CI) of 1.24–6.93. [44] Similarly, later found a statistically significant association between fever and malnutrition among children, with a p-value less than 0.05.
Prevalence Of Malnutrition and Multiple Comparisons:
|
Comparisons |
|
Comparison between Indian districts |
|
Malnutrition prevalence is elevated in regions with low maternal care, particularly in the western, central, and eastern districts of the country. Factors influencing malnutrition indicators vary across districts, with state-level factors not always correlating with district-level occurrences. [45] |
|
Southern regions generally exhibit better growth conditions for children compared to the central tribal belt, where girls tend to have lower weight and height averages. Northeastern districts show more favorable conditions for healthy child development, correlating with lower poverty, higher female education, and improved maternal health indicators. [46] |
|
Comparison between states |
|
States such as Uttar Pradesh, Bihar, Jharkhand, Gujarat, and Maharashtra exhibited elevated rates of childhood undernutrition. Decomposition analysis highlighted that around 14.8% of the disparity in stunting, 10.4% in wasting, and 9.6% in underweight children born with low birth weight could be explained after adjusting for selected individual characteristics. [33] |
|
The reduction in childhood underweight varied across states, with West Bengal showing the highest improvement and Haryana the least. Stunting reduction ranged widely from Manipur to Himachal Pradesh, while changes in wasting were observed in Bihar & Jharkhand and Haryana. Disparities between children from the poorest and richest households showed mixed trends across states. [47] |
|
Comparison between EAG and Non EAG states |
|
The decomposition analysis showed that nearly two-thirds of the gap in undernutrition among children under five between Empowered Action Group (EAG) and Non-EAG states was clarified by the variables considered. Household wealth explained roughly half of the variance in stunting and wasting disparities, with religion accounting for a quarter of the differences in underweight and wasting. Maternal education explained a significant portion of the difference in stunting between EAG and Non-EAG states. [48] |
|
The prevalence of undernutrition remains high, exceeding 30% in most Empowered Action Group (EAG) states. While stunting and underweight have decreased across all EAG states, they still surpass national levels, with wasting rates rising only in Bihar. To address undernutrition effectively, concerted efforts including public health initiatives, collaborative partnerships, improved maternal education, heightened awareness, and enhanced socioeconomic empowerment of mothers are imperative. [49] |
|
Comparison of ICDS and Non ICDS |
|
Under-five children utilizing Integrated Child Development Services (ICDS) exhibit significant undernutrition, influenced by various socioeconomic and demographic factors. Logistic regression analysis revealed insignificant associations between ICDS usage and nutritional status, yet children not immunized at ICDS centers were less prone to stunting, wasting, and underweight. Determinants include child's age, gender, maternal education and nutrition, wealth index, social group, and regional factors among ICDS beneficiaries. [50] |
|
Boys’ and girls’ comparison |
|
A total of 400 under 5 were examined by going from house to house, and 257 (64.2%) of them were underweight. Boys had significantly (p=0.001) more undernutrition than girls. In the age range of 49 to 60 months, it peaked. [51] |
|
The proportion of WaSt cases decreased from 8.7% in 2005–06 to 5.2% in 2019–2020, peaking at 19 months before dropping after 24 months. Boys have a higher prevalence of concurrent wasting and stunting. Children in higher birth orders are more likely to experience WaSt, while those with more educated and wealthier mothers have lower chances of being affected. [52] |
|
Among the 207 SAM cases, 57% were girls, with a district prevalence of 0.18% compared to the state's 0.9%; SAM rates varied across blocks, ranging from 0.02% in Dowda and Chikhali to 0.63% in Jothari.(Dungarpur -Rajasthan) [37] |
|
Seven children (1.72%) were reported dead and 400 were alive, mostly girls (59.5) MTCs [53] |
|
Tribal and non-tribal comparison |
|
In the surveyed region, 38% of children exhibit stunted growth, with tribal children showing higher rates, and 19% of preschoolers are deemed underweight. Among tribal children, 27% are underweight, contrasting with 17% among non-tribal counterparts. Factors such as caste, ownership of assets, and maternal height correlate with stunting, while underweight status is linked with asset ownership. The logistic regression model highlights the significant role of caste in normal height for age, while higher asset ownership and older age (13-36 months) decrease the likelihood of underweight status. [21] |
|
In tribal communities, the prevalence of moderately and severely underweight children stood at 32.63% and 7.49%, respectively, compared to 24.41% and 4.41% in non-tribal communities. For stunting and Body Mass Index, 64.37% and 63.47% of tribal children were within normal ranges, while the figures for non-tribal children were 73.22% and 73.90%, respectively. Factors such as household income and maternal literacy showed significant associations with malnutrition. [34] |
|
Children in the coastal plain region are better nourished compared to the children from highland and mountainous region. In tribal dominated districts children are more vulnerable to all forms of undernutrition. [54] |
|
NFHS Comparisons |
|
Some districts still experience elevated levels of undernutrition, surpassing the state average. Ariyalur, Dindigul, Erode, Karur, Trichy, the Nilgiris, and Sivagangai (Tamilnadu Districts) consistently exhibited higher prevalence of child growth failure indicators in both NFHS rounds (4 and 5). While immediate determinants showed varied changes, underlying factors like household assets, sanitation, and electricity witnessed consistent improvement, albeit to varying degrees. [55] |
|
In the northeastern states, over 22% of children were stunted from 2019 to 2021, with at least 9% wasted and 12% underweight. Hotspot clusters for stunting persisted in Assam and Meghalaya across both NFHS-4 (2015–16) and NFHS-5 (2019–21). Similarly, persistent clusters for underweight were observed in both NFHS-4 and NFHS-5 in Assam and Tripura. [16] |
|
Between NFHS-1 and NFHS-5, wasting prevalence experienced a slight rise from 19.9% to 20.5%, while stunting decreased from 51.9% to 34.1%, and underweight decreased from 45.8% to 29.4%. Stunting and underweight declined by 6.36% and 5.86%, respectively, while wasting showed a minor increase of 0.21%. Factors such as mother’s education level and the child’s gender significantly influenced children’s nutritional status. [56] |
|
Migrant and non-migrant children |
|
Non-migrant children had higher rates of stunting (44.2%) and underweight (39.5%) compared to migrants (37.4% and 32.8% respectively). Among scheduled caste children, non-migrants showed significant variations in underweight (34% vs. 41.6%) and stunting (36% vs. 46%) compared to migrants. Similarly, malnutrition was prevalent among non-migrant children from poor households, rural areas, and with low-educated mothers. Poor non-migrant children had higher odds of being underweight and stunted compared to their migrant counterparts in the same household category, with similar trends observed among scheduled caste children. [27] |
Causal Factors for Malnutrition Identified from The Study:
Through the synthesis of diverse research, causal factors contributing to outcomes were categorized into socio-economic and maternal domains. Socio-economic factors encompassed variables such as poverty, income, households, assets, sanitation, electricity, transport etc. while maternal factors included health, education, pregnancy and breast feeding.
Poverty/Bpl:
Numerous studies underscore the detrimental impact of poverty on nutrition status among children. Striessnig & Bora (2020) revealed a correlation between poverty and below-average child height and weight, highlighting the stark reality that children from poor families are disproportionately affected. Nambiar et al. (2023) further solidified this connection, establishing a significant association between poverty and under-five malnutrition. In contrast, the potential positive influence of working women in poor households, who contribute economic capital that indirectly benefits family health and nutrition. [20]. Shankar Mishra et al. (2022) identified a concerning trend of malnourishment within the poor wealth quintile, emphasizing that non-migrant children from impoverished backgrounds are particularly susceptible to being underweight compared to their migrant counterparts.
Karlsson et al. (2021) highlighted state-wise disparities in malnutrition rates, noting significant variations between the poorest and richest household living standards. Khadse & Bansod (2021) echoed this, revealing disparities in wealth and their association with malnutrition, particularly among children of Scheduled Castes. Logistic regression analysis by Gangurde & Waghela (2023) pinpointed BPL cardholder status as significantly linked to undernutrition, while Khura et al. (2023) found that children from wealthy families were substantially less likely to experience WaSt cases, indicative of the protective role of wealth against malnutrition. Moreover, Ansary & Rath (2021) identified the wealth index as a significant predictor of childhood undernutrition, emphasizing the multifaceted nature of poverty's impact on health outcomes. Agarwal et al. (2021) provided further insight, demonstrating through stepwise regression analysis the heightened risk of underweight and stunting among children from the lowest and middle households’ wealth index categories, underscoring the urgent need for targeted interventions to address the complex interplay between poverty and malnutrition.
Income And Household Assets:
The correlation between household income and undernutrition is a recurring theme across various studies. Gangurde & Waghela (2023) and Chowdhury et al. (2023) independently conducted logistic regression analyses, both uncovering a significant association between per capita income and undernutrition. Similarly, Mangal et al. (2020) identified a strong link between household income and malnutrition, while Scopazzini et al. (2021) utilized a linear mixed model analysis to reveal household income as a negative predictor of stunting. S. Singh et al. (2023) found that larger household sizes were associated with a heightened risk of Double Burden Malnutrition, as indicated by logistic regression. Shirisha (2022) noted varying changes in immediate determinants of malnutrition across districts, including household assets. Moreover, S. K. Singh et al. (2023) emphasized the significant role of household variables in determining the malnutrition burden in India. Ansary & Rath (2021) highlighted the influence of religion, social groups, and region of residence as significant predictors of childhood undernutrition, indicating the complex interplay of socioeconomic factors in shaping nutritional outcomes.
Civil Amenities :
Hygiene and sanitation emerge as pivotal factors influencing childhood undernutrition across several studies. Ansary & Rath (2021) identified hygiene-sanitation practices as significant predictors of childhood undernutrition, while Nambiar et al. (2023) established a statistically significant association between household sanitation facilities and nutritional outcomes. Kochupurackal Ulahannan et al. (2023) revealed that Adivasi children suffer from undernutrition due to disparities in access to clean water and sanitation, exacerbating their vulnerability. Mandadi et al. (2023) employed a spatial error regression model, highlighting the critical role of maternal health and improved sanitation facilities in combating malnutrition in India. M. Singh et al. (2021) observed a robust direct relation between poor sanitation facilities and adverse health outcomes like diarrhea, exclusive breastfeeding, and childhood malnutrition. Additionally, Shirisha (2022) noted varying improvements in factors like access to electricity, which also play a role in shaping nutritional outcomes, albeit to different extents.
Numerous studies have pinpointed significant determinants of undernutrition among children, shedding light on multifaceted factors influencing nutritional status. Abedi et al. (2021) highlighted a statistically significant association between food security and malnutrition among children, while Kochupurackal Ulahannan et al. (2023) revealed the complex interplay of factors, including unequal access to social capital, healthcare, and food security, contributing to undernutrition among Adivasi children. Additionally, another study identified a plethora of determinants among ICDS beneficiaries, ranging from demographic factors like child's age and gender to socio-economic indicators like maternal education, wealth index, and region of residence.[50]
Mothers’factors :
There is broad consensus regarding the necessity of direct maternal nutrition interventions to enhance women's nutrition, improve birth outcomes, and foster children's linear growth during infancy and early childhood. Maternal nutrition serves as a critical determinant of under-five malnutrition, exerting a profound influence on children's nutritional status and overall well-being. Ensuring adequate maternal nutrition is essential for mitigating the risk of malnutrition among young children. [23] Therefore, this review paper aims to synthesize the maternal factors identified by multiple studies conducted between 2020 and 2023.
Mother’s Education:
The association between maternal education and child malnutrition emerges as a consistent theme across multiple studies conducted between 2020 and 2023. Abedi et al. (2021) and Khadse & Bansod (2021) both found significant associations between malnutrition and mother’s education, with the latter noting a positive correlation among children of Scheduled Castes. Ansary & Rath (2021) highlighted the high intra-district disparity in undernutrition in western Odisha, emphasizing the role of mother’s educational status in under-five malnutrition. Chaudhuri et al. (2023) identified mother’s education and child’s sex as significant factors influencing nutritional status, while Khura et al. (2023) reported a 47% lower chance of WaSt cases among children of more educated mothers. M. Singh et al. (2021) indirectly associated maternal education with outcome variables, further reinforcing its importance. Chowdhury et al. (2023) revealed that maternal education explained a significant portion of the difference in stunting between different states. Finally, Striessnig & Bora (2020) highlighted the geographical clustering of malnutrition with low maternal education, suggesting a strong correlation between these factors.
Mothers Health:
Several studies have delved into the intricate relationship between maternal health and child malnutrition, uncovering significant insights. Mandadi et al. (2023) underscored the importance of maternal health indicators such as low BMI and early marriages, which were associated with a heightened risk of child malnutrition. Similarly, Striessnig & Bora (2020) identified geographical clusters of malnutrition aligning with lower maternal BMI and higher prevalence of parity 4+ and teenage pregnancies. Additionally, S. Singh et al. (2023) highlighted households with women exhibiting abdominal obesity as hotspots for elevated double burden malnutrition, with factors like C-section births and advanced maternal age amplifying the risk. Moreover, M. Singh et al. (2021) observed widespread low birth weight, indicating potential gaps in maternal healthcare access. Notably, Nambiar et al. (2023) established a significant association between malnutrition and institutional births, emphasizing the critical role of healthcare settings in addressing nutritional needs. Mothers who attended four or more ANC visits and consumed iron-folic acid (IFA) supplements for at least 100 days experienced a reduced prevalence of wasting, stunting, and underweight compared to mothers who had three or fewer ANC visits and insufficient IFA intake. [22] Furthermore, the study conducted decomposition analysis, revealing that a substantial portion of differences in stunting, wasting, and underweight among children were attributable to low birth weight.[33]
Breast Feeding and Dietary Needs of the Children:
Several studies have explored the associations between various factors and childhood undernutrition. Shweta Gangurde & Hetal Waghela (2023) conducted logistic regression, revealing that prelacteal feed and colostrum were significantly associated with undernutrition. M. Singh et al. (2021) observed a Moran’s I value indicating global spatial autocorrelation for exclusive breastfeeding and low birth weight. The study noted that children aged six to 24 months exhibited continued breastfeeding practices at a high rate (88.0%), with most breastfeeding five to six times a day (45.8%). However, it was observed that a majority of the children were not being fed according to maternal infant and young child feeding protocols. The study identified several predictors for a well-fed child, including age in months, age category, and breastfeeding frequency, which were associated with adjusted odds ratios indicating their impact on child nutrition status.[53] S. Singh et al. (2023) identified a heightened risk of double burden malnutrition (DBM) within households characterized by C-section births, affluence, and ongoing breastfeeding practices. Verma et al. (2021) found that malnutrition was higher among children who were not exclusively breastfed. Nirmalson & Vijayakarthikeyan (2022) highlighted the significance of exclusive breastfeeding in underweight, stunting, and wasting. Saha et al. (2023) concluded that inadequate minimum dietary diversity significantly increased the risk of being stunted, wasted, and underweight. Kochupurackal Ulahannan et al. (2023) emphasized the absence of a kitchen garden with fruits and vegetables and a history of cough and fever as contributors to heightened undernutrition risk. Saha et al. (2023) underscored the importance of dietary diversity, noting that children lacking intake of essential food items like dairy products and fruits and vegetables were more prone to stunting, wasting, and underweight status.[28].
Discussion:
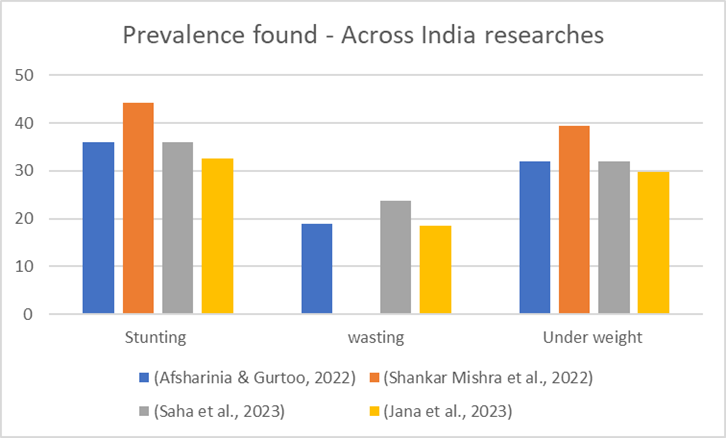
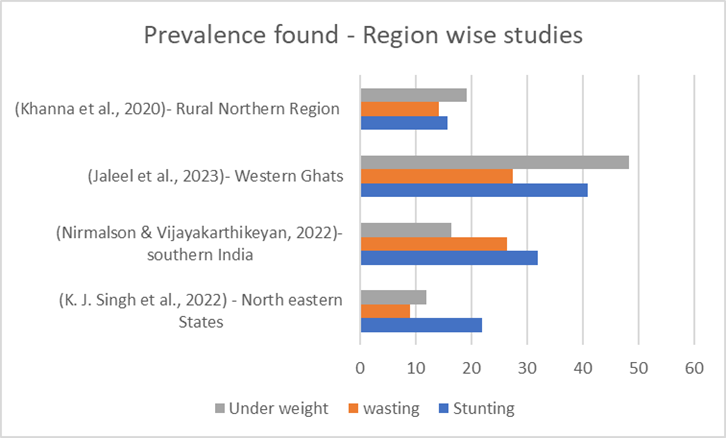
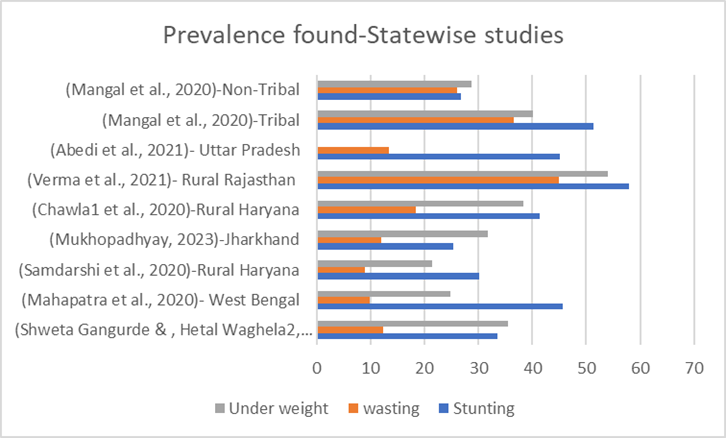
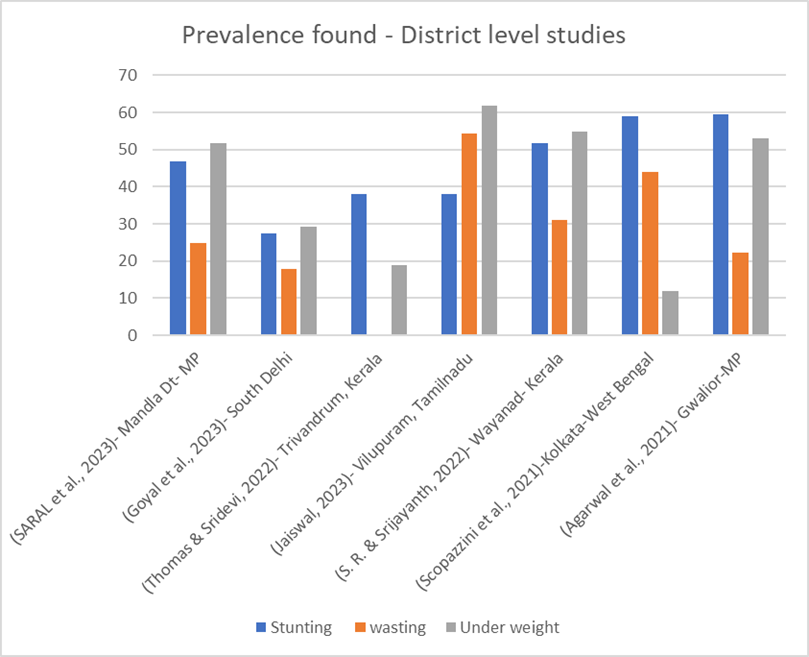
In the Indian context, the distribution of studies conducted using cross-sectional primary data collection methods is as follows: four studies (Fig 2) were conducted across India, four studies (Fig 3)) were region-wise, eight studies (Fig 3) were state-wise, and seven studies (n=7) were district-wise. Additionally, approximately 22 studies relied on secondary data from NFHS surveys. This classification highlights the varied approaches taken in research, ranging from national to local levels, with a significant reliance on NFHS secondary data for analysis and insights.
Pooled estimate of prevalence of child malnutrition – identified from the studies:
For the pooled estimate calculation, every study's (n= 23) sample size was considered, and the number of affected children was determined based on the respective studies' calculated percentages. Additionally, the mean count of affected children identified in Indian studies was computed.
Total number of samples taken = 630479
Total number of children stunted = 234456
Total number of children wasted = 74306 (But 3 of the studies not calculated wasting data)
Total number of children underweight = 203851 (one of the studies not calculated underweight)
Percentage of stunted children= 37.18% (calculated for 23 studies)
Percentage of wasted children= 11.7% (calculated for 20 studies)
Percentage of underweight children= 32.33 (calculated for 22 studies)
Out of the 45 studies examined, only two were intervention-based. One study implemented a nutritional counseling program as its intervention, [35]while the other conducted a pilot nutritional support program utilizing case-control studies. [30] While there is widespread discussion on the significance of millets in addressing malnutrition, intervention programs focusing on millet food supplements have not been widely published. Many articles, comments, and government policies highlight this importance, yet research articles specifically addressing millet interventions remain scarce. Only one study identified the association between millet cultivation and wasting patterns, particularly noting a stronger association with jowar and other millets. [57] Another study explored a millet-based mid-day meal intervention program, but it focused on adolescent school-going children and was not included in our review. [58] Additionally, a study in Coimbatore, Tamil Nadu, targeted children aged 3-6 years with a one-year intervention involving six nutrient-rich formulations of millet-pulse-groundnut-based products tailored to local taste preferences. [57] However, it fell outside our review period. Another nutritional intervention utilizing climate-resilient millets, pulses, and groundnuts to promote dietary diversity and improve children's nutrition and health status exists, [59] but it has not undergone peer review.
The studies conducted across India lack clarity regarding the specific regions or states included in the sampling process for generalizing the results. Moreover, district-based studies predominantly focused on populations of tribal and scheduled communities, with a greater emphasis on rural areas rather than urban locales. It is notable that urban slums and migrant children in urban areas of many metropolitan cities also encounter similar issues related to malnutrition.
Although childhood malnutrition remains a critical issue in India, there is a lack of diversity in robust research methods utilized, with frequent repetition across multiple studies. Common approaches include descriptive statistics such as mean values, frequencies, and percentages, along with inferential methods like logistic regression, ANOVA, F-tests, paired t-tests, and Chi-square tests. Notably, only one study attempted model building using Principal Component Analysis (PCA), [46]. while spatial analysis was conducted by five authors across different studies. [40] [16] [41] [43] [41]Limited research utilized the two-way blinder Oaxaca decomposition method. [48][34] Most studies relied on MS Excel and SPSS for analysis, with a few using WHO Anthro software. [19][13][22][24]Additionally, only one study employed NPV and PPV through the Youden Index,[38] and trend analysis was performed by two authors.[55] [47]
Conclusion
In conclusion, this review underscores the pressing need for increased research focus on intervention programs linking millet consumption with combating malnutrition among children under five. The findings highlight a significant gap in literature, with limited published studies addressing this critical issue. Authors emphasize the importance of adopting robust methodologies to ensure the reliability and validity of future research endeavors in this domain. Encouraging interdisciplinary collaboration and innovative approaches can further enrich our understanding of the potential benefits of millet-based interventions in addressing childhood malnutrition. It is imperative that policymakers, researchers, and stakeholders prioritize efforts to explore and implement effective strategies that integrate millets into nutrition programs. By bridging this gap in research and promoting evidence-based interventions, we can advance the fight against childhood malnutrition and contribute to improved health outcomes for vulnerable populations.