Gastroenterology and Hepatology Research
OPEN ACCESS | Volume 6 - Issue 1 - 2025
ISSN No: 2836-2888 | Journal DOI: 10.61148/2836-2888/GHR
Abdelmoneim Gomaa Elhadidy1*, Khaled Farid 2, Ashraf Alsayed Matar 3, Mohamed El Sayed Eldan 4, Ahmed El Sayed Jabr 5, Hussein Ghoneim 6& Fathy Ebrahim elnagdy 7
1Hepatology& Gastroenterology Department, Damietta Fever and Gastroenterology Hospital, Ministry of Health and Population, Egypt.
2Tropical Medicine department., Mansoura University, Egypt.
3Gynecological and obstetric Department, Damietta General Hospital.
4 ,5,6 Internal Medicine Department, ICU unit Damietta General Hospital, Ministry of Health and Population, Egypt.
7Surgery department, Damietta Cardiology and Gastroenterology Center, Ministry of Health and Population, Egypt.
*Corresponding author: Abdelmoneim Gomaa Elhadidy, Hepatology& Gastroenterology Department, Damietta Fever and Gastroenterology Hospital, Ministry of Health and Population, Egypt.
Received: August 07, 2025 |Accepted: August 25, 2025 |Published: August 30, 2025
Citation: Abdelmoneim G Elhadidy, Farid K, Ashraf A Matar, Mohamed El Sayed Eldan, Ahmed El Sayed Jabr. (2025) “Hepatic Rupture In Help Syndrome Postpartum And Spontaneous Resolution Rare Case Report”. Gastroenterology and Hepatology Research, 6(1); DOI: 10.61148/2836-2888/GHR/062.
Copyright: © 2025. Abdelmoneim Gomaa Elhadidy. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited., provided the original work is properly cited.
HELLP syndrome is a rare complication of pregnancy that may result in serious consequences such as hepatic rupture, one of the most feared and potentially life-threatening complications. This article aims to carry out a literature review on hepatic rupture in the context of HELLP syndrome as well as to present one clinical case.2019.
Hepatic hematoma and rupture, HELLP syndrome, Conservative management
The HELLP syndrome (haemolysis, elevated liver blood tests and low platelets) is a serious complication in pregnancy characterized by haemolysis, elevated liver enzymes and low platelet count occurring in 0.5 to 0.9% of all pregnancies and in 10–20% of cases with severe preeclampsia.
Hepatic hematoma and rupture are rare complications of HELLP syndrome, first described by Weinstein in 1982. The incidence of subcapsular liver hematoma with rupture in pregnancies varies from 1/40000 to 1/250000 (1). Ten percent to 20% of patients with preeclampsia develop HELLP, and it may occur in the absence of hypertension or proteinuria (2,3).
Importantly, 25% of HELLP presentations occur postpartum, (4) typically within 48 hours of birth. (5), Hepatic hematoma is rare, estimated to complicate 0.4% to 1.9% of HELLP syndrome cases hepatic rupture associated with significant risk of maternal mortality.
It is characterized by microangiopathic hemolysis, thrombocytopenia and impaired hepatic function (6). It commonly occurs between 28 and 36 weeks of gestation, but it can also occur postpartum or even during labor (7). It is associated with a maternal mortality rate of 3.3%. However, when hepatic hematomas are present, or when hepatic rupture develops, mortality and morbidity rise significantly (8). Preeclampsia in pregnant women has been reported as about 28% and is a leading cause of maternal near miss and mortality (9).
We report on a 25-year-old Egyptian woman delivered her baby vaginally at 35 weeks of gestation. After 4 days admitted to Damietta general hospital complained severe anemia, investigation elevated liver enzymes, low platelets, and abdominal ascites (HELLP syndrome) received supportive therapy and diuretic the liver enzyme and platelets became were normal after 2 weeks but the amount of free fluid moderate to marked ascites not respond to diuretic. Abdominal US revealed mild enlarged liver, large well-defined hypoechoic mass anterior to the liver, normal spleen and moderate free fluid (Ascites) which aspirated as diagnostic which revealed Concentrated (old)blood Hemoperitoneum then triphasic CT revealed hepatic subcapsular hematoma and may be liver rupture. Repeated small aspiration done and managed conservatively with intensive monitoring and serial liver imaging to assess for progression
The patient was discharged two months after admission then follow up for four months. Case reports such as ours may contribute to the management of pregnancy complicated by hepatic hematoma and rupture of the liver capsule associated to HELLP syndrome.
Case Report
A previously healthy Twenty-five-year-old pregnant woman, primigravida, routine antenatal booking revealed normal blood pressure, complete blood count, normal urine specimen, delivered her baby vaginally at 35 weeks.
Four days of postpartum, the patient was transferred to Damietta general hospital and Obstetric department complained of severe anemia, right upper quadrant and shoulder pain, Blood pressure measurement was 100/70 mm Hg and laboratory studies gave the following results: ; white blood cell, 12200/mm3; hematocrit, 24.5%; hemoglobin, 7.6 mg/dl; platelet count, 36 x 103 µ/mL. serum aspartate aminotransaminase (AST), 1530 IU/L; serum alanine aminotransaminase (ALT), 1730 IU/L; serum lactate dehydrogenase (LDH), 865 IU/L; serum creatine was 4.8, Viral markers HAV, HBV, ANA, ASMA, Total IgG, CMV, HSV, EBV and HIV were negative.
A catheterized urine specimen demonstrated no proteinuria. abdominal ultrasound (US) showed a hypoechoic heterogeneous subcapsular mass, 12 x 5.5 mm in diameter, in anterior segment of right hepatic lobe, and also perihepatic, perisplenic, pelvic free fluid in the abdominal cavity with normal spleen. The patient diagnosed postpartum HELLP syndrome, Subcapsular liver hematoma. the patient was transferred to intensive care unit and surgical consultation which advised for conservatively followed up in the intensive care unit. Six units of packed red blood cells, 6 units of fresh-frozen plasma and corticosteroids had given to patient and her motion was limited. On 8th day after addition, laboratory findings were as follows: serum ALT 55 IU/L, serum AST 31 IU/L, serum LDH 267 IU/L, white blood cell 10500/mm3, hematocrit 32.8%, hemoglobin 11.4 mg/dl and platelet count 367 x 103 µ/mL. Blood pressure measurement was 120/80 mm Hg. Patient was stable hemodynamically but by repeated ultrasound examinations were performed at a daily basis to monitor the results of conservative approach revealed moderate peritoneal free fluid then started diuretics and after two weeks the amount of peritoneal fluid not decreased , hepatological consultation revealed moderate to marked peritoneal free fluid without portal Hypertion with stable hemodynamically , According to the Egyptian Club of Ascites (ECA) 2022, algorithmic diagnostic workup for evaluating adult patients with ascites when imaging showed no finding, diagnostic aspiration was done ((10) aspirated ascitic fluid which revealed Concentrated blood (old) hemoperitoneum as (fig 1)
(Fig 1)


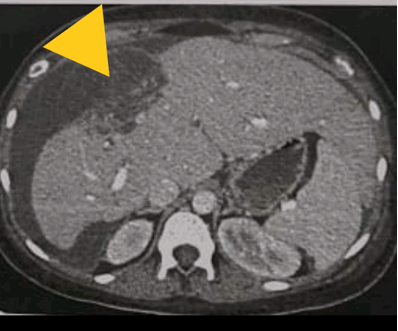
Computed tomography (CT) scan was performed to patient who revealed a Right lobe segment VIII subcapsular hypodense area measure 8*4*3cm with underlying liver capsule (subcapsular hematoma)
And marked free fluid in abdominal cavity (Fig 2).
(Fig 2).

The patient diagnosed postpartum HELLP syndrome, Subcapsular liver hematoma, and rupture liver, the patient referred to tertiary-level hospitals Menoufia liver institute for consultation as surgical intervention which he advised no surgical intervention with stable hemodynamically, repeated aspiration weekly 500ml and one packed RBCs transfusions for three weeks.
Two months postpartum follow up, the patient was mild free fluid, no complaint and discharged from the hospital in a stable status. Four months post-partum, USG examination of patient showed no residual hematoma or free peritoneal fluid.
Discussion
Spontaneous hepatic rupture is an uncommon condition and is mostly encountered in cases of benign and malignant disease of liver (11). Hepatic rupture in pregnancy is a rare entity and was first reported in 1844. During pregnancy, it has been reported as life threatening complication of preeclampsia and HELLP syndrome (12).
In HELLP the elevation of liver enzymes reflects the hemolytic process as well as ischemic liver injury in association with microthrombi. Doppler studies show reduced hepatic blood flow, in contrast to normal pregnancy in which increased portal blood flow occurs. Placental ischemia is thought to cause disseminated microangiopathy via placental release of anti-angiogenetic factors, necrotic debris, and cell-free DNA (from microvilli) that induces systemic endothelial dysfunction and a systemic inflammatory response. Red blood cell fragmentation results from shear stress as blood flows through turbulent areas of the microcirculation (liver and elsewhere) that are partially occluded by platelet and fibrin thrombi. Within the liver, the resulting ischemic injury triggers release of proinflammatory mediators, hepatocyte oxidative stress response, and enhanced liver cell injury(13(.
The most life-threatening liver-related complications are placenta abruptio, hepatic infarction, and rupture, occurring in 0.05% of preeclampsia/HELLP cases.(14). Rupture can occur postpartum, and symptoms include sudden onset of serve right upper quadrant or epigastric pain, referred right shoulder pain, or hypotension (15,16).
Prediction of hepatic rupture is poor due to lack of specific symptoms. Few studies correlated liver function tests and platelet count with hepatic rupture. Platelet count less than 1 × 105/cmm was the most common finding in these patients, though its role in predicting incumbent hepatic rupture is dubious and does not stand firm and established (17). Thus, diagnosis can be missed unless treating obstetrician has high index of suspicion.
Hepatic rupture is a rare but serious complication, occurring in 0.53% to 2% of women with preeclampsia and/or HELLP syndrome (18,19). The right lobe is most commonly involved (75% of cases).136 The reported maternal mortality rate was 7.5% in a recent review,135 decreased from prior summary estimates of 17% and 32% (20,21), and attributed to improved management. Late diagnosis is regarded as the main contributor to poor outcome, with a perinatal mortality of w40% (22,23).
In case of hepatic rupture, both conservative and surgical treatment is possible depending on the hemodynamic situation. The conservative approach should be preferred, including hemodynamic stabilization of the patient with blood products, volume substitution, and/or embolization of liver arteries with the option of switching to surgery when necessary (24,25, 26). Embolization of liver arteries represent a lower risk for the patient compared to surgery, and is possible even if multiple liver hematoma and/or coagulopathy are present. It can treat both liver hemorrhage as well as liver rupture (25,26) . Conversely, it can only be performed in specialized centers, the patient must be in stable circulatory condition, and necrosis of the liver or the biliary tract can complicate the recovery process (24,25,26). Alternative surgical methods are perihepatic packing, covering the hepatic fissure with absorbable meshes, fibrin glue, argon laser, hepatic artery ligation, liver transplantation, liver resection, or a combination of the methods (27).
In our case hemodynamic stable the conservative approach should be preferred and massive hemoperitoneum aspirated with backed RBCs replaced and follow up
Conclusion
Diagnosis of hepatic rupture/hematoma should be suspected in hypertensive pregnant women with complaints of epigastric pain, sudden pallor and hypotension either in antepartum or postpartum period. Abdomen distension should not be overlooked in postpartum period, the conservative approach should be preferred, including hemodynamic stabilization of the patient with blood products, volume substitutio
Acknowledgements
Not applicable.
Authors’ contributions
All authors are responsible for the modification and giving final approval of the manuscript. Abdelmoneim Elhadidy was a contributor in writing the manuscript. All authors read and approved the final manuscript.
Funding
The authors received no funding for this study.
Availability of data and materials
Please contact the corresponding author for data requests.
Declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests