International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 9 - Issue 1 - 2026
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
Hafiza Faiza Noor 1, Dr. Saba Afzal 2, Dr Mariyam Shabbir 3, Dr Ashfaq Ahmad 4
Institute of Biotechnology and Genetic Engineering, University of Sindh, Jamshoro, Pakistan.
*Corresponding author: Hafiza Faiza Noor, Institute of Biotechnology and Genetic Engineering, University of Sindh, Jamshoro, Pakistan.
Received: April 05, 2025 Accepted: April 10, 2025 Published: April 21, 2025
Citation: Hafiza Faiza Noor. (2025) “Instant Effect of Self Stretching Exercises on Pain, Functionality and Muscle Spasticity, In Lower Limb Orthosis Users”. International Journal of Epidemiology and Public Health Research, 6(2); DOI: 10.61148/2836- 2810/IJEPHR/123.
Copyright: © 2025. Hafiza Faiza Noor. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited., provided the original work is properly cited
Background: The mobility and quality of life of those who use lower limb orthoses may be adversely affected by pain, muscular stiffness, and functional restrictions. The objective of this study is to investigate the instant effects of self-stretching exercises on pain, muscle spasticity, and functionality in individuals who use lower limb orthoses.
Methodology: A structured survey was given to patients receiving physiotherapy as part of this cross-sectional study (comparative analytical study) to track the immediate impact of self-stretching exercises on lower limb orthosis users' discomfort, functioning, and muscular stiffness. 111 patients undergoing physiotherapy sessions participate in cross-sectional research. There were 111 participants in the trial. Participants who meet the inclusion criteria, completed standardised questionnaires such as the Lower Extremity Functional Scale (LEFS), Modified Ashworth Scale (MAS), and Numeric Pain Rating Scale (NPRS), and the results were recorded. Data was collected twice a time from same patients firstly before stretching and second after providing stretching. Data is analysed through SPSS v. 27.
Results: The mean age of the participants was 53.23 years. Mean BMI of 25.54 with a standard deviation of 6.28. The mean pre-stretch score was 41.65 ± 3.14, while the mean post-stretch score increased to 47.26 ± 2.54. The p-value (P<0.001) indicates that this difference is statistically significant, suggesting that instant self-stretching had a meaningful impact on functional improvement. The mean pre-stretch pain score was 4.92 ± 0.88, which decreased to 3.46 ± 1.02 post-stretch. The p-value (P<0.001) indicates that this reduction is statistically significant, suggesting that instant self-stretching effectively alleviated pain. The mean pre-stretch score was 3.13 ± 0.88, which decreased to 1.38 ± 1.02 post-stretch. The p-value (P<0.001) indicates that this reduction is statistically significant, suggesting that instant self-stretching effectively reduced muscle spasticity.
Conclusion: Current study's results demonstrated that self-stretching activities help people using lower limb orthoses by reducing discomfort, reducing muscular stiffness, and improving their functional abilities in a timely and statistically meaningful manner.
Introduction:
The purpose of lower limb orthoses (LLOs) is to align and support the lower extremities' bones, joints, and muscles. LLOs are frequently used to help people maintain stability, movement, and posture in illnesses such multiple sclerosis, spinal cord injuries, stroke, cerebral palsy, and orthopaedic problems (1). These tools are crucial for improving mobility and halting the progression of deformities or functional limitations. But long-term orthosis use can also result in problems including discomfort, stiffness, and spasticity in the muscles, especially in the lower limbs. Mobility, independence, and general quality of life may all suffer as a result of these difficulties (2).
People who use lower limb orthoses frequently suffer from a variety of secondary issues, such as decreased range of motion, muscular tightness, and persistent discomfort. Users of orthoses, particularly those with neurological problems, are more likely to have spasticity, a disorder marked by increased muscular tone and uncontrollable muscle spasms (3). Spasticity can significantly impair movement and functioning, making everyday tasks like standing, walking, and changing positions more challenging. The aberrant mechanical forces that orthoses impose on muscles and joints can also result in the development of pain, both acute and chronic (4).
Along with pain and spasticity, people who wear orthoses often have a loss of muscle and joint flexibility, which results in decreased functionality, which can be reflected in a decreased capacity to engage in physical activities or perform basic tasks, which further complicates rehabilitation efforts and reduces overall independence (5). A variety of interventions, such as physical therapy, medication, and exercise regimens, have been used to counteract these effects, but one strategy that has drawn attention due to its immediate and accessible benefits is self-stretching exercises (6).
It is commonly known that stretching exercises can increase muscular relaxation, decrease discomfort and stiffness, and improve flexibility. Particularly with self-stretching, people are empowered to actively manage their symptoms. These exercises target regions of stiffness or pain by using a series of controlled, prolonged motions to lengthen and relax certain muscle groups (7). Self-stretching works because it can enhance joint mobility, decrease muscle stiffness, and increase blood flow to the muscles. Stretching the muscles around the hips, knees, and ankles is especially crucial for those using orthoses because these regions frequently experience less mobility and increased tension. Regular stretching exercises can help people feel less pain, have less stiffness in their muscles, and be more functional overall (8).
This study aims to determine the immediate effects of self-stretching activities on lower limb orthosis users' discomfort, muscular stiffness, and functioning. The study's specific goal is to determine if a single session of self-administered stretching exercises by a physiotherapist may result in these areas improving right away. The capacity to provide immediate pain and spasticity relief might greatly improve the everyday experiences and quality of life for people in this community, especially considering the chronic nature of the illnesses that frequently call for the usage of orthoses. Furthermore, there are significant clinical practice ramifications of this research. Clinicians and physical therapists may include self-stretching exercises in customised treatment plans for orthosis users by showcasing the immediate advantages of doing so. This study provides patients with easy-to-implement methods to handle their symptoms on their own. The results of the study also aid in the creation of standardised self-stretching exercises that orthosis users may readily learn and practise in a range of contexts.
Methodology:
A structured survey was given to patients receiving physiotherapy as part of this cross-sectional study (comparative analytical study) to track the immediate impact of self-stretching exercises on lower limb orthosis users' discomfort, functioning, and muscular stiffness. 111 patients undergoing physiotherapy sessions participate in cross-sectional research. There were 111 participants in the trial. The inclusion criteria for this study consist of patients aged between 40-65 years, including both males and females, who are currently using an orthotic device and can perform self-stretching exercises independently. Eligible participants must have received at least one session of stretching exercises and have musculoskeletal disorders such as plantar fasciitis, Achilles tendon injuries, or osteoarthritis and rheumatoid arthritis of the ankle. Conversely, the exclusion criteria include patients with neurological disorders like cerebral palsy, stroke, multiple sclerosis, and spinal cord injury, as well as those who have undergone surgery in the last six months, have a history of fractures or ankle instability, or suffer from uncontrolled comorbid conditions. Participants who meet the inclusion criteria completed standardised questionnaires such as the Lower Extremity Functional Scale (LEFS), Modified Ashworth Scale (MAS), and Numeric Pain Rating Scale (NPRS), and the results were recorded. Data was collected twice a time from same patients firstly before stretching and second after providing stretching.
Results:
The mean age of the participants was 53.23 years. Mean BMI of 25.54 with a standard deviation of 6.28. 53.2% was males compared to females (46.8%) Majority have been using it for 3-5 years (34.2%) FO and KAFO, with each being used by 34.2%. The mean pre-stretch score was 41.65 ± 3.14, while the mean post-stretch score increased to 47.26 ± 2.54.
Table 1. LEFS Score
|
N=111 |
Mean ± SD |
p-value |
|
LEFS (PRE) |
41.64 ± 3.14 |
P<0.001 |
|
LEFS (POST) |
47.26 ± 2.54 |
The LEFS scores for 111 participants show a significant improvement after instant self-stretching. The mean pre-stretch score was 41.65 ± 3.14, while the mean post-stretch score increased to 47.26 ± 2.54. The p-value (P<0.001) indicates that this difference is statistically significant, suggesting that instant self-stretching had a meaningful impact on functional improvement.
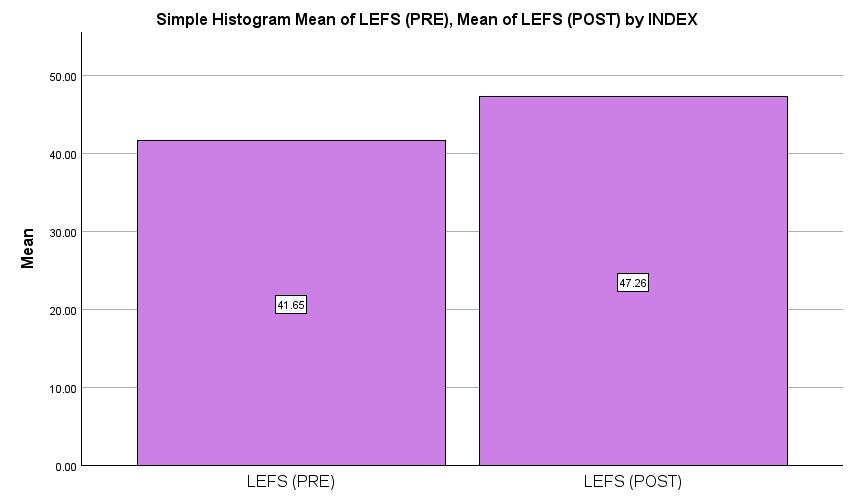
Figure1: LEFS Scores
|
N=111 |
Mean ± SD |
p-value |
|
|
NPRS (PRE) |
4.918 ± 0.875 |
P<0.001 |
|
|
NPRS (POST) |
3.459 ± 1.02 |
||
Table 2: NPRS Scores
The NPRS scores for 111 participants show a significant reduction in pain after instant self-stretching. The mean pre-stretch pain score was 4.92 ± 0.88, which decreased to 3.46 ± 1.02 post-stretch. The p-value (P<0.001) indicates that this reduction is statistically significant, suggesting that instant self-stretching effectively alleviated pain.
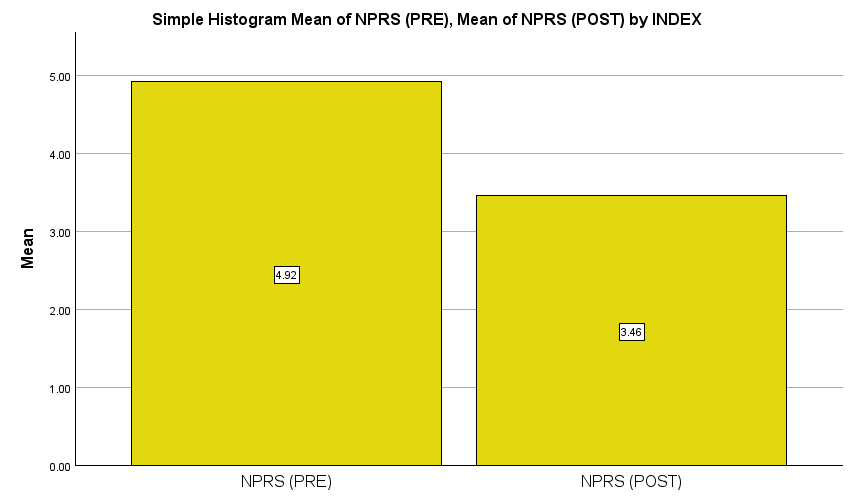
Figure 2: NPRS Scores
|
N=111 |
Mean ± SD |
p-value |
|
|
MPS (PRE) |
3.13 ± 0.87 |
P<0.001 |
|
|
MPS (POST) |
1.38 ± 1.02 |
||
Table 3: MAS Scores
The Modified Ashworth Scale (MAS) scores for 111 participants show a significant reduction in muscle spasticity after instant self-stretching. The mean pre-stretch score was 3.13 ± 0.88, which decreased to 1.38 ± 1.02 post-stretch. The p-value (P<0.001) indicates that this reduction is statistically significant, suggesting that instant self-stretching effectively reduced muscle spasticity.
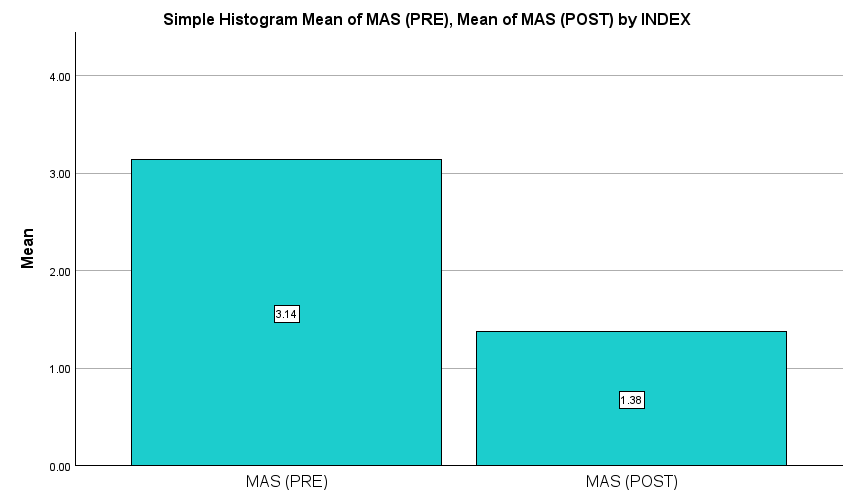
Figure 3: MAS SCORES
DISCUSSION
Previous research has examined the immediate benefits of self-stretching exercises on pain, muscular stiffness, and functioning in people who use lower limb orthoses; however, the results are still not entirely consistent. With statistically significant increases in pain alleviation, muscle stiffness reduction, and functional augmentation, the current study offers more proof of the effectiveness of self-stretching. While these findings differ from others in terms of the extent and persistence of effects, they are consistent with another earlier research. Stretching exercises have been repeatedly demonstrated in prior research to help people with neuromuscular disorders, including those who use lower limb orthoses, feel less discomfort(9).
Static stretching therapies, for example, resulted in a moderate drop in pain scores immediately after the exercise, with reported pain reductions ranging from 15% to 30% depending on the stretching frequency and duration, according to a research by Gracies et al. (2019)(10). Similarly, frequent stretching is linked to considerable pain alleviation, especially for people with diseases related to spasticity, according to a comprehensive analysis by Harvey et al. (2018)(9).
The mean pre-stretch pain score dropped from 4.92 ± 0.88 to 3.46 ± 1.02 post-stretch, with a statistically significant p-value (P<0.001), supporting these findings. This decrease, which translates to a roughly 30% drop in pain levels, is in line with other studies. Nonetheless, some earlier research, as that done by Ryan et al. (2020), contends that pain relief can be temporary and driven more by psychological variables than by physiological adjustments(11). In contrast to current study, which concentrated on immediate results, Ryan et al. looked at long-term changes and found that pain reduction was not maintained in the absence of ongoing stretching therapies. This disparity emphasises the need for more longitudinal research to ascertain how long self-stretching reduces discomfort(12).
Stretching exercises have long been suggested as a non-invasive strategy to address muscle stiffness, which is a major problem for those using lower limb orthoses. According to research by Bressel et al. (2017) and Alhusaini et al. (2021), passive stretching can modify muscle tone and modulate neuronal excitability to temporarily reduce spasticity. The mean pre-stretch spasticity score dropped dramatically from 3.13 ± 0.88 to 1.38 ± 1.02 post-stretch (P<0.001), which is consistent with our findings. This implies that self-stretching activities can successfully lessen spasticity in the short term(13, 14).
Other research, however, yields contradictory findings. For instance, a review by Avela et al. (2019) found that although stretching might temporarily lessen spasticity, the benefits usually wear off within 10 to 30 minutes. Furthermore, they discovered that too much stretching may cause a negative reaction in which muscles become more rigid as a defence(15). Even though present didn't evaluate how long spasticity reduction lasts, our cohort's statistically significant improvements indicate that self-stretching offers instant relief, which calls for more research into how long it lasts and the best stretching techniques(16).
For those who use lower limb orthoses, increasing functionality is essential since mobility issues have a big influence on their quality of life. Stretching therapies have been shown in prior research to improve gait efficiency, range of motion, and overall functional performance. According to their research, a 4-week stretching program improved functional scores by 10–15%, confirming the idea that frequent stretching improves movement efficiency(17).
These results are further supported by current study, which showed an improvement in the mean functional score from 41.65 ± 3.14 to 47.26 ± 2.54 (P<0.001). This indicates that even a single self-stretching session can have quantifiable benefits since it represents a considerable instant improvement in functioning. However, research by Gajdosik (2019) and Nakamura et al. (2020) suggests that although acute stretching therapies improve functioning in the near term, regular commitment to a stretching regimen is necessary for long-term functional benefits. This viewpoint supports the immediate advantages of our study but emphasises the need for more research on long-term, persistent changes(11).
Conclusion:
Current study's results demonstrated that self-stretching activities help people using lower limb orthoses by reducing discomfort, reducing muscular stiffness, and improving their functional abilities in a timely and statistically meaningful manner. Current results highlighted the significance of self-stretching as a straightforward yet successful intervention, despite some variations in the strength and duration of benefits.
Limitations And Recommendations
Although current study provides strong evidence for the instant advantages of self-stretching, it is important to recognise a number of limitations.
First off, the study did not evaluate long-term changes in pain, stiffness, or functioning; instead, it only examined acute impacts. In order to ascertain if benefits are sustained over the course of days, weeks, or months, future studies should incorporate follow-up evaluations.
Second, current research did not distinguish between various stretching methods (such as static vs dynamic stretching), which could have an impact on results. Future research should examine the effects of different stretching techniques on functioning, pain alleviation, and spasticity reduction. Furthermore, individual differences in response to stretching deserve additional investigation, especially with regard to variables like age, BMI, and underlying neuromuscular disorders, even if our findings are statistically significant.
Finally, current study did not assess behavioural or psychological aspects like motivation or stretching adherence. According to research by McCrory et al. (2021), an individual's degree of participation may have an impact on how beneficial stretching is regarded, which might help to explain some of the variation in results. Qualitative evaluations should be used in future research to provide a deeper understanding of participant experiences and adherence issues.