International Journal of Epidemiology And Public Health Research
OPEN ACCESS | Volume 9 - Issue 1 - 2026
ISSN No: 2836-2810 | Journal DOI: 10.61148/2836-2810/IJEPHR
Cameron Y. S. Lee, DMD, MD, PHD, MPH, MSEd.
Oral Maxillofacial and Reconstructive Surgery. Aiea, Hawaii 96701. The University of Chicago. Graham School. Chicago, IL. 60637.
*Corresponding author: Cameron Y. S. Lee, DMD, MD, PHD, MPH, MSEd, Oral Maxillofacial and Reconstructive Surgery. Aiea, Hawaii 96701. The University of Chicago. Graham School. Chicago, IL. 60637.
Received: February 09, 2024
Accepted: February 13, 2025
Published: February 25, 2025
Citation: Cameron Y. S. Lee. (2025) “The Public Health Effects of the Maui and Southern California Wildfires from Smoke Inhalation and Air Pollutants: Risk of Venous Thromboembolism and Life-Threatening Pulmonary Embolism”. International Journal of Epidemiology and Public Health Research, 6(1); DOI: 10.61148/2836- 2810/IJEPHR/105
Copyright: © 2025. Cameron Y. S. Lee. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited., provided the original work is properly cited.
Air pollution from the 2023 Lahaina, Maui and ongoing 2025 Southern California wildfires negatively impact the environment and population in nearby communities. Understanding the public heath effects of particulate matter with an aerodynamic diameter less than 2.5 um (PM 2.5) as one of the most harmful air pollutants is not well understood. While there is evidence that wildfire smoke is harmful to the cardiovascular system, there is a paucity of information regarding development of life-threatening acute pulmonary embolism (PE) from venous thromboembolism (deep vein thrombosis) of the lower extremity due to fine particulate matter (PM2.5). This paper will describe exposure to wildfire air pollutants such as particulate matter as an independent risk factor for the development of venous thromboembolism leading to acute pulmonary embolism that is a medical emergency as it can be life-threatening.
Introduction
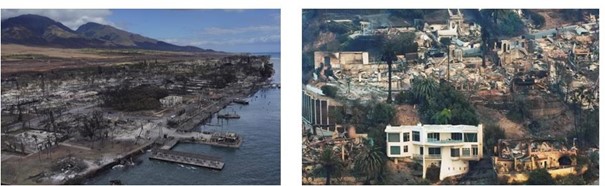
The August 2023 Lahaina, Maui and ongoing 2025 Southern California wildfires (Figure 1) are a significant public health threat that caused extensive loss of property, morbidity, and mortality [1, 2]. Over 100 people were killed in the Lahaina wildfire,[3] while economic losses from the California wildfire are estimated at over $50 billion. Both wildfires left thousands homeless, destroyed businesses and will have a profound impact on the environment and economy for decades.
There are many published articles on the health effects of air pollution from particulate matter due to smoke inhalation that affects the cardiovascular and respiratory system [4, 5, 6]. Further, there is an association between wildfire smoke inhalation and all-cause mortality [7]. Vulnerable populations include children under five years of age and adults 65 years and older with existing cardiovascular and respiratory problems are especially susceptible to the effects of inhaled smoke [8, 9, 10].
Exposure to wildfire smoke can exacerbate cardiovascular conditions, such as myocardial infarction and cardiac arrests [11] and respiratory conditions, such as asthma, chronic obstructive pulmonary disease (COPD), bronchitis, pneumonia, and lead to acute pulmonary embolism formation, [1, 12, 13] Common risk factors for venous thromboembolism of the deep veins of the lower extremity includes age, hypertension, hyperlipidemia, obesity, and diabetes mellitus [14, 15].
However, there is a paucity on the relationship between wildfire air pollutants and thromboembolism of the lower extremity. This paper will focus on acute pulmonary embolism from deep vein thrombosis due to particulate matter from smoke inhalation as particulate matter is a dangerous form of air pollution.
Wildfire Smoke and Air Pollutants
Both wildfires exposed entire communities to toxic materials in the ash from the burning of buildings, wood, vegetation, automobiles, and toxic metals [16, 17] Such toxic metals include arsenic, lead, copper, cobalt, and antimony that are commonly found naturally in rock and soil and consumer products [16-18]. Ash samples collected were above levels determined to be safe by the department of public health (Maui DOH, 2024) [16]. Secondary air pollutants detected include carbon monoxide, nitrogen dioxide, and carcinogenic polycyclic aromatic hydrocarbons.
Air pollution is a heterogenous mixture of particulate matter, and solid and liquid gases of various chemical composition traveling in the environment. Particulate matter are solid compounds suspended in air that can be inhaled due to its extremely small size [1, 6].
Particulate matter of natural origin is non-toxic, such as dust, and dirt and visible in the environment. In contrast, anthropogenic particulate matter are substances that cause air pollution. Examples include particle pollution from automobile emissions, industry smoke and burning of agriculture [19]. Chronic obstructive pulmonary disease (COPD) and asthmatic conditions worsen as the lung is the main organ for particulate matter pathophysiology [20].
Figure 1.
Left. 2023 Maui Wildfire. The ruins of historic Lahaina. (Kevin Fujii/Civil Beat/2023).
Right. 2025 Southern California wildfire. Pacific Palisades neighborhood of Los Angeles. (AP Photo/Mark J. Terrill).
Fine Particulate Matter (PM2.5) and Deep Vein Thrombosis (DVT)
Aerodynamic fine particulate matter less than 2.5 um in diameter (PM 2.5) is a toxic material in smoke that can be inhaled into the lungs and cause systemic inflammation, oxidative stress, and coagulation as they can enter the circulatory system [1, 6] Wildfire smoke, such as PM2.5 can be ten times more toxic than particulate matter from other sources, as they also contain toxic gases such as carbon monoxide, nitrogen oxides, and volatile organic compounds [5].
Annually, greater than one million people in the United States are diagnosed with lower extremity deep vein thrombosis as the etiology for pulmonary embolism [21]. A study by Brook et al [22] reported on the negative effects of air pollutants on the coagulation system. Exposure to long-term air pollutants increase the risk of DVT, as air pollutants can induce platelet aggregation, and dysfunction of the endothelial lining of the veins [23, 24, 25, 26] Studies by Gwon and colleagues [27] and Bumroongkit et al [28] also demonstrated that long-term exposure to particulate matter less than 10um (PM10) is associated with an increased incidence of lower extremity DVT and pulmonary embolism that can be life- threatening.
Several studies showed the association of an increase in levels of inflammation and coagulation biomarkers [15, 29]. Increased levels of D-dimer and C-reactive protein (CRP) are used to evaluate the development of a blood clot, while the CRP test is used to evaluate levels of inflammation. Both tests are elevated with exposure to fine PM 2.5 [29] Lastly, Kloog et al [30] showed that PM2.5 exposure is associated with DVT and increased rates of hospital admission.
Conclusion
The loss of life and destruction of property caused by the Maui and Southern California wildfires highlight the need for preventing future wildfires of this magnitude. Both wildfires have released enormous amounts of air pollutant emissions that will affect the environment and health of the public for decades. Healthcare and public health clinicians must educate the community about the health risks from wildfires, and disaster planning. Lastly, more clinical studies are needed to understand the health consequences of acute pulmonary embolism from deep vein thrombosis due to smoke inhalation that can be life-threatening.
Conflict of Interest
The author declares no conflict of interest relevant to this paper.