International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 9 - Issue 1 - 2026
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
Nelson Adekoya, DrPH1* and Man-Huei Chang, MPH1
1National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention, Atlanta, Georgia, USA.
*Corresponding author: Nelson Adekoya, DrPH National Center for HIV, Viral Hepatitis, STD, and TB Prevention, Centers for Disease Control and Prevention 1600 Clifton Road, NE MS-E07 Atlanta, GA 30341, USA.
Received: May 26, 2025
Accepted: June 10, 2025
Published: June 17, 2025
Citation: Adekoya N, Man-Huei C. (2025) “Educational attainment and all-cause and HIV mortality among adults — United States, 2018–2021”. International Journal of Epidemiology and Public Health Research, 6(5); DOI: 10.61148/2836-2810/IJEPHR/150.
Copyright: © 2025. Nelson Adekoya. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited., provided the original work is properly cited.
Objective: We described age-adjusted death rates of all-cause and HIV and educational attainment among US adult residents at national and state levels during 2018–2021.
Method: We used 2018–2021 mortality data from the Centers for Disease Control and Prevention underlying cause-of-death files and the American Community Survey (2017–2021) to assess the influence of educational attainment on all-cause deaths and HIV deaths. We conducted unadjusted regression and Pearson’s correlation to test for the association between age-adjusted death rates for all-cause and HIV mortality and educational attainment.
Results: Among 35 states that recorded educational attainment above the national average of 88.9%, age-adjusted mortality rates were lower for 22 states, compared with the nationwide all-cause mortality rate. Similar patterns of increased HIV age-adjusted mortality rates were observed with decreased educational attainment. A significant correlation was identified between increased mortality rates for all-cause deaths (r = –0.45; P <.0021) and HIV deaths (r = –0.66; P <.0001) and decreased educational attainment. Black population had the highest all-cause and HIV mortality rate than among White and Hispanic/Latino population. However, the lowest educational attainment rates were observed among Hispanic/Latino populations (71.2%) than Black population (87.2%) and White (93.5%) population during 2017–2021.
Conclusion: This ecological study shows the importance of reducing disparities in education to improve health.
Introduction:
Several risk factors (e.g., smoking, diet, lack of exercise, use of seatbelts) leading to premature death have been addressed in the United States, resulting in notable declines in mortality rates and increased life expectancy (i.e., the expected number of years that a group of persons might live at each attained age if the group is subject to the age-specific death rates prevailing for the actual population in a given year) (1,2). One socioeconomic factor affecting health outcome determination is education, whereby an increase in educational achievement decreases income inequality and improves health outcomes (3). At least one study has shown that cumulative mortality decreases drastically as educational achievement increases, and individuals who lack primary or secondary education have higher risk for death than those with tertiary education (4). Similarly, the relationship between educational levels and all-cause mortality among persons with HIV has been documented (5,6). Because education is a well-established social determinant of health, and there is a documented negative linear relationship between educational level and HIV infection rate (7), it is essential to continually assess educational levels and HIV mortality to identify, develop, and implement additional prevention strategies (8).
Education enhances citizens’ ability to process behavioral development which is necessary to build healthy community. Education is associated with employment, income, health insurance, and health care utilization which are associated with better health outcomes and lower death rates (9). Recognizing the role of education in community health, Healthy People 2020 (10) and Healthy People 2030 (11) specifically placed education among its leading health indicators. Additionally, the National HIV/AIDS Strategy for United States developed by the White House Office of National AIDS Policy, in collaboration with federal and community partners, unambiguously stressed that education is an important socioeconomic factor that should be considered in approaches to address individual, community, and structural factors and inequalities that contribute to HIV transmission (12).
Education is sensitive to structural factors such as economy which is important in healthcare delivery system (13). Nationwide, educational attainment has improved; however, mortality rate inequalities exist between states (8,12). While education can be used as an instrument to understand HIV mortality differentials in communities (population health), state-level information is sparse (14). The National HIV Surveillance Report presents HIV deaths by age, race, sex, transmission category, and region of residence but does not include educational attainment and deaths by state (15). Because HIV infections are higher among younger persons and inequalities in mortality are more pronounced among this population (16), we present an ecological study which combines state-specific all-cause mortality and HIV mortality data from the National Centers for Health Statistics Vital Statistics with state-specific data on educational attainment from the American Community Survey (ACS). Given that education has a protective effect on most causes of death (5,6), we present the overall correlation between educational attainment and all-cause mortality and HIV mortality to determine whether both follow similar patterns.
Methods
National Vital Statistics System data were obtained from WONDER, which provides customized reports based on state-reported death certificate records (17). The underlying cause of death data on all-cause mortality and HIV deaths during 2018– 2021 were analyzed. Mortality and educational attainment analyses were limited to persons aged ≥25 years (18), in parallel with the ACS on educational attainment. Population estimates from the U.S. Census Bureau were used to calculate death rates, and rates were age-adjusted to the 2000 standard U.S. population. Results are presented for all-cause deaths and HIV mortality at the national and state levels. Because access to care can affect health problems regardless of educational attainment, especially in rural states (19), all-cause mortality death was used as a mean test (standard) because composite risk factors are inclusive (e.g., smoking, high blood pressure, lack of exercise, high cholesterol level, family history, and sedentary life), including heart diseases which is a major cause of death (17). If the effect of education is substantial, the pattern noted for all-cause deaths would resemble HIV deaths. A previous study reported that cause-specific death rates indicate that changes in death rates for heart disease account for a substantial portion of the increase in educational differentials in overall mortality (20). Death counts <10 was suppressed and deaths <20 are considered unreliable following the data source stipulations (17).
Educational attainment statistics were obtained from ACS, an ongoing statistical survey conducted by the U.S. Census Bureau. Data are collected monthly on a random sample of the U.S. population regarding education, income, language proficiency, migration, and housing, among other characteristics. These monthly data are aggregated to generate annual estimates, which reflect the dynamics of U.S. population. The 2017–2021 ACS 5-year estimates were used to calculate national- and state-level percentages of persons aged ≥25 years with a high school or higher educational attainment; mortality rates for both all-cause and HIV mortality were compared with educational attainment. Educational attainment data by state were available for Non-Hispanic or Latino (Hispanic) White (NHW, herein referred to as White throughout the manuscript) and Hispanic or Latino persons but not for Non-Hispanic or Latino Black /African-American (Black) persons (although there is a table for Black /African-American persons).[1] We analyzed and presented data on sex. Lastly, we conducted unadjusted regression and Pearson’s correlation to test for the association between age-adjusted death rates for all-cause and HIV mortality and educational attainment using SAS (version 9.4; SAS Institute). This analytic study did not involve human subjects research supervised by a CDC Institutional Review Board.
Results
All-Cause Deaths
During 2018–2021, a total of 12,288,169 deaths occurred in the United States among persons aged ≥25 years, for an age-adjusted mortality rate of 1,186.2 deaths/100,000 population (Table 1). Nationwide, Hawaii, California, and New York recorded the lowest overall mortality rates at 887.4, 1,008.4 and 1,041.1 deaths/100,000 population, respectively. Whereas Mississippi, West Virginia, and Alabama recorded the highest mortality rates at 1,577.9, 1,574.6, and 1,503.5 deaths/100,000 population, respectively. Although 18 states recorded mortality rates of <1,186.2 deaths/100,000 population, 13 states recorded rates >1,300 deaths/100,000 population, the majority of which were in the South (Georgia, Alabama, Arkansas, Indiana, Kentucky, Louisiana, Mississippi, Missouri, Ohio, Oklahoma, South Carolina, Tennessee, and West Virginia). Four states recorded >1,500 deaths/100,000 population (Alabama, 1,503.5; Kentucky, 1,507.8; Mississippi, 1,577.9; and West Virginia, 1,574.6) and none of the southern states were represented in the first quartile of deaths (887.4–1,116.2 deaths/100,000 population).
The rate for men (1,407.9 deaths/100,000 population) was 41% higher than that for women (997.3/100,000 population), for an absolute rate difference of 411 (Table 2). Women in West Virginia (1,331.6), Mississippi (1,314.4), and Kentucky (1,276.2) had the highest mortality rates, compared with women in Hawaii (701.4), California (832.2), and Connecticut (879.0), who had the lowest mortality rates. Similarly, men in Mississippi (1,900.9), West Virginia (1,843.3), and Alabama (1,797.1) had the highest mortality rates, compared with the rates for men in Hawaii (1,098.5), California (1,213.2), and Minnesota (1,235.5).
HIV Deaths
Minnesota, New Hampshire, and Utah recorded the lowest overall HIV mortality rates, each with 0.6 deaths/100,000 population. Alternatively, District of Columbia, Mississippi, Florida, and Louisiana recorded the highest mortality rates at 13.9, 4.7, 4.2, and 4.2 deaths/100,000 population, respectively. Although 13 states recorded mortality rates of ≤ 1 death/100,000 population, 12 states recorded rates of ≥
1 death/100,000 population, 12 states recorded rates of ≥ 2.7 deaths/100,000 population; there was no noteworthy concentration of states by region, unlike all-cause deaths recorded in the South (Georgia, Alabama, Delaware, District of Columbia, Florida, Maryland, Nevada, New York, Louisiana, Mississippi, South Carolina, and Texas). The District of Columbia (13.9) recorded the highest rate compared with other states; 4 states that recorded ≥
2.7 deaths/100,000 population; there was no noteworthy concentration of states by region, unlike all-cause deaths recorded in the South (Georgia, Alabama, Delaware, District of Columbia, Florida, Maryland, Nevada, New York, Louisiana, Mississippi, South Carolina, and Texas). The District of Columbia (13.9) recorded the highest rate compared with other states; 4 states that recorded ≥ 4.1deaths/100,000 population were in the South (Georgia, Florida, Louisiana, and Mississippi). None of the southern states were represented in the first quartile of deaths (0.9–1.0 death/100,000). Wyoming did not meet the reporting threshold (death counts <10), and rates were unreliable (death count < 20) for 6 states (Alaska, Idaho, Montana, North Dakota, Vermont, and Wyoming).
4.1deaths/100,000 population were in the South (Georgia, Florida, Louisiana, and Mississippi). None of the southern states were represented in the first quartile of deaths (0.9–1.0 death/100,000). Wyoming did not meet the reporting threshold (death counts <10), and rates were unreliable (death count < 20) for 6 states (Alaska, Idaho, Montana, North Dakota, Vermont, and Wyoming).
The HIV mortality rate for men (3.3 deaths/100,000 population) was 3 times higher than that for women (1.1/100,000 population), with an absolute rate difference of 2.2 (Table 2). Women in the District of Columbia (10.7), Mississippi (2.9), Florida (2.7), Louisiana (2.6), Georgia (2.4), and Maryland (2.2) had the highest mortality rates, compared with women in Washington (0.3), Wisconsin (0.4), and Colorado (0.3), who had the lowest mortality rates. Similarly, men in the District of Columbia (17.7), Mississippi (6.7), Louisiana (5.8), and Maryland (5.6) had the highest mortality rates, compared with the rates for men in Wisconsin (1.0), Minnesota (1.1), and Utah (1.1). More small data points were suppressed or unreliable for females than males.
Educational Attainment, All-Cause Deaths, and HIV Deaths
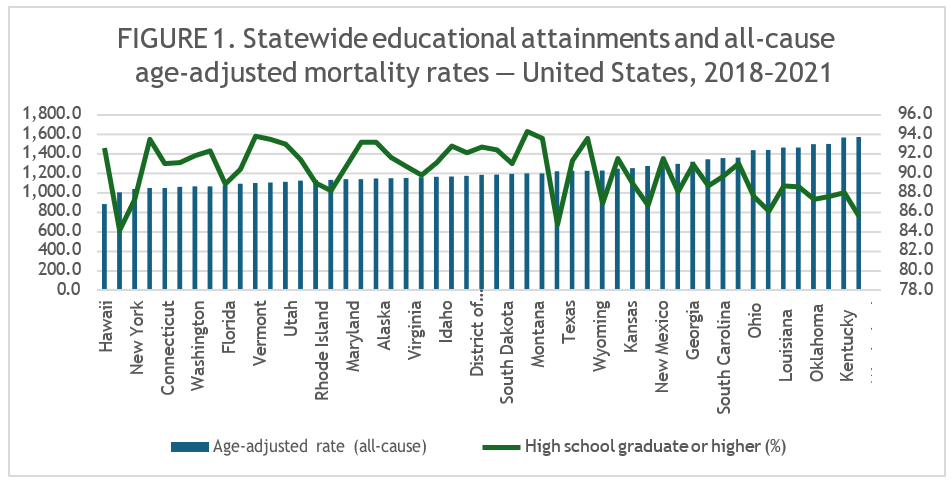
Figure 1 presents the all-cause mortality rates, by state, from the lowest to the highest all-cause mortality rates. Beginning with the state ranked 31st (Texas, 1,225.7 deaths/100,000 population), there was a noteworthy gradient increase in mortality rates. The increase in mortality corresponded to a continuous decline in educational achievement, reaching 85.6% for Mississippi. Educational attainment
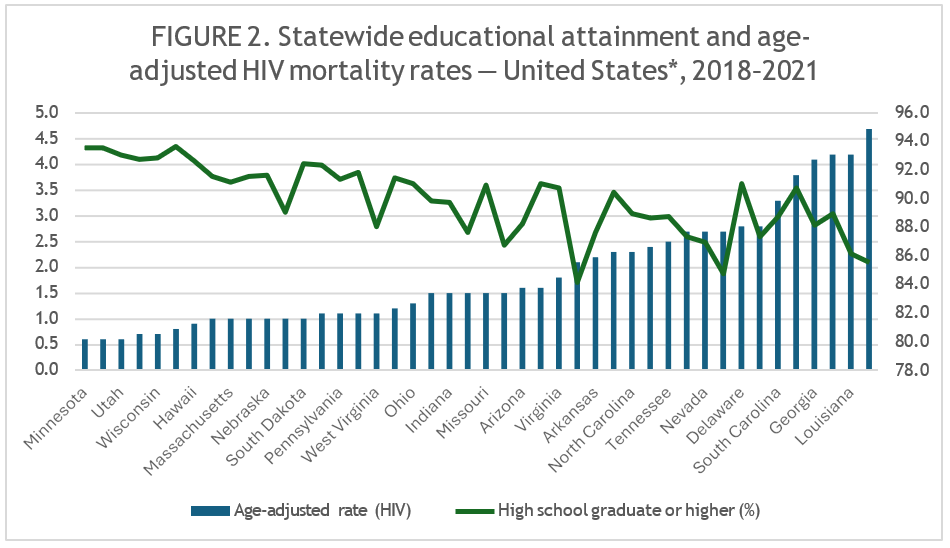
(high school completion or higher) ranged from 94.4% in Montana to 84.2% in California. California (84.2%), Texas (84.8%), and Mississippi (85.6%) had the lowest educational attainment. The relationship between HIV deaths and educational attainment was similar to that observed in all-cause deaths, where lower educational attainment corresponded with increased HIV death rates (Figure 2). Minnesota, New Hampshire, Utah, and Iowa, each with higher educational attainment, had lower HIV death rates. In contrast, Mississippi, Louisiana, Texas, and California, all with lower educational attainment, had higher HIV death rates. In 6 states, the educational attainment gradient was so high that adjusted death rates were too unreliable to report, suggesting an inverse relationship between educational attainment (Alaska, 93.3%; Idaho, 91.2%; Montana, 94.4%; North Dakota, 93.3%; Vermont, 93.9%; and Wyoming, 93.7%) and HIV deaths. A significant correlation was identified between increased mortality rates for all-cause deaths (r = –0.45; P <.0021) and HIV deaths (r = –0.66; P <.0001) and decreased educational attainment.
Race/ethnicity, Sex, Educational Attainment, All-Cause Deaths, and HIV Deaths
The state-specific all-cause and HIV deaths compared with educational attainment by sex and race/ethnicity (data not shown). Data on HIV age-adjusted death rates for race/ethnicity and sex were sparse and therefore were either suppressed or unreliable in certain states, making correlation test results unreliable. White population had the highest average educational attainment at 93.5% and only handful states recorded <90% educational attainment (Alabama, Kentucky, Louisiana, Mississippi, and West Virginia) among this population. The highest HIV age-adjusted death rates were recorded in Florida (2.1), Nevada (2.2), and Oklahoma (2.0) among non-Hispanic White persons. Fifteen states recorded HIV age-adjusted death rates greater than the national average for White population. Age-adjusted death rate was 4.5 times higher in males (1.8) in comparison to females (0.4). Age-adjusted all-cause death rate recorded for White population (1,213.8) is lower than for the Black population (1,448.5) but higher than the Hispanic/Latino population (941.2).
For Black population, the average age-adjusted HIV death rate was 8.8 deaths/100,000 with marked differences between males and females’ Black population (12.7 versus 5.4). Thirteen states recorded age-adjusted death rates greater than the average for Black population (Delaware, 9.5; District of Columbia, 26.2; Florida, 15.9; Georgia, 10.2; Louisiana, 10.4; Maryland, 10.3; Mississippi, 10.3; Nevada, 9.0, New Jersey, 10.3; New York, 9.2; South Carolina, 9.7; Tennessee, 9.6; and Texas, 8.9). The average educational attainment of Black population is 87.2%. HIV age-adjusted death rate among Black males (12.7) was 2.35 times the rates among females’ Black population (5.4). All-cause mortality age-adjusted rate of males (1,789.1) was much higher than the females in Black population (1,191.8).
For Hispanic/Latino population, the average educational attainment was 71.2% which was substantially lower than the rate in Black population (87.2%) and White population (93.5%). Hispanic/Latino males recorded the lowest educational attainment at 69.7%. The average age-adjusted HIV death rate for Hispanic/Latino population group is 2.1 and rates were higher than the Hispanic/Latino population average among 7 states (Connecticut, 3.6; Florida, 2.4; Massachusetts, 2.8; New Jersey, 2.6; New York, 4.4; Oklahoma, 2.4; and Pennsylvania, 2.6). Hispanic/Latino population recorded the lowest all-cause mortality rate (941.2) in comparison to Black and White population groups. Similarly, age adjusted rates were lower for Hispanic/Latino males (1,151.1) and females (762.3) in comparison to White and Black population of these groups.
Discussion
This study examined the association of education on all-cause and HIV mortality among adults in the United States during 2018–2021. Among 35 states (69%) that recorded educational attainment (i.e., high school graduate or equivalent) above the national average of 88.9%, age-adjusted all-cause mortality rates were lower for 22 states (22/35; 63%), compared with the nationwide all-cause mortality rate. With the exception of California, New York, and Arizona, among the 16 states with the lowest educational attainment, age-adjusted mortality rates increased and were worse than the national average (13/16; 81%). Additionally, similar inverse patterns of increased adjusted mortality rates were identified when educational attainment and HIV deaths were examined. Because persons who are educated live longer and suffer less morbidity during their lifetime (21), education is an effective tool for addressing health disparities and is associated with other socioeconomic factors such as employment, income, health insurance, and health care utilization (9).
Examination of death rates and educational attainment provides information on the population groups that might be focused or targeted for interventions. This analysis supports a previous study that reported associations between education and mortality (22). The majority of states with lower educational attainment exhibited high mortality rates both for all causes of death and HIV. Although higher mortality rates among persons with lower education reflect a complex causal pathway with confounding variables (22), given the importance of social determinants of health, Healthy People objectives specifically encourage programs and jurisdictions to collaborate in addressing education and other social determinants of health. Educational attainment is a socioeconomic variable that remains relatively constant throughout adulthood because the majority of persons achieve the required level before adulthood (23). As such, there is a long-term consequence on health.
Although educational attainment improved during the study period, states with the lowest education attainment are still at increased risk for death from all causes and HIV. One major finding of this report is that the risk for all causes of death was substantially greater among states with the least educated residents, compared with the states where residents are more educated. Lower educational attainment is associated with health risk factors (e.g., smoking, inadequate nutrition, lack of exercise, lack of access to high-quality medical care, and the inability to afford adequate housing and food) (19,24). States in the South and Midwest regions continue to record higher rates of smoking, despite tobacco being the leading cause of preventable diseases and death (25,26). Although the nation is experiencing improved educational attainment, medical care, and access to care, longitudinal studies are needed to determine whether people of all education levels are experiencing these improvements. To address health disparities, nonprofit organizations located in states with high mortality rates can take advantage of the Patient Protection and Affordable Care Act, which requires communities to conduct health assessments every 3 years to maintain their tax-exempt status (27). Key partners, including local public health departments, can help address health disparities by collaborating with nonprofit organizations which are working to improve education. States such as Rhode Island have found an achievement gap between Hispanic and White students (28). During 2018, education levels at or above high school completion were higher among White (90.2%) and Black (87.9%) persons than Hispanic persons (71.6%) in the United States (29). In the current analysis of data from 2017-2021, education levels at or above high school completion were higher among White (93.5%) and Black (87.2%) persons than Hispanic persons (71.2%). Texas, California, New Mexico, and Rhode Island have a high proportion of Hispanics and reduced statewide educational attainment. However, because of other intrinsic factors, these states recorded lower adjusted all-cause and HIV mortality rates. Lastly, although we found higher HIV mortality rates among males than females in all states, the rates recorded among both males and females in the District of Columbia were exceedingly higher. The 14 states where HIV mortality rates are higher than the national average of 3.3/100,000 population in males should institute strategies to address this disparity.
The findings in this report are subject to certain limitations. First, this study is ecological, and a causal relationship cannot be established. The aim was to assess educational attainment and mortality by state; intrastate variations, demographic characteristics, medical advances, health care access and lifestyle changes among the population groups at the state level were not assessed. Second, we did not adjust for race/ethnicity, differences between high and low HIV prevalence states, comorbidities, urban or rural states, substance abuse, Covid-19 mortality, and sex-related differences in deaths. Third, because mortality data were used, determining the stages of diseases (underlying cause of death) and whether deceased persons took appropriate clinical actions during the illness course (stages) could not be determined. A longitudinal study or retrospective review of medical records is needed to answer that question. Fourth, because educational information is inadequately captured on death certificates, we had to use educational data from another source. Using education from the death certificate might overestimate death rates for those with high school-level attainment (30). Fifth, we were unable to conduct regression analysis at the state level and determine specific contributions of education at this level because we lacked individual-level data on educational attainment. Improved educational data on decedents would be needed to conduct this type of analysis. For example, the surveillance system used by the tuberculosis program, which collects this type of information, could be used as a model for collecting educational data. Six, rather than examining all-cause mortality for the entire population, ages ≥25 years (18) were selected to correspond with the educational attainment data set. The rationale for this selection was that by aged 25 years, adults are expected to have completed their high school education or the equivalent. Seven, other socioeconomic factors (e.g., income), lifestyle changes, or available healthcare resources that might influence mortality were not included. However, education is a strong determinant of future employment and income and captures the influence of adult circumstances on their health (1,3,18,31).
Although ecological, this study echoes the relationship between educational attainment and mortality and the importance of reducing disparities in education to improve health (32). State health and education agencies should continue to collaborate on improving educational attainment for their residents.
Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Declaration of Conflicting Interests: Authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Data availability: The datasets used during analysis are available to the public at the referenced websites.
Funding: Authors received no funding for this work.
Authors’ contributions: Nelson (conceptualization, writing, review and editing). Man-Huei (data analysis, review, and writing).
Consent for publication: Authors give permission for publication.
Ethics approval: This analytic study did not involve human subjects research supervised by an Institutional Review Board. [1] Mortality & educational attainment data for the three major racial and ethnic groups (i.e., “NHW”, “Black”, and “Hispanic”) as an Appendix. Data on educational attainment for race/ethnicity for Non-Hispanic Blacks aged >=25 are NOT available in ACS. Therefore, the mortality data along with the educational attainment data in the Appendix was created for “Black or African American Alone” in which all ethnic origins (i.e., Hispanic, non-Hispanic, Latinos, or not stated) were included. Data on each racial and ethnic group were listed separately in each table by sex and in total. We only included this information as a supplemental material.