Clinical Cardiology Interventions
OPEN ACCESS | Volume 5 - Issue 1 - 2025
ISSN No: 2836-077X | Journal DOI: 10.61148/2836-077X/JCCI
S. EJJEBLI*, A. ALTIMIMI, S. ABOULMAJD, J. JABBOURI, M. HABOUB, R. HABBAL
Cardiology, Ibn Rochd University Hospital Center, Casablanca, Morocco.
*Corresponding author: S. EJJEBLI, Cardiology, Ibn Rochd University Hospital Center, Casablanca, Morocco.
Received: April 01, 2025
Accepted: April 25, 2025
Published: May 12, 2025
Citation: S. EJJEBLI, A. ALTIMIMI, S. ABOULMAJD, J. JABBOURI, M. HABOUB, R. HABBAL, (2025) “Rectal Adenocarcinoma Associated With A Prosthetic Valve Infective Endocarditis Due To Escherichia Coli: A Rare Case Report.”. journal of clinical cardiology interventions, 5(1). DOI: 10.61148/2836-077X/JCI /052
Copyright: © 2025 S. EJJEBLI. Thisis an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Infective endocarditis (IE) is a severe microbial infection that affects native and prosthetic heart valves, often caused by pathogens like Escherichia coli, which accounts for only 0.5% of cases due to its lack of key virulence traits. While urinary tract infections are a common source of bacteremia leading to IE, this unique case involved a rectal adenocarcinoma as the origin. The report highlights the 12th documented instance of E. coli IE on a prosthetic valve, emphasizing limited guidelines for its management and discussing risk factors to prevent such infections. It features a 54-year-old woman with mitral valve IE seeded from a digestive tract source.
A 54-year-old North African woman with a history of type 2 diabetes and a prosthetic mitral valve was admitted for dyspnea, palpitations, and fever. She had recently been diagnosed with rectal adenocarcinoma. Blood cultures revealed Escherichia coli, leading to a diagnosis of prosthetic valve infective endocarditis. The patient received intravenous antibiotics and showed initial improvement but later experienced a recurrence of endocarditis and complications, ultimately resulting in her death
Prosthetic valve endocarditis is an uncommon yet serious manifestation of infective endocarditis that demands timely and precise diagnosis. Individuals with ongoing or recurrent E. coli bacteremia, particularly those with underlying risk factors like prosthetic valves, diabetes, or recent invasive interventions, are more susceptible. Early use of transesophageal echocardiography and targeted antibiotic therapy are key to management, although the overall prognosis remains cautious.
infective endocarditis; escherechia coli; prosthetic mitral valve; recal adenocarcinoma
Introduction:
Infective endocarditis (IE) is a microbial infection that primarily involves the heart valves and, less commonly, the mural endocardium. It can affect both native and prosthetic valves, including mechanical and bioprosthetic types and it can be caused by various pathogens.
Escherichia coli, a gram-negative bacillus belonging to the Enterobacteriaceae family, is a rare cause of IE, accounting for approximately 0.5% of cases according to data from a large international study. Its low incidence is largely due to the absence of key virulence traits typically linked to endocardial infections. [1]
While infective endocarditis can arise from various sources of initial infection, the urinary tract is often identified as the origin of bacteremia that seeds the heart valves. However, our case is unique in that the infection originated from the digestive tract, as the patient was diagnosed with rectal adenocarcinoma.
This case study represents the 12th reported instance of this uncommon condition. Our objective is to emphasize the limited data and guidelines available for managing E. coli endocarditis on prosthetic valves, share our clinical experience, and discuss risk factors highlighted in the literature that warrant attention to prevent such infections.
In this report we present a unique case of E.coli prosthetic mitral valve endocarditis in a 54-year-old woman seeded from a rectal source.
Observation:
We report the case of a 54 years old north African female who visited the emergency department accompanied by her family, with a medical history of type 2 diabetes treated with insulin, a mitral valve replacement with a prosthetic valve for a severe mitral stenosis 6 years ago, and rectal adenocarcinoma diagnosed 1 month before her hospitalization.
The patient was admitted in the cardiology department for significant dyspnea and palpitations associated to rectal bleeding and episodic fever (39 ◦C) for the last 2 weeks. The medical examination revealed a conscious patient with a generalized pallor, blood pressure of 100/ 64 mmHg, heart rate of 120 bpm, temperature of 38.5 C, respiratory rate of 21 cpm, and oxygen saturation of 97% on room air. The cardiovascular examination found a grade IV/VI diastolic murmurs, no Janeway lesions or Osler nodes were found.
Complete blood count found an anemia with a hemoglobin rate at 7.2g/dl, white blood cell count (WBC) at 18,000/ml, C-reactive protein (CRP) elevated at 253 mg/dl, Procalcitonin at 1, creatinine (Cr) 9.9 mg/dl; a positive rheumatoid factor. Series of blood cultures were performed before starting antibiotic therapy, with a positive culture for Escherichia coli.
The EKG showed an atrial fibrillation at 120bpm with no anginal symptoms. Transthoracic echocardiography (TTE) showed a mitral prothetic valve with an elevated gradient at 18mmHg, ITVm/ITVao at 2.8, Vmax at 2.5m/s (Fig. 1), dilated left atrium, Pulmonary hypertension a 63mmHg, right ventricule dysfunction. The left ventricular size was within normal limits and the left ventricular ejection fraction was 55%.
We completed examinations with a cine radiograph that showed a partial blocking of the posterior leaflet of the prothetic valve(Fig 2). The transesophageal echocardiogram (TEE) showed a blocked leaflet of the prosthetic mitral valve with the presence of a vegetation image near the blocked leaflet measuring 10*10mm (fig 3 and 4).
A PET scan showed prosthetic and peri-prosthetic hypermetabolism, suggestive of active endocarditis. A cranial and Thoracoabdominal pelvic scan were realized and revealed cardiomegaly and a bilateral mild pleural effusion, Rectal tumor classified as T3bN1Mx.
Considering the results of imaging studies, clinical findings and blood tests, a diagnosis of prosthetic mitral valve infective endocarditis due to Escherichia coli was established. The patient received intravenous antibiotic therapy consisting of ceftriaxone and gentamycin for 6 weeks. Throughout the patient’s hospitalization she received a transfusion of 2 blood bags because of his severe anemia with a control of hemoglobin at 10.5g/dl.
The progression was marked by clinical, biological, and echocardiographic improvement, and she was discharged on Cefixime due to the persistence of a small vegetation with regular echocardiographic follow-up. The evolution was marked by poor tolerance to radiotherapy indicated for her adenocarcinoma, a recurrence of endocarditis with peripheral emboli, then arterial ischemia of the lower limbs, and the patient died in the intensive care unit.
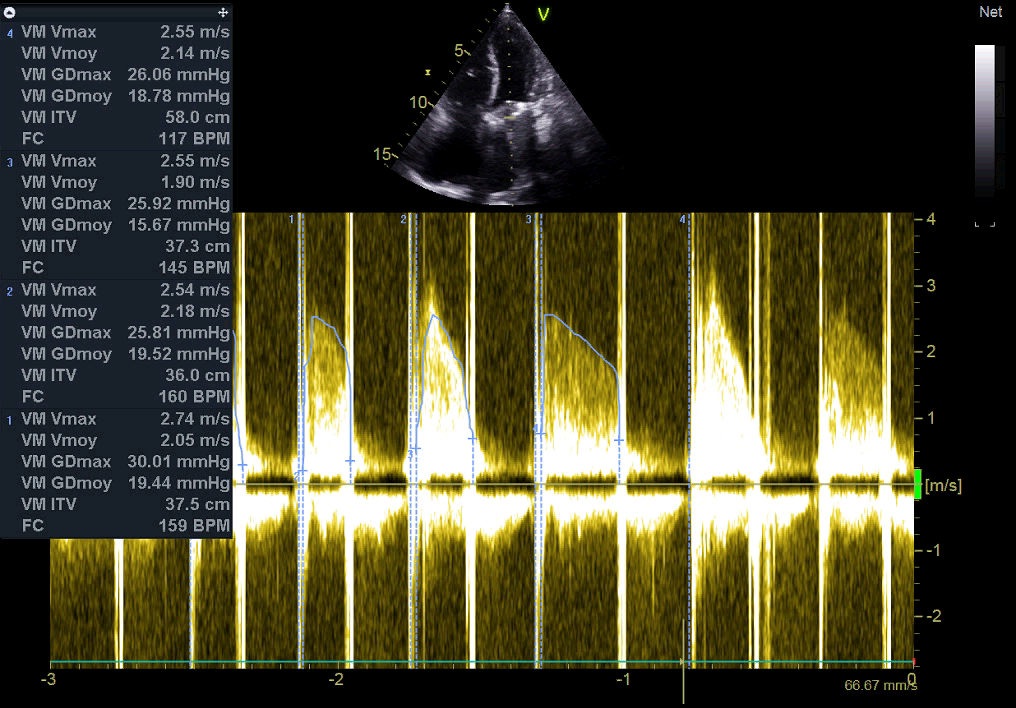
Figure 1: Echocadiography: continuous Doppler on the prothetic mitral valve showing an elevated gradient.
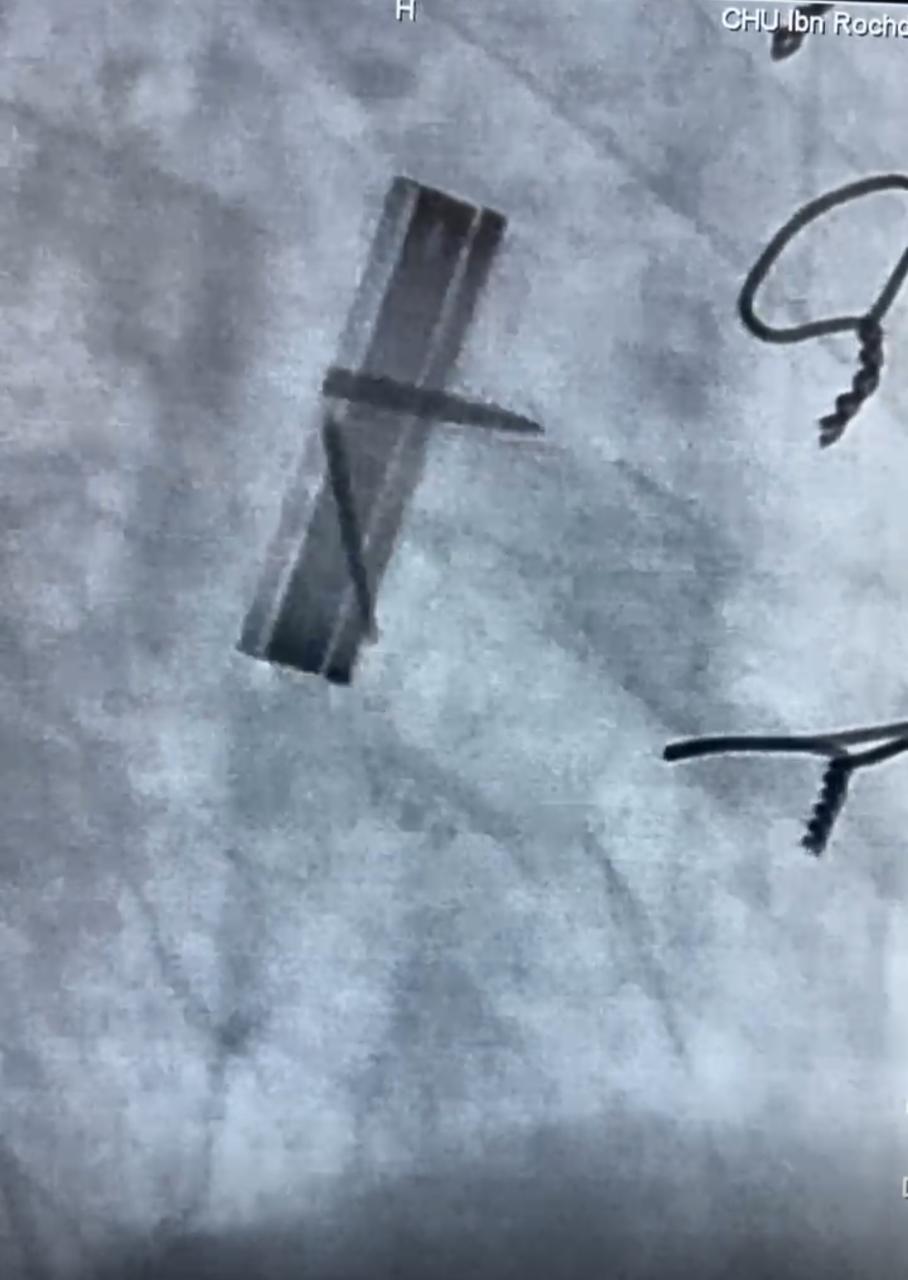
Figure 2: cine radiograph showing a blocking of the posterior leaflet of the prothetic valve
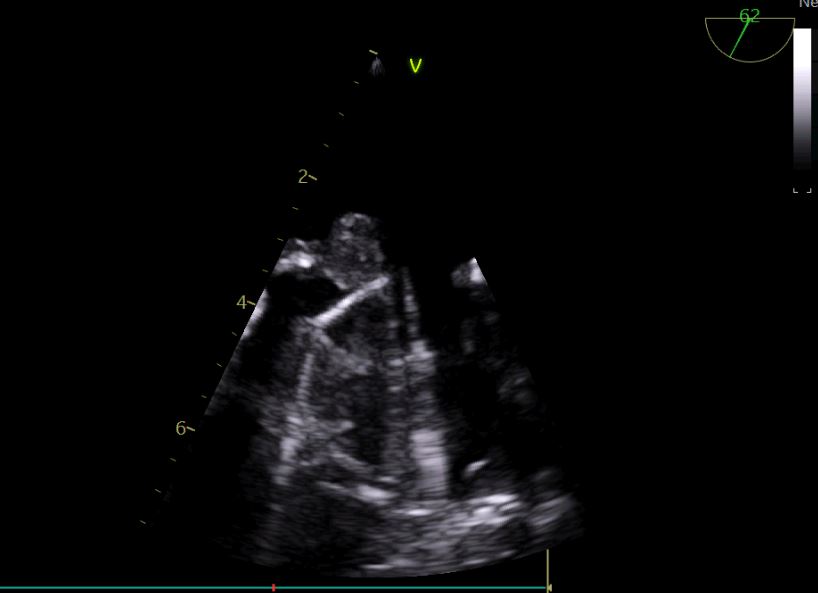
Figure 3: Transoesophageal echocardiography showing the vegetation blocking the leaflet
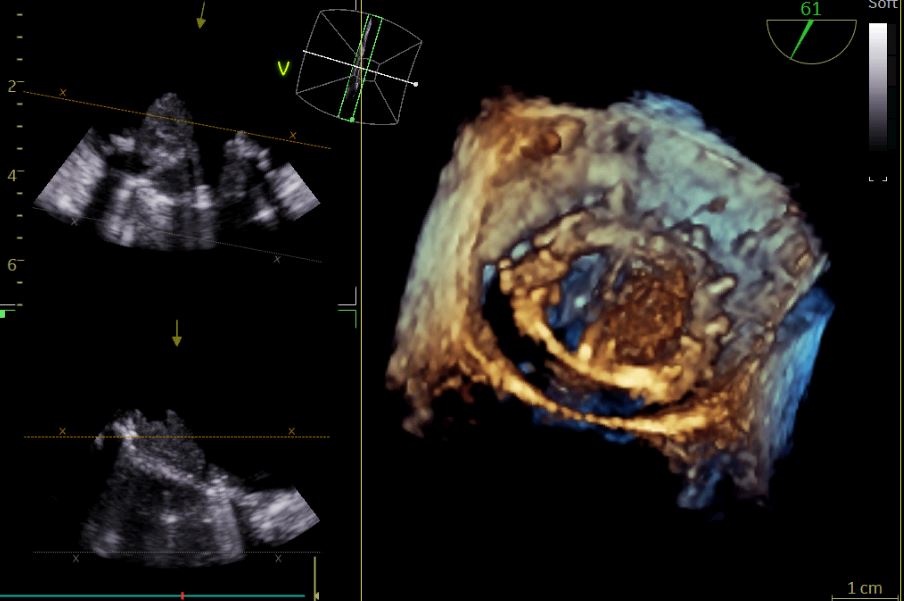
Figure 4: Transoesophageal echocardiography showing the vegetation blocking the leaflet in 3D
Discussion:
Prosthetic valve endocarditis (PVE) is an infrequent yet life-threatening complication following valve replacement, contributing to approximately 10–30% of all cases of infective endocarditis (IE). Its estimated incidence ranges from 0.3 to 1.2% per patient annually. [1]
Although improvements in diagnostic methods, antimicrobial therapy, and surgical approaches have significantly lowered the mortality rate—from 60% to around 30% over the last 20 years— the prognosis remains guarded. [1]
A large international study, involving 2,761 patients diagnosed with definite IE across 61 centers, identified non-HACEK gram-negative bacilli as the causative organisms in 1.8% of cases (49 patients). Among these, Escherichia coli was implicated in 14 cases (29%). Mortality during hospitalization was notably higher in the non-HACEK group (24%) compared to those with HACEK organisms (4%). [2] Over the past 40 years, only 34 cases of E. coli-related IE have been documented in the PubMed database, and among them, just 11 were linked to prosthetic valve infections. [3]
The rarity of E. coli as a causative agent in IE is attributed to its limited ability to adhere to the endocardial surface, necessitating a high bacterial load to establish infection. Risk factors known to predispose individuals to this form of endocarditis include advanced age (over 70 years), female gender, diabetes, immunocompromised states, urinary tract infections, and the presence of intracardiac devices. [2] Among the 11 prosthetic valve-related cases, the mitral valve was involved in the majority (60%).
Our patient presented with multiple risk factors predisposing her to E. coli infective endocarditis (IE), including a mechanical mitral valve, female gender, poorly controlled diabetes, recent hospital stay, and a recent colonoscopy performed in the context of rectal adenocarcinoma.
When evaluating patients with suspected prosthetic valve (PV) endocarditis, transesophageal echocardiography (TEE) is the preferred imaging modality, given its superior sensitivity over transthoracic echocardiography (TTE) in identifying vegetations and associated complications such as abscess formation. [1] TTE, particularly in the context of a prosthetic valve, lacks sufficient sensitivity to confidently exclude IE. [1] This diagnostic distinction was illustrated in our case, where the initial TTE failed to detect vegetations, while subsequent TEE revealed a mitral valve vegetation.
Management of PV endocarditis caused by non-HACEK gram-negative bacilli remains challenging, as there is limited evidence to guide optimal treatment strategies. Current guidelines from the American Heart Association (AHA) [4] recommend a six-week course of combination therapy—typically a β-lactam plus either an aminoglycoside or a fluoroquinolone—for native valve IE caused by these organisms. However, no specific recommendations exist for prosthetic valve involvement.
Morpeth et al. [3] observed similar mortality rates (~25%) in patients who received surgical treatment and those managed medically, indicating that surgery may not be obligatory in all cases of non-HACEK gram-negative IE. In alignment with AHA suggestions for native valve infections, our patient was treated with Ceftriaxone and Gentamicin, resulting in clinical stabilization and a decrease in vegetation size. Unfortunately, the medium-term outcome was unfavorable, with a relapse of endocarditis ultimately leading to the patient’s death—consistent with the high mortality associated with this condition.
Conclusion:
Prosthetic valve endocarditis is a rare but severe form of infective endocarditis that requires early and accurate diagnosis to improve outcomes. Patients with persistent or recurrent E. coli bacteremia, especially those with risk factors such as prosthetic valves, diabetes, or recent invasive procedures, are at increased risk and should be carefully evaluated. Prompt use of TEE and initiation of appropriate antimicrobial therapy are essential for effective management, though prognosis remains guarded.
Declarations
Consent for publication: Written informed consent was obtained from the patients for publication of this case report and any accompanying images.
Availability of data and material: All data generated or analysed during this study are included in this published article.
Competing interests: The authors declare that they have no competing interests.
Author contributions EJJEBLI S.: writing paper AL TIMIMI A : study concept literature ABOULMAJD S.and JABBOURI J.: care of the patient. Habbal R: Interpretation and analysis.
Abbreviations:
IE: Infective endocarditis
TTE: transthoracic echocardiography
TEE: transesophageal echocardiography
HACEK : Haemophilus species; Aggregatibacter species (formerly Actinobacillus) ; Cardiobacterium hominis ;Eikenella corrodens ; Kingella species
AHA: American Heart Association
PVE: Prosthetic valve endocarditis