International Journal of Clinical Otorhinolaryngology
OPEN ACCESS | Volume 2 - Issue 1 - 2025
ISSN No: - | Journal DOI: -
Alene Meshesha1, Uta Fröschl1, Michael Kebede1, Tolesa Diriba Biratu2, Fufa Hunduma2, Yoseph Worku2, Waltengus Birhanu1*
1Department of Otolaryngology- Head and Neck Surgery, School of Medicine, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia.
2Department of Epidemiology, School of Public Health, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia.
*Corresponding author: Waltengus Birhanu, Department of Otolaryngology- Head and Neck Surgery, St. Paul’s Hospital Millennium Medical College, Addis Ababa, Ethiopia.
Received: December 01, 2025 | Accepted: December 06, 2025 | Published: December 12, 2025
Citation: Meshesha A, Frösch U, Kebede M, Tolesa D Biratu, Hunduma F, Worku Y, Birhanu W. (2025) “Tympanic Membrane Status and Associated Factors Among the Ethiopian Population: Evidence From the 2023 National Ear and Hearing Survey.” International Journal of Clinical Otorhinolaryngology, 2(1); DOI: 10.61148/IJCO/004.
Copyright: © 2025 Waltengus Birhanu. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objective:
Ear health is integral to overall well-being, and abnormalities in the eardrum can significantly impact hearing and quality of life. This study aims to assess the prevalence and determinants of abnormal tympanic membranes in Ethiopia, considering factors such as socioeconomic conditions and regional variations.
Methods:
A nationwide survey was conducted using the World Health Organization's Ear and Hearing Survey Handbook. Participants from all regions of Ethiopia were enrolled through a multi-stage sampling procedure, with a sample size of 3,000 households. The study utilized otoscopic examinations, audiometry, tympanometry, demographic surveys, and interviews to collect data on abnormal tympanic membrane status and relevant variables.
Results:
Out of 9,966 participants, 9.1% had abnormal tympanic membranes, with perforation being the most common tympanic membrane abnormality (5.3%). Factors associated with abnormal tympanic membranes included sex, region, number of rooms the participants household had, and history of ear discharge. Males, participants from specific regions, and those with a history of ear discharge had higher odds of abnormal status of the tympanic membrane.
Conclusion:
This nationwide Ethiopian study effectively quantifies the substantial burden of abnormal tympanic membranes, revealing a prevalence of 9.1% with perforation as the leading abnormality. The identified determinants sex, specific regional disparities, history of ear discharge, and crowded housing conditions provide crucial insights for public health interventions. These findings underscore the urgent need for targeted strategies focusing on ear health education, early detection, and improved living standards to mitigate the significant impact of these conditions on hearing and overall quality of life in Ethiopia.
Abnormal tympanic membrane, prevalence, determinants, ear health, Ethiopia, survey
Ear health is an important aspect of overall health, and abnormalities in the eardrum can significantly impact hearing function and quality of life. 1 The eardrum serves as an important barrier between the outer ear and middle ear, facilitating sound transmission and protecting the delicate structures of the ear. 2
Abnormalities of the eardrum, such as perforation, retraction, or inflammation, can lead to hearing loss, recurrent ear infections, and other complications if left untreated. 3 Understanding the prevalence and determinants of abnormal tympanic membranes is important for estimating the severity of the problem and identifying population groups at higher risk. Identifying factors associated with tympanic membrane abnormalities may also provide insight into the underlying factors that contribute to the disease and may inform interventional measures, targeted policies, and resource allocation to effectively address the burden of ear-related disorders. 4
Ethiopia faces a number of ear health challenges: limited access to health care facilities, inadequate awareness of ear health, and socioeconomic disparities contribute to the burden of ear-related disorders. 5 Although previous studies have explored various aspects of ear health in Ethiopia, the prevalence and determinants of abnormal tympanic membranes remain understudied. 5 Several potential determinants may contribute to the abnormality of the eardrum. Socioeconomic factors, such as income level, education level, and occupation, may influence access to health services and perceptions of ear-health care practices. 6
Environmental factors, including exposure to noise pollution, poor hygiene, and crowded living conditions, may also play a role in the prevalence of abnormal eardrum conditions. 7 Environmental factors, including exposure to noise pollution, poor hygiene, and crowded living conditions, may also play a role in the prevalence of abnormal eardrum conditions. 8 Differences in health care infrastructure, cultural practices, and environmental conditions across regions may influence hearing health outcomes. 6 Therefore, a comprehensive understanding of the regional distribution and determinants of abnormal tympanic membrane conditions is essential to developing region-specific policies and interventions.
The results of this study will have important implications for public health policies and hearing health interventions in Ethiopia. By identifying the determinants associated with abnormal eardrum status, our study will contribute to evidence-based strategies to reduce the burden of ear-related disorders. Furthermore, the study will highlight regional differences in abnormal eardrum conditions, highlighting the need for tailored interventions to address specific challenges in different regions of Ethiopia. To address these research gaps, we conducted a nationwide survey to assess the prevalence and determinants of abnormal tympanic membranes in Ethiopia in 2023.
Methods
Ethical clearance for this study was given by the Institutional Review Board of St. Paul’s Hospital Millennium Medical College. The study was conducted based on the World Health Organization’s (WHO) Ear and Hearing Survey Handbook. 9 The handbook has well-stipulated procedures and methods to conduct national surveys, and it has been used by different nations that have implemented similar population-based surveys.
Study design and participants
We conducted a population-based national survey by enrolling participants from all over Ethiopia from February to June 2023. Ethiopia is the second-most populous country in Africa, with a population exceeding 105 million, and is found in the north-eastern part, also known as the Horn of Africa. 10 The study participants were all household members residing in randomly selected enumeration areas (EAs) in 12 regional states and city administrations in Ethiopia. The Tigray region was not included in the study due to serious security concerns in this part of the country at the time of data collection. All people who had lived at least six months in the residence area were included. People who were not permanent residents of Ethiopia, local visitors, and critically ill and mentally disabled individuals that were unable to communicate easily for the ear and hearing examination were excluded from the study.
Sample size determination and sampling procedures
We calculated sample size using the single population proportion formula by considering 95% confidence interval (CI), 0.011 margin of error, 4.5% expected prevalence of abnormal tympanic membrane status based on WHO’s estimate 9, a design effect of two because of the multi-stage sampling procedure, and a 10% addition for the non-response. Accordingly, the estimated sample size was 3,000 households. To recruit the study participants, we used the sampling frame prepared by the Ethiopian Statistical Service (ESS). The sampling frame is used for all national surveys and censuses. The national sampling frame uses EAs from all the regions and city administrations. EAs are well-delineated geographic areas that include an average of 131 households (170 in urban and 119 in rural settings). 10 We employed a multi-stage sampling procedure. The primary sampling units were the EAs, and the secondary sampling units were households. A proportional number of EAs were allocated for each region and city administration based on the total number of EAs in the respective regions and city administrations. From every EA, 30 households were randomly selected, and from every randomly selected household, all eligible household members were recruited for the study.
Variables and definitions
The dependent variable of this study was abnormal tympanic membrane status, which is defined as the presence of any form of abnormality of the tympanic membranes during otoscopic examinations. The abnormalities included perforation, being dull and retracted, being red and bulging, and cholesteatoma. The independent variables included sociodemographic variables (age, sex, educational status, residence, region, occupation, and number of rooms), history of ear discharge, and history of tinnitus.
Data collection and management
We used the standard data collection tool prepared by the WHO. The tool was originally prepared in English and translated to Amharic and Afan Oromo local languages. Most of the study participants from all the 12 regional states and city administrations were able to communicate with the Amharic language. Translators were used if the study participants and examiner did not speak the same language. The components of the survey tool used for this study were demographics, history of ear symptoms, ear examination findings, and possible causes of ear diseases. We collected electronic data using tablets and Open Data Kit (ODK) software. The data were collected by field teams comprised of ENT specialists, ENT residents, nurses trained as ear and hearing care workers, and health extension workers. The ear examinations were performed by the ENT residents from St. Paul’s Hospital Millennium Medical College, who received prior additional training on the whole process of data collection. One ENT specialist worked as a supervisor of the data collection process. Ten teams of examiners traveled to various parts of the country to conduct the study. The data collection process involved an initial interview phase, where the examiners interviewed the study subjects and filled the questionnaire, followed by hearing evaluation and physical examination. All subjects had their ears examined by an ENT resident using otoscopes. To ensure data quality, different measures were taken: a data manager ensured the consistency, completeness, and accuracy of the data recording. A pilot study was conducted before the actual data collection, and the tools were revised according to the findings of the pilot results. The data collection was closely monitored.
Statistical analysis
The data were analyzed using IBM SPSS Statistics for Windows, Version 28 (IBM Corp., Armonk, NY, USA). To describe the demographic and symptom data, we used frequency distribution by calculating the percentages of the categories. The prevalence of abnormal tympanic membrane status was calculated as a proportion of the participants who had any form of abnormal tympanic membrane status out of all the participants. To identify the determinants of abnormal tympanic membrane status, we used simple and multiple binary logistic regression analyses. Variables that had p < 0.25 during the simple binary logistic regression analysis were entered into the final model of the multiple binary logistic regression analysis. We checked the key assumptions of the model. The Hosmer-Lemeshow test showed that the model had a good fit with p = 0.509. None of the independent variables showed multicollinearity. We used an adjusted odds ratio (AOR) with a 95% confidence interval (CI) to measure the associations between the independent variables and the abnormal tympanic membrane status. P < 0.05 was used to declare statistical significance.
Ethical considerations
The study was conducted after securing ethical clearance from the Institutional Review Board of St. Paul’s Hospital Millennium Medical College. The study participants were informed about their voluntary participation and their right to withdraw from the study. All adult study subjects provided their informed consent to take part in the research and gave their approval for their children to participate as well. Older children and adolescents also provided their informed assent to participate in the study. Privacy and confidentiality principles were strictly observed. Appropriate treatment or referral services were provided for study participants who were diagnosed with abnormal tympanic membrane status.
Results
In this survey, we enrolled a total of 9,966 study participants from all over Ethiopia, with a response rate of 99.6%.
Demographic profile of study participants
Females showed a slightly higher proportion among the study participants (5,626, 56.5%). The largest proportion of the population were within the 15–44 age range, accounting for 3,998 persons (40.1%). The 0–4 age group included 2,905 participants (29.1%). The older age groups, 45–60 and above 60, constituted smaller proportions at (834) 8.4% and (487) 4.9%, respectively. Around half of the participants (4,963, 49.8%) had no formal education. More than a third (3,513, 35.2%) had completed primary education. Those with tertiary education accounted for 498 (5.0%) of the participants. Six out of ten participants (6,010, 60.3%) lived in rural areas. Oromiya and Amhara accounted for 1,735 (17.4%) and 1,531 (15.4%) of the participants, respectively. Addis Ababa and Harari participants comprised 871 (8.7%) and 249 (2.5%), respectively. Most households had two rooms, accounting for 4,121 (41.4%) of the participants. One-room households represented 2,605 (26.1%) of the participants. [Table 1].
Table 1: Demographic profile of the participants of NEHS, Ethiopia, 2023
|
Variables |
Categories |
Frequency |
Percentage |
|
Sex |
Male |
4,340 |
43.5 |
|
Female |
5,626 |
56.5 |
|
|
Age in years |
0–4 |
2,905 |
29.1 |
|
5–14 |
1,742 |
17.5 |
|
|
15–44 |
3,998 |
40.1 |
|
|
45–60 |
834 |
8.4 |
|
|
> 60 |
487 |
4.9 |
|
|
Educational status |
None |
4,963 |
49.8 |
|
Primary |
3,513 |
35.2 |
|
|
Secondary |
992 |
10.0 |
|
|
Tertiary |
498 |
5.0 |
|
|
Residence |
Rural |
6,010 |
60.3 |
|
Urban |
3,956 |
39.7 |
|
|
Region |
Addis Ababa |
871 |
8.7 |
|
Afar |
793 |
8.0 |
|
|
Amhara |
1,531 |
15.4 |
|
|
Benishangul Gumuz |
367 |
3.7 |
|
|
Dire Dawa |
254 |
2.5 |
|
|
Gambella |
348 |
3.5 |
|
|
Harari |
249 |
2.5 |
|
|
Oromiya |
1,735 |
17.4 |
|
|
Sidama |
950 |
9.5 |
|
|
SNNPR |
1,487 |
14.9 |
|
|
Somali |
1,381 |
13.9 |
|
|
No of rooms |
One |
2,605 |
26.1 |
|
Two |
4,121 |
41.4 |
|
|
Three or more |
3,240 |
32.5 |
NEHS: National Ear and Hearing Survey. SNNPR: Southern, Nations, Nationalities, and Peoples Region
Self-reported ear symptoms and ear examination findings
In this survey, 571 (5.7%) of the participants reported having tinnitus (ringing, roaring, and buzzing) over the 12-month period before the data collection, while 557 (5.6%) of them reported a history of ear discharge. [Figure 1].
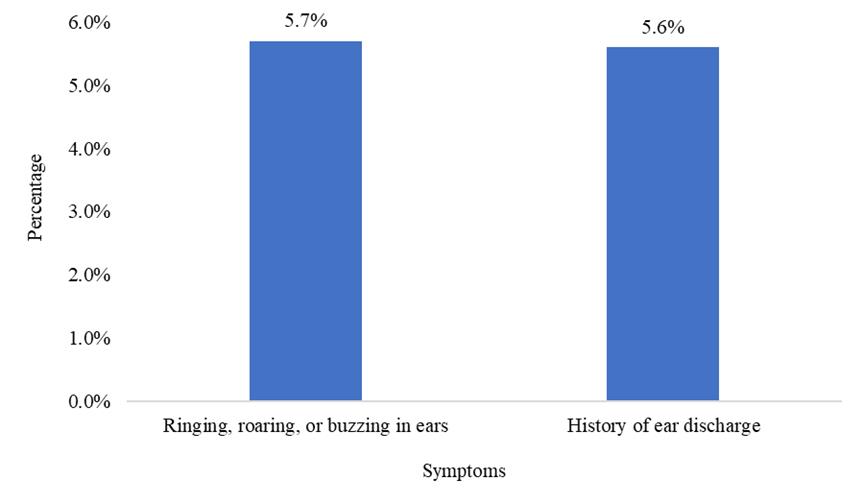
Figure 1: Self-reported ear symptoms by the study participants of NEHS, Ethiopia, 2023
NEHS: National Ear and Hearing Survey.
Only nine (0.1%) of the participants exhibited auricular malformation. Around one-tenth of the participants (916, 9.2%) had wax impaction in their ear canals. Inflammation, foreign body, and fungal infection (otomycosis) were observed in 48 (0.5%), 32 (0.3%), and 18 (0.2%) of the participants, respectively. [Figure 2]
Prevalence of abnormal tympanic membrane status
In this survey, 907 (9.1%) of the participants had an abnormal tympanic membrane. Perforation, middle ear discharge, as well as dull and retracted tympanic membrane were the abnormalities reported in 481 (5.3%), 258 (2.8%), and 237 (2.6%) of the participants, respectively. [Table 2].
Table 2: Tympanic membrane abnormalities among the study participants of NEHS, Ethiopia, 2023
|
Variable |
Category |
Frequency |
Percentage |
|
Tympanic membrane status |
Normal |
9,059 |
90.9 |
|
Abnormal |
907 |
9.1 |
|
|
Abnormalities of the tympanic membrane status* |
Dull and retracted |
237 |
2.6 |
|
Red and bulging |
128 |
1.4 |
|
|
Perforation |
481 |
5.3 |
|
|
Middle ear discharge |
258 |
2.8 |
|
|
Cholesteatoma |
18 |
0.2 |
NEHS: National Ear and Hearing Survey
*The sum of the abnormalities is >907 because of concomitant abnormalities.
Factors associated with abnormal tympanic membrane status
Based on the multivariable binary logistic regression analysis, sex, region, number of rooms, and history of ear discharge were the significant variables that were associated with the abnormal tympanic membrane status at p < 0.05.
Males were 1.31 times more likely to have an abnormal tympanic membrane compared to females. (AOR = 1.31; 95% CI: 1.05, 1.65). Compared to the study subjects from the capital, Addis Ababa, those from the Afar Region were 2.18 times more likely to have abnormal tympanic membrane status (AOR = 2.18; 95% CI: 1.17, 4.06). Similarly, participants from Dire Dawa City Administration were 2.50 times more likely to develop abnormal tympanic membrane status (AOR = 2.50; 95% CI: 1.06, 5.92). Study participants with a history of external or middle ear discharge were 33.27 times more likely to have an abnormal tympanic membrane compared to those without a history of discharge (AOR = 33.27; 95% CI: 22.05, 50.22). Study participants living in households with one room had a 40% increased chance of having abnormal tympanic membrane status as compared to those with three or more roomed houses (AOR =1.40; 95% CI: 1.03, 1.89). [Table 3].
Table 3. Multivariable binary logistic regression analysis for factors associated with abnormal tympanic membrane status, NEHS, Ethiopia, 2023.
|
Variable |
Category |
Tympanic Membrane status |
COR (95%CI) |
AOR (95%CI) |
P-value |
|
|
Abnormal n (%) |
Normal n (%) |
|||||
|
Sex |
Male |
453 (10.4) |
3,887 (89.6) |
1.28 (1.05, 1.57) |
1.31 (1.05, 1.65) |
0.019 |
|
Female |
454 (8.1) |
5,172 (91.9) |
1 |
1 |
|
|
|
Region |
Addis Ababa |
41 (4.7) |
830 (95.3) |
1 |
1 |
|
|
Afar |
106 (13.4) |
687 (86.6) |
3.12 (2.15, 4.54) |
2.18 (1.17, 4.06) |
0.014 |
|
|
Amhara |
112 (7.3) |
1,419 (92.7) |
1.60 (1.11, 2.31) |
1.16 (0.61, 2.22) |
0.652 |
|
|
Benishangul Gumuz |
18 (4.9) |
349 (95.1) |
1.04 (0.59, 1.84) |
1.02 (0.43,2.42) |
0.956 |
|
|
Dire Dawa |
32 (12.6) |
222 (87.4) |
2.92 (1.80, 4.74) |
2.50 (1.06, 5.92) |
0.037 |
|
|
Gambella |
29 (8.3) |
319 (91.7) |
1.84 (1.12, 3.01) |
1.15 (0.49, 2.72) |
0.752 |
|
|
Harari |
19 (7.6) |
230 (92.4) |
1.67 (0.95, 2.94) |
0.87 (0.32, 2.34) |
0.783 |
|
|
Oromiya |
120 (6.9) |
1,615 (93.1) |
1.50 (1.04, 2.17) |
0.90 (0.48, 1.68) |
0.746 |
|
|
Sidama |
77 (8.1) |
873 (91.9) |
1.79 (1.21, 2.64) |
0.86 (0.43, 1.70) |
0.666 |
|
|
SNNPR |
131 (8.8) |
1,356 (91.2) |
1.96 (1.36, 2.81) |
0.89 (0.48, 1.66) |
0.717 |
|
|
Somali |
222 (16.1) |
1,159 (83.9) |
3.88 (2.75, 5.47) |
1.47 (0.81, 2.67) |
0.202 |
|
|
History of external and middle ear discharge |
Yes |
449 (80.6) |
108 (19.4) |
81.25 (64.55, 102.27) |
33.27 (22.05, 50.22) |
<0.001 |
|
No |
458 (4.9) |
8,951(95.1) |
1 |
1 |
|
|
|
Number of rooms |
One |
292 (11.2) |
2,313 (88.8) |
1.58(1.32, 1.89) |
1.40(1.03, 1.89) |
0.032 |
|
Two |
375 (9.1) |
3,746 (90.9) |
1.25(1.06, 1.48) |
1.06(0.80, 1.41) |
0.685 |
|
|
Three or more |
240 (7.4) |
3,000 (92.6) |
1 |
1 |
|
|
NEHS: National Ear and Hearing Survey. COR: Crude Odds Ratio. AOR: Adjusted Odds Ratio. SNNPR: Southern, Nations, Nationalities, and Peoples Region
Discussions
There is limited data regarding the tympanic membrane status of the Ethiopian population. To develop effective preventive and treatment methodologies, it is essential to understand the significance of abnormal tympanic membranes and the factors contributing to these issues. This study reported a prevalence of 9.1% for abnormal tympanic membrane status among participants. The observed anomalies included perforation, middle ear discharge, and dull or retracted tympanic membranes. Perforation was the most common abnormality, accounting for 5.3% of cases, followed by middle ear discharge (2.8%) and dull/retracted tympanic membranes (2.6%).
Comparing these findings with existing literature, our reported prevalence contrasts with Berhanu et al. (2021), which revealed a prevalence of 0.8% for perforated tympanic membranes in a school screening of 1,351 children in the Tigray region 2. Since our study did not include Tigray, further research is needed to investigate disparities in tympanic membrane perforation rates among different regions of Ethiopia. Similar studies found a comparable prevalence of chronic suppurative otitis media, which often manifests as ear discharge and perforation of the tympanic membrane. These findings highlight the persistent burden of ear-related disorders in the country. A study from a tertiary setting in Nigeria revealed perforation as the commonest tympanic membrane abnormality, with a prevalence of 7.8%. 1 A descriptive cross-sectional study done in another tertiary care setting also showed perforation as the commonest tympanic membrane abnormality, with a prevalence of 24.15%.3 This discrepancy can be explained by methodological differences, including sample size, and selection criteria. The prevalence is higher than the 2.1% reported in a cross-sectional analysis among individuals aged 12 years and older in the United States. 11 This discrepancy can be attributed to less accessible health care facilities, individuals may not seek treatment for ear infections, leading to higher rates of tympanic membrane perforation.
We identified several factors associated with abnormal tympanic membrane status, including sex, region, family housing conditions, and history of ear discharge. Males were found to have a 1.31 times higher likelihood of having an abnormal tympanic membrane compared to females, consistent with research indicating a higher prevalence among males. 13 National Health and Nutrition Examination Survey in US, performed a cross-sectional analysis, According to this study, males and females have a relatively similar prevalence at 2.3% (95% CI, 1.6%–3.0%) among males and 2.0% (95% CI, 1.4%–2.6%) among females.11 Also our finding doesn’t go with study A cross-sectional study which was conducted at Creek General Hospital and United Hospital, Karachi, from 2019 to 2023 ear morbidities showed no significant variation by age or sex. 19
Regarding regional differences, participants from the Afar region and Dire Dawa City Administration had 2.18- and 2.50-times higher chances of having abnormal tympanic membranes compared to those from Addis Ababa. These findings highlight the importance of accounting for geographical variations in healthcare access, ecological factors, and social practices that may contribute to the increased prevalence of ear-related issues. Timely diagnosis and treatment of ear infection are crucial in addressing these disparities. This aligns with a study from the Himalayan region of Nepal, which also reported regional and ethnic differences in chronic otitis media prevalence. 13
A significant association was found between a history of ear discharge and abnormal tympanic membrane status. Participants with a history of outer or middle ear discharge were 33.27 times more likely to have an abnormal tympanic membrane, supporting the notion that ear discharge often indicates perforation. 16 Research in sub-Saharan Africa has identified a connection between hearing loss and factors such as chronic ear infections, earwax accumulation, advanced HIV, and tuberculosis.18
Additionally, family housing conditions were linked to abnormal tympanic membrane status. Individuals living in one-bedroom houses were 40% more likely to exhibit abnormalities compared to those living in houses with three or more rooms. Crowded living conditions can facilitate the spread of resistant strains and increase the risk of ear-related disorders, consistent with findings from other studies highlighting the effects of crowding on tympanic membrane changes. 17 20
These findings illuminate the significant burden of ear disease in the nation, particularly persistent otitis media, which can lead to long-term complications if untreated. Understanding the factors contributing to abnormal tympanic membranes such as gender, location, history of ear discharge, and family circumstances provides valuable insights into interventional planning. Interventions should focus on promoting ear health education, facilitating early detection and treatment of ear diseases, and improving environmental factors like housing conditions.
The study's limitations include its limited geographical scope, excluding regions like Tigray, which may affect generalizability. The cross-sectional design prevents establishing cause-and-effect relationships. Additionally, a lack of detailed methodology and reliance on potential self-reported data (e.g., ear discharge history) could introduce biases like recall bias.
Conclusions
This study highlights a significant burden of abnormal tympanic membranes in Ethiopia, with a 9.1% prevalence. Perforation is the most common issue. Key contributing factors include male sex, living in the Afar and Dire Dawa regions, a history of ear discharge, and crowded housing conditions. These insights are crucial for developing targeted interventions and improving ear health nationwide.
Acknowledgements
We acknowledge the significant contributions and collaboration of various individuals and organizations in the successful execution of the 2023 National Ethiopia Hearing Survey (2023 NEHS). Special thanks are extended to the Christian Blind Mission (CBM) – Ethiopia for the financial support and Dr. Diego Santana for his continuous professional advice. Dr. Sisay Sirgu's leadership at St. Paul's Hospital Millennium Medical College (SPHMMC) are also recognized. Additionally, Dr. Sena Dhugasa's dedication and the collective efforts of regional health bureaus, public health institutes, and other stakeholders were crucial. The study adhered to WHO guidelines and underwent thorough review by various experts. Gratitude is expressed to department of Otolaryngology- head and Neck Surgery at SPHMMC, Ethiopian Public Health Association (EPHI) along with the data collectors, administration staffs and drivers involved in the survey. In conclusion, we appreciate the commitment and collaboration of all individuals and organizations involved in the survey.
Authors’ note
Prior presentation: This paper has neither been presented at any conferences nor published in any other journal.
Declarations of conflicting interests
All the authors declared no conflict of interest.
Funding
The study was funded by the Christian Blind Mission – Ethiopia. The authors received no payment for the authorship or publication of this article.