Pediatrics and Child Health Issues
OPEN ACCESS | Volume 4 - Issue 1 - 2025
ISSN No: 2836-2802 | Journal DOI: 10.61148/2836-2802/JPCHI
Nigusu Derese 1*, Kemal Ahmed 2, Edao Tesa 2, Tariku Derese 3
1 Senior Expert in reproductive health at West Guji zone, Zonal Health Departement,in Oromia regional state, Hagermariam, Ethiopia.
2Assistance professor and Lecturer at Madda Walabu University, Shashemene Campus, School of Health Science, Department of Public Health,Ethiopia
3Lecturer at Dire Dawa University, Department of Midwifery, College of Medicine and health Science, Ethiopia
*Corresponding author: Nigusu Derese, Senior Expert in Reproductive health at West Guji zone, Zonal Health Departement, Oromia regional state, Hagermariam, Ethiopia.
Received date: November 18, 2020
Accepted date: November 20, 2020
Published date: November 25, 2020
Citation: Derese N, Ahmed K, Tesa E, Derese T. “Essential Newborn Care Practice and Associated Factors Among Home Delivered Mothers within the Past Six Months, in Abaya District, West Guji Zone, Oromia Regional State, Ethiopia, 2019.’’. J of Pediatrics and Child Health Issues, 1(1); DOI: http;//doi.org/03.2020/1.1002.
Copyright: © 2020 Nigusu Derese. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Background: Poor immediate new-born care practice increases risk of morbidity and mortality by predisposing the new-borns to sepsis and hypothermia. In developing countries nearly 3 million new-borns babies die every year mostly where many births happen at home. Therefore, assessment of essential new-born care practice among home delivered mothers is important for the improvement of new born health and reduction of risk of morbidity and mortality. However, to the best knowledge of researcher, there was no previous study on this title at this study area.
Objective: Assess essential new-born care practices and associated factors among mothers delivered at home during the six months preceding the study in Abaya district of West Guji zone, Oromia, Ethiopia from August 1-30, 2019.
Methods: Community based cross-sectional study design was employed. Stratified-multi stage sampling technique was used to select 632 study subjects. Structured pretested questionnaire was used for data collection. After one day training given six diploma and 2 BSc nurses were participated as data collectors and supervisors respectively. After data clearance and coding done data entered in to Epi-info version 7 and exported to SPSS window version 21.0 for analysis. Binary and multiple logistic regression analysis were used to identify factors associated with outcome variable .Adjusted odd ratio with their 95% CI were calculated to determine the presence and strength of association. P-value of <0.05, considered to declare significance.
Result: The overall level of good new-born care practice in this study was 18.9%(95% CI:0.16; 0.22).Urban residence (AOR: 2.233; 95% CI: 1.082, 4.607),No PNC visit (AOR:0.618; 95% CI:0.400,0.954), Home delivery assisted by HEW (AOR:3.617;95% CI:1.058,4.607),Home delivery assisted by relatives(AOR:0.427;95%CI:0.222,0.821),Last ANC visit at health post (AOR:0.485; 95% CI:0.299,0.785), didn’t knowing poor sucking as danger sign (AOR:0.524;95% CI:0.332,0.826) were independent factors associated with Essential New-born care practice.
Conclusion: The level of essential new-born care practice (ENBCP) found in this study was very low compared to studies conducted previously in different areas. No PNC home visit by HEW, having last ANC visit at health post, didn’t knowing poor sucking as danger sign and home delivery assisted by relatives were factors negatively associated with ENBCP and urban residence and home delivery assisted by HEW were factors positively associated with Essential new-born care practice.
Introduction
Abbreviations: ANC: Antenatal Care, AOR: Adjusted Odd Ratio, BF: Breast Feeding, BSC: Bachelor Science, CI: Confidence Interval, CHW: Community Health Worker, CSA: Central Static Agency, COR: Crude Odd Ratio, EDHS: Ethiopia Demography and Health Survey, ENCP: Essential New-born Care Practice, ETB: Ethiopian Birr, HEW: Health Extension Worker, MNCH: Maternal Neonatal and Child Health, NMR: Neonatal Mortality Ratio, OR: Odd Ratio, PNC: Postnatal Care, SBA: Skill Birth Attendant, SDG: Sustainable Development Goal, SRS: Simple Random Sampling, SNNP: South Nation Nationality of People, TBA: Traditional Birth Attendant, TTI: Tetanus Toxoid Injection, UN: United Nation, UNICEF: United Nation International Children Emergency Fund, WHO: World Health Organization
Background
The essential new-born care practice (ENBCP): refers to a set of practices that reduces neonatal morbidity and mortality such as safe cord care practice, thermal care practice and initiating breastfeeding within the first hour(WHO, 2017, KUMOLA, 2015). ENBC is a care that every new-born baby needs regardless of where it is born or its size. It should be applied immediately after the baby is born and continued for at least the first 7 days after birth (Thenmozhi and Saraswathi, 2017).
Neonatal death in the first month of life mainly concentrated in the first days of life which are mostly preventable and could be avert by providing care around the time of birth by applying key essential new-born care practices that should be applied starting immediately after birth (UNICEF, 2019). Poor new-born care practices immediately following delivery contribute to the risk of morbidity and mortality of the new-born by predisposing to sepsis and hypothermia (Afolabi, 2017).
Globally women’s and children’s health is a smart investment, particularly care given at birth. The global society had sets a goals by SDG (sustainable development goal) that targeted to achieve at the end of 2030, end preventable new-borns death, with all countries aiming to reduce neonatal mortality to at least as low as 12 per 1000 live births(UN, 2015). With high coverage of care around the time of birth and the care of small and sick new-borns would safe nearly 3 million lives of new-borns each year at an additional running cost of only US$ 1.15 per person in 75 high burden countries. This would have a triple impact on investments: saving women, new-borns and preventing stillbirths (WHO, 2015, Thenmozhi and Saraswathi, 2017). However, in 2018 an estimated 2.5 million new-borns died in the first month of life. Most of these new-borns died in the first week of life with approximately one million died in the first day and another one million died in the following six days (UNICEF, 2019). The high mortality and morbidity rates among new-borns are related to inappropriate community practices that currently occur throughout the region at home delivered mothers (WHO, 2014). In developing countries nearly three million new-born babies die every year mostly where many births happen at home and 98% of the global neonatal death occurs in these areas (Children, 2017).
In sub-Saharan Africa, 50% of neonatal deaths occur in just five countries(Nigeria, DR Congo, Ethiopia, Tanzania and Uganda)(Afolabi, 2017) and up to 67 per cent of sub-Saharan Africa’s new-born deaths could be prevented with high coverage of care, with simple home behaviour’s including birth preparedness, breastfeeding, keeping the baby warm, and safe cord care practice and also neonatal mortality can be decreased (19-34%) by care given at child birth and (10-27%) care given at postnatal period (Graft-Johnson et al., 2015).
In Ethiopia as the recent mini- EDHS 2019 report showed , even if the infant mortality rate was decreased from 48 to 43 deaths per 1,000 live births, neonatal mortality increased 29/1000 to 30/1000 ([Ethiopia] and ICF, 2019). Due to lack of information how to care herself and her baby immediately after birth a large proportion of maternal and neonatal death occur within the first 48 hours of post-delivery ([Ethiopia] and ICF, 2019)
Even if improving new-born health outcomes in Ethiopia will likely require a multifaceted approach and the government of Ethiopia strived to this by designing different intervention, but not great attention was given to those mothers delivered at home how they practiced essential new-born care practices (Callaghan-Koru1 et al., 2013).
Therefore this study aimed to assess the level of essential new-born care practice and associated factors among home delivered mothers which help to the survival of neonate at communities’ level by providing locally generated evidence.
Methods
Study Area and Period
The study was conducted in Abaya district, one of the 10 districts of west Guji zone in Oromia region. It is located 465 KM away from Addis Ababa, capital city of Ethiopia to Southern. The district has six health centres and 30 health posts .There are 69 Health extension workers, 7 midwifes and 40 other health workers totally 126 health workers .The district also has 26 rural and four urban kebeles. As district evidence showed according to CSA (2019) population projection, the district has 142,368 populations. Data were collected from August 1– 30, 2019.
Study Design
A community based cross-sectional study design was employed.
Inclusion and Exclusion Criteria
Inclusion criteria All women who gave live birth at home in the past six months prior to the study period and who lived at least for six months in the selected kebeles of Abaya district.
Exclusion Criteria
Those mothers who had not mental ilness and seriously ill and unable to respond during the data collection period were excluded.
Operational definitions
Essential new born care practices: Set of practices given by mothers to new-borns which include safe cord care practice, thermal care practice and early initiating breast feeding within the first hour of birth (WAKUMA, 2017, Mersha et al., 2018).
Good new-born care practices: Mothers who reported practicing thermal care, safe cord care and early initiation of breast feeding were considered as having good essential new-born care practice. (WAKUMA, 2017, Mersha et al., 2018).
Poor new-born practice: Mothers who reported practicing of two or less practices mentioned above were considered as having poor essential new-born care practice (WAKUMA, 2017, Mersha et al., 2018).
Early initiation of breast feeding: Mothers initiating breast feeding to new-born baby following delivery within one hour of life (WHO, 2017).
Safe cord care: Using clean instrument to cut umbilical cord, keeping the cord clean and dry without application of any foreign substances until the umbilical stump falls off (Berhe et al., 2016).
Thermal care: Avoidance of bathing before 24 hrs of delivery and well wrapping of neonates with new or clean cloth and early skin to skin contact (WHO, 2017).
Good knowledge on new-born care practice: Those mothers who responded correctly above 50% of knowledge related questions (WAKUMA, 2017, Mersha et al., 2018).
Poor knowledge on new-born care practice: Those mothers who responded correctly less or equal to 50% of knowledge related questions (WAKUMA, 2017, Mersha et al., 2018)
Good knowledge on neonatal danger sign: Mothers who mentioned >=4 neonatal danger signs (WAKUMA, 2017, Mersha et al., 2018)
Poor knowledge on neonatal danger sign: Mothers who mentioned less than 4 of danger signs (WAKUMA, 2017, Mersha et al., 2018
Data Collection Tool
The data were collected using pre-tested, structured interview administered questionnaires through face to face interview. The tool was adapted from previous literature and EDHS (WAKUMA, 2017, Ethiopia, 2016) and arranged in such a way that included all relevant variables to meet the objectives of the study. The questionnaire was first written in English language then it was translated to Afan Oromo language for better understanding for both data collectors and respondents. To keep consistency the questionnaire was translated back to English language by another individual who speak both languages. Finally the Afan Oromo version was used for data collection.
Data Quality control
Six data collectors and two supervisors who were fluent speaker of Afan Oromo language and worked in the same district were selected and trained for one day on procedures of data collection techniques, approaching participants, ethical issues, quality of data and advantage of collecting the actual data as well as the role and responsibilities they had as data collectors and supervisors. The pre-test was done by data collectors on 5% of the total sample size outside of the study selected kebeles (odo mike and kelaltu) which have the same socio-demographic characteristics with selected kebeles. During pre-test lack of clarity, on some words was faced and modification was done accordingly before the actual data collection period. Onsite supervision was carried out during the whole period of data collection in daily basis. At the end of each day, questionnaires was reviewed and cross checked for their completeness, accuracy and consistency by the supervisor and investigator, in case error faced corrective measures was taken and remark was given in the next morning before data collection started to data collectors. After the data collected data clearance and coding done by investigator and careful data entry was employed by the investigator to control data quality.
Data collection procedure
Prior to interview, informed consent was obtained from respondents after thoroughly communicated about the objective of study. Data were collected by six diploma Nurses with house to house visit through face to face interview and were supervised daily by two BSc Nurses. When mothers were not at home on the first home visit, two additional visits were made before considering as non-response. The supervisors was responsible for supporting the data collectors, checking filled out questionnaires daily for completeness and logical consistence then provided feedback for data collectors. The investigator also participated in the supervision of the data collection and daily feedback on gaps identified.
Data processing and Analysis
After the data was checked for error, completeness and accuracy by investigator, it was coded and entered using EPI Info version 7 and exported to SPSS version 21.0 software packages for analysis. Variables with p–value ≤ 0.25 on binary logistic analysis were considered for fitting to multiple logistic regression analysis to determine the effect of various factors on the outcome variable and to control confounding effect. Hosmer-lemesho goodness-of-fit done and was found to be insignificant (p=0.725) and Omnibus test of model was found to be significant (0.000) which indicate that the model was fitted. The multi-co linearity also checked by using Variance inflation factors (VIF) and VIF>10 were checked to drop from multi variable logistic regression. The presence of association between the independent and dependent variables was reported using adjusted odds ratio with 95% confidence interval and p-value < 0.05 were considered to declared significance level. The results were presented in the form of tables, figures and text using frequency and summary statistics such as, percentage.
Result
Socio demographic characteristics of the respondents
A total of 620 mothers who gave birth at home within the last six months participated in the study. The response rate was 620(98.1%). The median ages of the respondents were 27 year. From the respondents 482(77.7%) were protestant by religion, 562 (90.6%) of them were Oromo by ethnicity and 96 %( 595) of them were married. Majority of the respondents have no formal education 436(70.3%) and 496(80%) of them were house wife by occupation. About 569(91.8%) of respondents were rural residents and 314(50.6%) of the respondents have monthly income below 500 Ethiopian Birr (Table 1).
|
Variables n=620 |
Frequency |
Per cent |
|
|
Mothers age |
|
|
|
|
15-24 |
181 |
29.2 |
|
|
25-35 |
403 |
65 |
|
|
36-49 |
36 |
5.8 |
|
|
Religion |
|
|
|
|
Protestant |
482 |
77.7 |
|
|
Orthodox |
92 |
14.8 |
|
|
Others |
46 |
7.4 |
|
|
Ethnicity |
|
|
|
|
Oromo |
562 |
90.8 |
|
|
Others |
57 |
9.2 |
|
|
Marital status |
|
|
|
|
Married |
595 |
96 |
|
|
Not married |
11 |
1.8 |
|
|
Others |
14 |
2.2 |
|
|
Educational level |
|
|
|
|
No formal education |
436 |
70.3 |
|
|
Primary |
164 |
26.5 |
|
|
Secondary and above |
20 |
3.2 |
|
|
Residence |
|
|
|
|
Urban |
51 |
8.2 |
|
|
Rural |
569 |
91.8 |
|
|
Monthly income |
|
|
|
|
<500 |
314 |
50.6 |
|
|
500-999 |
274 |
44.2 |
|
|
>=1000 |
32 |
5.2 |
|
Table 1: Socio demographic characteristics of mothers who gave birth at home within the last six months in Abaya district, Oromia, Ethiopia, 2019.
Maternal health service and obstetric information of the respondents
About 273(44%) of the respondents reported that, they received education and advice on essential new-born care practices from HEWs through home visit. From respondents 411(66.3%) have at list one ANC visit and 329(53.1%) of mothers started ANC after four months of gestational age of which 362(58.4%) of them counselled about new-born care. More than half 366(59%) of the respondents attended ANC services at health posts. Majority of the respondents 472(76.1%) were delivered their first babies between the age of 15-19 years and 86(13.9%) of them have history of neonatal loss. From all respondents 270(45%) and 198(32%) were assisted during home delivered by relatives and traditional birth attendants respectively (Table 2a, 2b).
|
Variables(n=620) |
Frequency |
Percent |
|
HEW home visit |
|
|
|
No |
347 |
56 |
|
Yes |
273 |
44 |
|
Neonatal death history |
|
|
|
No |
534 |
86.1 |
|
Yes |
86 |
13.9 |
|
Children alive |
|
|
|
>=4 |
328 |
52.9 |
|
2-3 |
181 |
29.2 |
|
1 |
111 |
17.9 |
|
ANC follow up |
|
|
|
No |
209 |
33.7 |
|
Yes |
411 |
66.3 |
|
Number of ANC visit |
|
|
|
1 |
78 |
12.6 |
|
2=3 |
314 |
77.9 |
|
>=4 |
59 |
9.5 |
|
Place of ANC visit |
|
|
|
Health Center |
251 |
40.5 |
|
Health post |
336 |
59.5 |
|
Gestational age of first visit |
|
|
|
<=4 month |
291 |
46.9 |
|
>4 month |
329 |
53.1 |
|
Attending monthly pregnant mother meeting |
|
|
|
No |
398 |
64.2 |
|
Yes |
222 |
35.8 |
Table 2a: Maternal health service and obstetric information of mothers who gave birth at home within the last six months in Abaya district, Oromia, Ethiopia, 2019
|
Variables(n=620) |
|
|
|
Counseling during ANC visit at least once on |
|
|
|
Breast feeding within 1 hour |
Frequency |
Percent |
|
No |
258 |
41.6 |
|
Yes |
362 |
58.4 |
|
Skin to skin contact for 24 first hour |
|
|
|
No |
278 |
44.8 |
|
Yes |
342 |
52.2 |
|
Delany bathing >24hr |
|
|
|
No |
268 |
43.2 |
|
Yes |
352 |
56.8 |
|
Keep cord care clean & safe |
|
|
|
No |
237 |
38.2 |
|
Yes |
383 |
61.8 |
|
Care for LBW |
|
|
|
No |
342 |
55.2 |
|
Yes Current child sex |
238 |
44.8 |
|
Female |
322 |
51.9 |
|
Male |
292 |
47.1 |
|
Child age |
|
|
|
<1month |
39 |
6.3 |
|
1-6moths |
581 |
93.7 |
|
HEW visit during PNC |
|
|
|
No |
377 |
60.8 |
|
Yes |
243 |
39.2 |
Table 2b: Maternal health service and obstetric information of mothers who gave birth at home within the last six months in Abaya district,Oromia ,Ethiopia ,2019
Health education and advice given by HEW during home visit on essential new-born care related practice.
Health education and advice given by HEW during home visit on essential new-born care related practice. About 67% of respondents were educated about neonatal danger sign that need immediate health care (Figure 1)
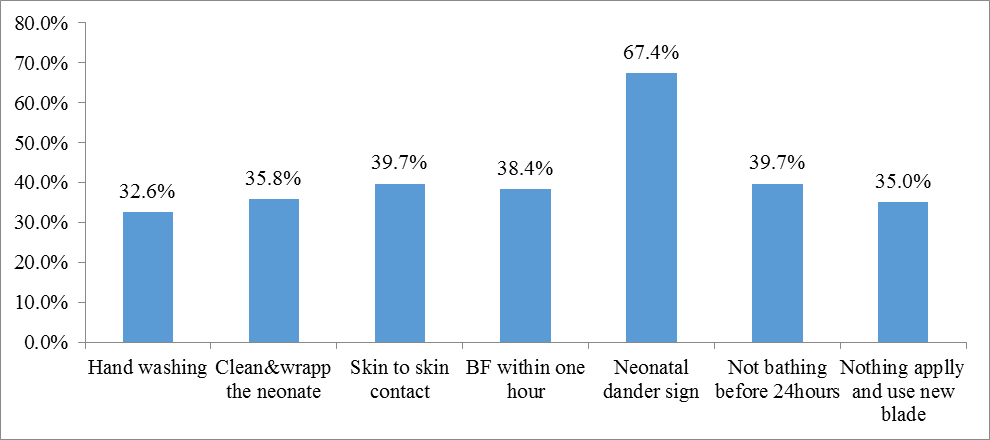 Figure 1: Health education and advice given by HEW during home visit for those mothers who gave birth at home within the last six months in Abaya district, Oromia , Ethiopia, 2019.
Figure 1: Health education and advice given by HEW during home visit for those mothers who gave birth at home within the last six months in Abaya district, Oromia , Ethiopia, 2019.
Prevalence of new-born care practice
The overall prevalence of good new-born care practice of mothers who had less than six months in Abaya District was 117(18.9%) The prevalence of each of variables: Early breast feeding initiation 161(26%), safe cord care practice 179(28.9%) and thermal care was 191(30.8%) respectively (Figure 2).
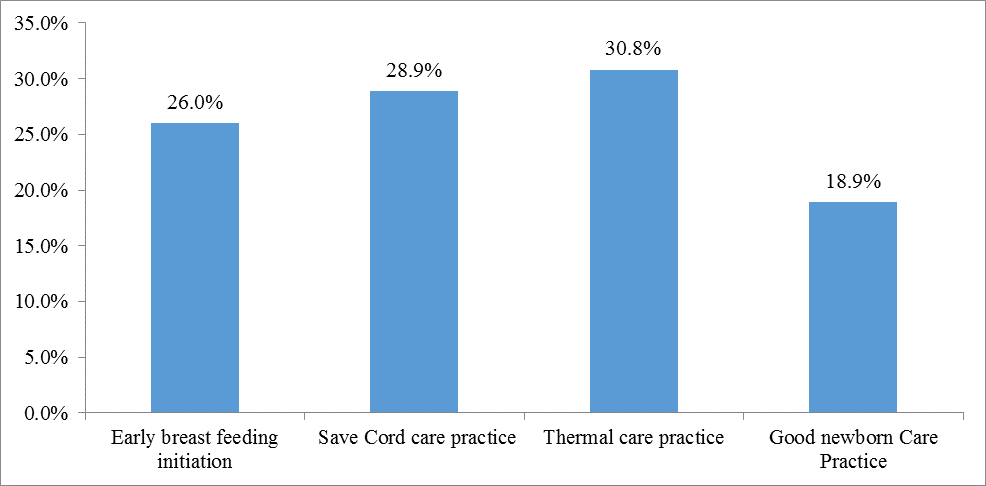
Figure 2: Prevalence of new-born care practice by composite variables for mothers who gave birth at home within the last six months in Abaya District, Oromia , Ethiopia, 2019.
Early initiation of breast feeding practice of respondents
From all the respondents 570(91.9%) of mothers gave first milk/colostrum to their babies. But only 161(26%) of them started early breast feeding initiation within the first hours after delivery and 370(59.7%) of mothers breast fed exclusively. Respondents started to give additional food were 250(40.3%) and majority of them gave cow milk 399(64.4%) and 75(12.1%) use bottle feeding because of advice given from their family33 (5.3%) (Table 3
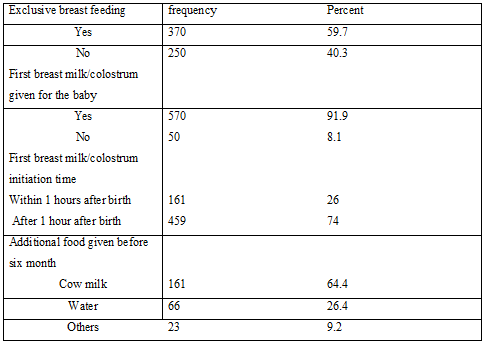
Table 3: Breast feeding practice of respondents who gave birth at home within the last six months in Abaya District, Oromia, Ethiopia, 2019.
Safe cord care practice of respondents
Almost all respondents 532(85.8%) used material to cut cord were new or boiled blade and 524(84.5%) of them used new tread to ties the cord after cut. Most mothers 414(66.8%) nothing applied on the cord but, 206(33.2%) of respondents applied substances commonly butter 412(66.4%) (Table 4).
Table 4: Safe cord care Practice of respondents who gave birth at home within the last six months in Abaya District, Oromia , Ethiopia ,2019.
|
Material used to cut cord |
|
|
|
Used new or boiled blade |
530 |
85.5 |
|
Used not boiled blade |
90 |
14.2 |
|
What applied after cut |
|
|
|
Substance applied |
414 |
66.8 |
|
Nothing applied |
206 |
33.2 |
|
Article used to tie cord |
|
|
|
New tread |
592 |
84.5 |
|
Tread |
83 |
13.4 |
|
Plant fiber |
13 |
2.1 |
|
What substance applied on the cord |
|
|
|
Butter |
152 |
24.4 |
|
Others |
55 |
8.8 |
|
What did you do if baby cord bleed /unpleasant discharge |
|
|
|
Go to health center |
|
|
|
No |
83 |
13.4 |
|
Yes |
537 |
86.6 |
|
Home medication |
|
|
|
No |
480 |
77.4 |
|
Yes |
140 |
22.6 |
|
Wait until heal |
|
|
|
No |
556 |
89.7 |
|
Yes |
64 |
10.3 |
|
Others |
|
|
|
No |
600 |
96.8 |
|
Yes |
20 |
3.2 |
Thermal care practice of respondents
Among total respondents, only 218(35.2%) delayed 24 hours to bath the baby according to the standards. Mothers had practiced skin to skin contact with their babies were 251(40.5%). Those had skin to skin contacts were placed on mothers abdomen and chest accounts 231(37.2%) and 249(40.2%) of the babies dry and wrapped with new or clean closes. Over all thermal care practiced (delay bathing for 24 hours, skin to skin contact always and wrapped with new or clean close) were found 191(30.8%) (Table5)
|
Time given bathing for the baby after birth |
|
|
|
Within one hours |
192 |
31 |
|
After 24 hours |
218 |
35.2 |
|
Within 24 hours |
180 |
29 |
|
I don’t know |
30 |
4.8 |
|
Skin to skin contact within 24 hours of birth |
|
|
|
Not at all |
91 |
14.7 |
|
Upto2hours |
263 |
42.3 |
|
2-24hr |
40 |
6.4 |
|
Always |
251 |
40.5 |
|
On what part of mothers |
|
|
|
Abdomen or chest |
231 |
37.2 |
|
Others |
108 |
62.8 |
|
Did baby dry and wrapped by |
|
|
|
Clean or new close |
|
|
|
No |
371 |
60.8 |
|
Yes |
249 |
40.2 |
|
|
|
|
Table 5: Thermal care practice of respondents who gave birth at home within the last six months in Abaya district, Oromia, Ethiopia, 2019.
Knowledge of respondents on new-born care practices and neonatal danger signs
The respondents asked new-born care practices related questions to assess their knowledge of essential new-born care practices and about 271(43.7%) of them answered above fifteen per cent (>50%). Again respondents asked to mention neonatal danger signs (Poor sucking or not able to feed breast, fast breathing, fever, hypothermia, drowsy or unconscious and cord bleeding and infection) to assess mothers neonatal danger signs knowledge and 283(45.6%) of them mentioned four and above(>=4) (figure 3).
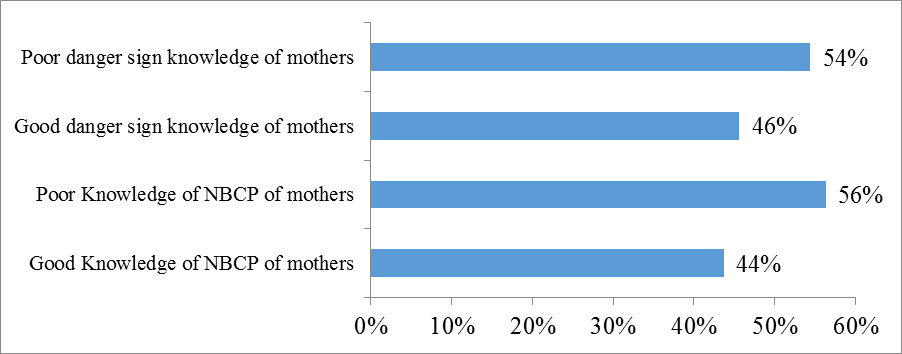
Figure 3: Knowledge level of respondents on new-born care practice and danger sign of new-born for mothers who gave birth at home within the last six months in Abaya district, Oromia, Ethiopia ,2019.
Factors associated with essential new-born care practices
Logistic regression was carried out to examine the associations between each independent variables and the outcome variable. The variables with p-value of <0.25 were taken as candidates for multivariable analysis (Table 6a). Accordingly nine variables which fulfil this criterion were fit in to multivariable model.
Table: 6a Factors associated with ENBCP by bivariate logistic regression analysis for mothers who gave birth at home within the last six months in Abaya district, Oromia, Ethiopia, 2019.
|
Variables |
Good ENBCP |
Poor ENBCP |
COR(95%CI) |
P-value |
|
Residence |
|
|
|
|
|
Urban |
15(12.8%) |
36(7.2%) |
1.908(1.007-3.615) |
0.048* |
|
Rural |
102(87.2%) |
467(92.8%) |
1 |
|
|
Advise during ANC/ early initiation of breast feed visit |
|
|
|
|
|
No |
80(68.4%) |
280(55.7%) |
0.581(0.347-0.891) |
0.013* |
|
Yes |
37(31.6%) |
223((44.3%) |
1 |
|
|
Place of last ANC visit |
|
|
|
|
|
Health post |
83(70.9%) |
283(56.3%) |
1.372(1.103-1.707) |
0.004* |
|
Health center |
34(20%) |
223(43.7%) |
1 |
|
|
Assistant during delivery |
|
|
|
|
|
HEW |
6(5.1%) |
8(1.6%) |
2.872(0.944,8.740) |
0.063 |
|
Neighbors |
54(46.2%) |
223(44.3%) |
0.972(0.589,1.461) |
0.745 |
|
Relatives |
16(13.6%) |
115(22.9%) |
0.533(0.285,0.996) |
0.049* |
|
TBA |
41(35.1%) |
157(31.2%) |
1 |
|
|
Immediate PNC visit |
|
|
|
|
|
No |
58(49.6%) |
319(63.4%) |
0.567(0.378-0.850) |
0.006* |
|
Yes |
59(50.4%) |
184(36.6%) |
1 |
|
|
Knowing cord bleeding or infection as danger sign |
|
|
|
|
|
No |
56(47.9%) |
295(58.6%) |
0.647(0.43-0.969) |
0.035* |
|
Yes |
61(52.1%) |
208(41.4%) |
1 |
|
|
HEW advise about neonate need immediate health care |
|
|
|
|
|
No |
49(41.9%) |
153(30.4%) |
0.607(0.401-0.917 |
0.018* |
|
Yes |
68(58.1%) |
350(69.6%) |
1 |
|
|
Knowing poor sucking as danger sign |
|
|
|
|
|
No |
38(32.5%) |
261(51.9%) |
0.446(0.292-0.682) |
0.001* |
|
Yes |
79(67.5%) |
242(48.1%) |
1 |
|
|
Mothers Knowledge about ENBCP |
|
|
|
|
|
Good |
93(79.5%) |
428(85.1%) |
1.208(1.017-1.434) |
0.031* |
|
Poor |
24(20.5%) |
75(14.9%) |
1 |
|
Multivariable logistic regression analysis was carried out through forward conditional method in multiple logistic regression analysis, Urban residence (AOR: 2.233; 95% CI: 1.082, 4.607, p<0.030),ANC visit at health post (AOR:0.485; 95% CI :0.299,0.785, p<0.003), Home delivery assisted by HEW (AOR:3.617; 95% CI:1.058,4.607, p<0.040), Home delivery assisted by relatives (AOR:0.427; 95% CI :0.222,0.821, p<0.011), No PNC visit (AOR:0.618,;95% CI :0.400,0.954, p<0.030), didn’t knowing poor sucking as neonatal danger sign(AOR:0.524; 95% CI:0.332,0.826, p<0.005) were significantly associated factors (Table 6b).
|
Variables |
ENBCP |
AOR |
(95% CI) |
P-value |
|
|
Residence |
Good ENBCP |
Poor ENBCP |
|
|
|
|
Urban |
15(12.8%) |
36(7.2%) |
2.233 |
1.082-4.607 |
0.030* |
|
Rural |
102(87.2%) |
467(92.8%) |
1 |
|
|
|
Place of ANC visit |
|
|
|
|
|
|
Health post |
83(70.9%) |
283(56.3%) |
0.485 |
0.299-0.785 |
0.003* |
|
Health center |
34(20.1%) |
216(43.7%) |
1 |
|
|
|
Assistant during home delivery |
|
|
|
|
|
|
HEW |
6(5.1%) |
8(1.6%) |
3.617 |
1.058-4.607 |
0.040* |
|
Neighbors |
54(46.2%) |
223(44.3%) |
0.848 |
0.525-1.358 |
0.499 |
|
Relatives |
16(13.6%) |
115(22.9%) |
0.427 |
0.222-0.821 |
0.011* |
|
TBA |
41(35.1%) |
157(31.2%) |
1 |
|
|
|
PNC visit by HEW |
|
|
|
|
|
|
No |
58(49.6%) |
319(63.4%) |
0.618 |
0.400-0.954 |
0.030* |
|
Yes |
59(50.4%) |
184(36.6%) |
1 |
|
|
|
Knowing poor sucking as danger sign |
|
|
|
|
|
|
No |
38(32.5%) |
261(51.9%) |
0.524 |
0.332-0.826 |
0.005* |
|
Yes |
79(67.5%) |
242(48.1%) |
1 |
|
|
Table 6b: Factors associated with the ENBCP variables by multivariate logistic regression analysis for mothers who gave birth at home within the last six months in Abaya district, Oromia, Ethiopia ,2019.
Discussion
In this study the overall level of good essential newborn care practice was 18.9% (95% CI:0.16;0.22) while timely initiation of breast feeding was 26%, thermal care practice was 30.8% and safe cord care practice was 28.9% .The overall level of good essential newborn care practice (ENBCP) of this study 18.9% was lower than study conducted in Indian with good essential newborn care practice of 46.7% (Thenmozhi and Saraswathi, 2017), Nekemte town which was 47% (WAKUMA, 2017), in Hosana town which was 31% (SAKELO, 2018), Aksum town which was 26.7% (Berhe et al., 2016), Metekel zone Mandura district which was 40.6% (Tegene et al., 2015), in Gojam zone Awabel district which was 23.1% (Kokebie et al., 2014), Wolayita zone Damot Pulsa district which was 24% (Chichiabellu et al., 2018) and Tigray ,Gulokoma district which was 92.7%.
The possible reason for this difference might be due to study design employed in Indian, Nekemte town and Aksum town institutional based cross-sectional study design were used and educational status also might be the reason for the deference included with Hosanna town since in this study area 70.3% of respondents has no formal education. The possible reason for the difference with Mandura district, Damot pulas district and Awabel distric might be due to cultural difference, media access and health service coverage’s.
This ENBCP prevalence slightly higher than study done in Keniya Garissa 14% (KUMOLA, 2015) and in Lawra district of Ghana15.8% (Saaka et al., 2018).This might be due to the presence of cultural and life style difference. For instance in Kenya Carissa the study was done in pastoralist areas and there is a believe, camel milk had more energy than breast milk from newly delivered mothers for first feed and in Ghana lawra district giving breast milk first may dry newborn throat. However in this study area around 92% of respondents give first milk or colostrums to their babies.
Timely initiation of breast feeding in this study was very low 161(26%) compared to study conducted in urban Uganda where over half of the mothers initiated breast feeding within the first hour of life(Kayom et al., 2015).The finding also lower than study conducted in Oromia regional state Nekemte town 76.6%(WAKUMA, 2017), Aksum town 63.1% (Berhe et al., 2016), Hosanna town 83.3% (SAKELO, 2018).This difference might be due to better understanding about breast feeding within one hours after delivery in urban areas secondary to educational status, health service coverage and quality as well as media access.
This study finding also lower than study conducted in East Gojam, Awabel district 41.6% (Kokebie et al., 2014), Metekel zone Madura district 45.1% (Tegene et al., 2015), Wolayita zone Damot pulasa district 45.85% (Chichiabellu et al., 2018) and study done in four region of Ethiopia 52.1% (Callaghan-Koru1 et al., 2013). These differences may be due to socio-cultural difference and presence of lower awareness about importance of timely initiation of breast feeding in this study area secondary to respondent’s educational status.
Timely initiation of breast feeding in this study, 26%, was higher than study done in Oromia region Illu Aba bora zone chewaka resettlement 16.8% (Aliye, 2014).This might be due to these resettled community still may not have stable life and poor health infrastructure to access health service to get adequate information about ENBCP.
The level of thermal care practice found in this study 191(30.8%) was lower than study done, Nekemte town 78.7%(WAKUMA, 2017),SNNP regional state wolayita damot pulasa district 65.3%(Chichiabellu et al., 2018),study done in SNNP regional state Hosana town 32.95%)(SAKELO, 2018),Amhara regional state East Gojam Awabel district 34.4% (Kokebie et al., 2014)and Aksum town 32.6%(Berhe et al., 2016).The possible reason for this might be presence of cultural difference . In this study area there is a cultural believes bathing newborn early considered as removing dirty from it. But thermal care practice found in this study was higher than study conducted in four region of Ethiopia (Oromia,Amhara,SNNP and Tigry)25.3%(Callaghan-Koru1 et al., 2013) and this might be related with study design employed and time difference between the study period. This study result also higher than study done in Oromia region Illu Aba bora zone Chewaka resettlement 16%(Aliye, 2014) it might be due to instability of this resettled community , health service coverage and awareness difference between respondents .
The prevalence of safe cord care practice 28.9% in this study found was lower than studies conducted in study done in Gojam Awabel district 97.6%(Kokebie et al., 2014) and SNNP Wolayita Damot pawulas district 96.4% (Chichiabellu et al., 2018) Nekemte town 76.7%
(WAKUMA, 2017), Metekel Zone Madura district 59.8%(Tegene et al., 2015), Hosana town 32.9%(SAKELO, 2018), Aksum town 42.96%(Berhe et al., 2016) and with the studies conducted in four region of Ethiopia 88.3%(Callaghan-Koru1 et al., 2013).This might be due to presence of traditional practices in this study area applying different substances commonly after cord cut commonly butter 24.4%.
This study showed the odds of mothers who live in urban areas 2.332 to practiced ENBCP compared to live in rural area(AOR:2.332;95%CI:1.082,4.607,P<0.030).This finding is in line with study conducted in Wolayita , Damot Pulas district 2 times higher in urban areas women to practiced newborn practices compared to rural areas(AOR =2,P = 0.042, CI = 1.024–3.693)(Chichiabellu et al., 2018)and another study conducted in Metekel , Mandura district the likelihood of good newborn practice was 3 times higher among urban residents compared to rural once (AOR=3.26 95% CI: 1.90-5.57)(Tegene et al., 2015).This might be due to accessibility of health service, media coverage and good awareness secondary to better educational status of urban women compared to rural women.
In this study mothers not visited by health extension worker during postnatal period were 37% times less likely practiced essential newborn care practices when compared with those home was visited by HEW during postnatal period (AOR:0.618 ;95% CI:0.400,0.954,p<0.010). This study finding is in line with research conducted in East Gojam ,Awabel district ,those mothers had immediate PNC visited 3.22 times practiced ENBCP than those their home was not visited (OR=3.22, 95% CI = 1.18, 9.48) (Kokebie et al., 2014) and study done in Hosana town ,those mothers had not PNC visit 0.209 times less practice NBCP while compared to those had immediate PNC home visit by HEW(AOR = 0.209,P = 0.00,CI = 0.110–0.399)(SAKELO, 2018).Another study in Gamo Gofa zone, Chencha district showed the odds of good ENC practice were 3.27 among mothers who had immediate postnatal care(AOR = 3.27, 95%CI: 1.99, 5.35) than counterparts(Mersha et al., 2018).This might be due to health extension worker give proper advise about ENBCP during the visit.
In this study findings the odds of mothers assisted by HEW during home delivery 3.617 to practice ENBCP (AOR=3.617 95%CI: 1.058-4.607 p<0.040) than assisted by traditional birth assistant. This might be since HEW gives proper counseling to mothers to practice good essential newborn care .Those mothers assisted by relatives were 57% times less likely to practiced ENBCP compared to those assisted by traditional birth assistant(AOR:0.427 ;95%CI:0.221,0.821, p<0.011) .This might be due to currently awareness creation to traditional birth assistants given by different stakeholders especially to promote skill birth attendants’ and TBAs also have experience and acceptance by the communities and they might be promote mothers to practiced good essential newborn care practices when they awareness raised.
This research also showed that those mothers have not knowing poor or not able to breast sucking as neonatal danger sign 48% times less likely to practice ENBCP compared to those who know poor sucking as neonatal danger sign (AOR:0.524;95% CI :0.332,0.826, p<0.005).This is in line with study conducted in Ghana those mothers had knowledge of dander sign 4.7 time practice than counterparts(AOR=4.7,CI:2.43-9.28,p<0.001)(Saaka and Iddrisu, 2014) and Wolayita Damot pawula district those mothers had no danger sign knowledge 72% times less likely practiced ENBC than had knowledge about danger signs(AOR = 0.277, P = 0.006, CI = 0.110–0.697)(Chichiabellu et al., 2018) .This may be due to similarity advise given about poor sucking of newborn as neonatal danger sign by health workers in these areas . This study finding also showed those mothers visited last ANC at health post were 52% times less likely to practice than had visited at health center(AOR:0.485;95% CI:0. 299,0.785,p<0.003) .This might be counseling about ENBCP given at health center level had more quality than at health post level.
Although studies done in East Gojam, Awabel distric, Metekel ,Mandura district Hosana town reported that educational status has positively associated with good essential newborn care practice(Kokebie et al., 2014, Tegene et al., 2015, SAKELO, 2018)where as in the present study there is no statically significant association between educational status and essential newborn care practice. This discrepancy might be due to social-demographic characteristics difference between respondents and also in this study area majority of mothers have not formal education compared to others.
Attending pregnant monthly mother meeting did not association within essential newborn care practices in this study .However study done in East Gojam, Awabel district and Gamo Gofa ,Chencha district reported as attending monthly pregnant mother meeting has positively associated with good essential newborn care practices (Kokebie et al., 2014, Mersha et al., 2018). The possible reason for this might be the difference in conducting monthly pregnant mothers continuously and advice given about essential newborn care practices by making main agenda in this study area might have difference.
Studies done in Aksum town, Hosanna town reported that having 2-3 number of children has positively associated with good essential newborn care practice (SAKELO, 2018, Berhe et al., 2016). But in this study area did not association with essential newborn care practice. The possible reason might be mothers in this study area might not remembered experience from the prior birth and this might be due to awareness difference between respondents in understanding poor practices.
Conclusion
This study showed that the level of good essential new-born care practices found to be very low compared to findings of different literatures previously conducted in different areas. Over all good essential new-born care practice found was 18.9% (early initiation of breast feeding 26%, safe cord care practice 28.9% and Thermal care practice 30.8%). Initiation of breast feeding after one hours, applying substances after cord cut, not delaying to bath the new-born for the first 24 hours and not at all having skin to skin contact between mothers and new born for the first 24 hours, were practiced by majority of study participants in the study area which is contradicted with the standards recommended. As in this study finding revealed different factors such as urban residences and home delivery assisted by HEW were positively associated with essential new-born care practices for home delivered mothers and not home visit by health extension workers during PNC, having last ANC visit at health post, home delivery assisted by relatives and didn’t knowing poor sucking as neonatal danger sign were factors negatively associated with essential new-born care practices.
Declaration
Ethics Approval and Consent to participate Ethical clearance letter was obtained from Madda Walabu University and given for Oromia health bureau, then to West Guji zone health department and letter obtained from zonal health department was given for all concerned bodies including Abaya health office who gave permission to conduct the study. After the objective of the study clearly told to the participants by their own language and the advantage were explained for the participants and the only disadvantage to them were taking the time. They would have been told about the strict confidentiality and no respondents name were written rather only code were given to all respondents to keep confidentiality as well as when needed as they had the right to withdraw during the interview, informed verbal consent were obtained from those the respondents prior to interview started.
Consent for publication
Consent for publication is not necessary, because this manuscript did not contain any personal detail like photo, image and video data
Availability of data and Material
The data sets used or analysed data currently availed in the hand of corresponding author and can be asked any time for reasonable request.
Competing interests
Authors declared that, there is no competing interest regarding to this manuscript.
Funding
There is no funder for this research thesis and the full paper cost had been covered by the author. No organization fund for this paper.
Authors’ contributions
Nigusu Derese developed and organized the materials and designs the study, perform analysis and interpret the data. Kemal Ahmed and Edao Tesa assisted with design, the analysis and interpretation the correspondence author through whole thesis work validation. Tariku Derese participated in the various aspect of this paper development especially on contents development. Tariku Derese also writes up and drafted the manuscript and all the authors read and approved the final manuscript.
Acknowledgments
First of all, I would like to thanks Madda Walabu University. I would also thanks Mr. Kemal Ahmed and Mr. Edao Tesa for their valuable and constructive comment they gave me throughout my thesis work.
This is also a right time to me to express my great thanks to my data collectors, supervisors and respondents for their invaluable support during data collection. Finally, it is my pleasure to thanks all my families for their continuous assistance and help during throughout my thesis work.