
Chhabra S
Mahatma Gandhi Institute of Medical Sciences, India
*Corresponding author: Chhabra S, Mahatma Gandhi Institute of Medical Sciences, India
E-mail: chhabra_s@rediffmail.com , schhabra@mgims.ac.in
Chhabra S
Mahatma Gandhi Institute of Medical Sciences, India
*Corresponding author: Chhabra S, Mahatma Gandhi Institute of Medical Sciences, India
E-mail: chhabra_s@rediffmail.com , schhabra@mgims.ac.in
Received date: November 09, 2020; Accepted date: November 20, 2020; Published date: November 29, 2020
Citation: Chhabra S., (2020) Abortion Services at Health Facilities. Women’s Health Care and Analysis, 1(1); DOI: http;//doi.org/03.2020/1.1001
Copyright: © 2020 Chhabra S, This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background
Induced abortion (IA) performed safely at safe place is one of safest procedures. Spontaneous abortion (SA), most common adverse event of pregnancy, need not cause problems. But complications do, occur with both. SA can recur too. It is essential to have needed services, and proper records.
Objective
To know about abortion services, records at health facilities.
Material Methods
Records of IA, SA cases managed at ten health facilities each in two Districts were analyzed.
Results
It was not possible to know abortions burden at health facilities. At medical colleges, of randomly seen 10 SA,10 IA records each 90%, 50% each respectively in Wardha,100%in Amravati were of first trimester, managed by medical officers.SA in District Hospitals, were managed by MOs, 10%medically in Wardha, 40% medically Amravati. Recorded IA in Sub District Hospital (SDH) Wardha were of first trimester managed by MOs, IA 20% surgically, 40% medically, 40% mix method, SA 20% medically, 30% mixed method. All 21 recorded SA and IA for whole year at SDH Amravati were of first trimester managed by MOs, 5 IA surgically, two IA medically, all 14SA Medically. Five SA records from private hospital, were of first trimester managed surgically in Wardha,40% medically on Amravati, 5 each IA of first trimester managed by specialists surgically. There were no abortion records in Primary Health Centers (PHCs) Sub centers (SCS) of Wardha. In Amravati all 16 SA recorded, for whole year at 3 PHCs 9at 3 SCs, were of first trimester managed by nurse midwives medically. Reasons recorded for IA in all HF were contraceptive failure or no contraception mixed, health reasons, poverty.
Conclusion
Abortion records were incomplete, not very useful for policies/ programs, services. There was need of awareness of contraception, second trimester abortion dangers, medical abortion, availability of abortion services at peripheral health facilities.
Background
Aanganwadi workers, Accredited Social Health Activists (ASHAs) and nurse midwives do use Aanganwadis for mother and child care, antenatal services, but Sub-centre (SC) is the first contact health point between community and the public health system in true sense. The success of national programmes depends largely on well-functioning SCs and Primary Health Centers (PHCs) for providing basic services of acceptable standards. However Pasricha et al (1) reported that studies have shown that ensuring accessibility and availability of quality primary health care through SCs were major concerns. Kumutha et al (2) reported that the launch of National Rural Health Mission in India provided the opportunity to have a fresh look at functioning of PHCs and SCs for women’s reproductive health services which included abortion services. Stillman et al (3) reported that while abortion has been legal in India for around 5 decades, unsafe abortions persist, particularly in the rural areas. Records need to be complete at the health facilities where IA are performed or SA are managed. Chaturvedi et al 4) reported that availability and distribution of abortion care facilities can influence women's access to these services, especially in rural areas.
Objectives
Objectives of the study were to collect information of status of abortion services and records at different health facilities of two districts in Maharashtra for knowing about abortion services, cases managed, methods and gaps.
Material And Methods
Institute’s ethics committee’s approval was taken before initiation of the study. Mapping of health facilities (government and private): was tried, in both the districts of Maharashtra province of India. Information was collected from 10 health facilities (HF)each in both the districts, one Medical College (MC), District Hospital (DH), Sub district Hospital (SDH), one Private Hospital (PH) each three Primary Health Centres (PHCs), and Sub centers (SCs). However there were limitations, as the HF were at the borders of four states. Many women, not only from nearby Districts, but from nearby States also sought services from the HF. Issues of permissions and confidentiality were other challenges for having information from the health facilities in the two big districts. Whatever information was possible by looking at records without any conflicts was collected using a predesigned tool. Permission of incharge of abortion services in each HF was taken with assurance of confidentiality. It was not possible to know the exact burden of abortion care because of non availability / incomplete records and various other reasons including confidentiality. However in spite of so many odds some useful information could be collected.
Results
In the MC of Wardha district of 10 randomly seen SA case records, 2 were of less than 6 weeks, 4 of 6-9 weeks and 4 of 10-13 weeks pregnancy. Seen records revealed abortion cases managed by specialists, 8 surgically and 2 medically. Of the 10 records of IA, one was of less than 6 weeks, one of more than 6 but less than 10 weeks, 3 of 10-13 weeks, 3 of 14-17 weeks and 2 of 18-20 weeks pregnancy,(5 IA second trimester, only2 of less than 10 weeks). Records revealed 4 IA managed by medical officers and 6 by specialists,7 surgically and 3 medically. Recorded indications in 3 were spacing and in 5mix of spacing/ no use of contraceptive /failure of contraception and 2 records had health reasons without any details of the health problems.
In DH also of10 SA records,7 were of 6-9 weeks and 3 of 10-13 weeks, managed by medical officers, 9 surgically and one medically. Of the 10 IA records, four were of 6-9 weeks pregnancy, 3 of 10-13 weeks and 3 of 14-17 weeks managed by medical officers, 6 surgically and 4 medically. One woman’s records had single mother as an indication. Eight nonuse or failure of contraception put together and one had health reason recorded.
In SDH of 10 SA records, 3 had less than 6 weeks pregnancy recorded, 6 of 6-9 weeks and one of 10-13 weeks, all managed by medical officers, 5 surgically, 2 medically and 3 by both methods. Of the 10 IA records, one was of less than 6 weeks, 4 of 6-9 weeks, 3 of 10-13 weeks and 2 of14-17 weeks pregnancy, all managed by medical officers. 2 surgically and 4 medically and 4 by mixed method. One woman’s records revealed single mother, 7 nonuse or contraception failure and two had health reasons recorded without any more details. There were no untoward event recorded.
In private hospital of Wardha of 5SA, one was of 6 weeks, one 6-9 weeks and 3 of 10-13 weeks managed by specialists surgically. Of the 5 I records, 2 were of less than 6 weeks, one of 6-9 weeks and 2 of 10-13 weeks, all managed by specialists, 4 surgically and one medically. In 2 cases, reasons for IA recorded were failure /nonuse of contraception mixed and 3 had health reasons recorded. In 3 PHCs and 3 SCs visited in Wardha district, there were no abortion records.
In Amravati district also in the MC of 10 SA records seen randomly,4 were of 6-9 weeks pregnancy, 5 of 10 to 13 weeks and one of 18 to 20 weeks, managed by specialists, 7 surgically and 3 medically. Of the 10IA records, 3were of less than 6 weeks pregnancy,4 of 6-9 weeks and 3of 10-13 weeks. Seven cases were managed by specialists surgically and 3 medically. Recorded indications of abortions were spacing in 2, single mother in one, failure or nonuse of contraception in 3, and4 had health problems recorded. In DH of 10 SA records, 3 were of less than 6 weeks pregnancy, 4 of 6-9 weeks, 3 of 10-13 weeks and 4 of 14-17 weeks, ratio of 3 to 2 of first and second trimester pregnancy. All records revealed management by medical officers, 6 surgically and 4 medically. Of 10 records of IA managed, 2 were incomplete and it was not possible to know anything. Of the left8 cases, one IA was for less than 6 weeks pregnancy, 2 of 6-9 weeks, 3 of 10-13 weeks and 2 of 14-17 weeks, managed by medical officers. 6 surgically and 2 by medication. Recorded reasons for IA were single mother in 2, nonuse or failure of contraception mixed in 4 and 2 records had health problems recorded. In SDH of Melghat region, there were 21 cases recorded for the whole year. So all were seen,14 of SA, 4 of less than 6 weeks pregnancy, 8 of 6-9 weeks pregnancy and 2 of 10-13 weeks, all managed medically by medical officers. Seven records were of IA, one of less than 6 weeks, 5 of 6-9 weeks and one of 10-13 weeks pregnancy managed by medical officers, 5 surgically and 2 medically. Recorded indications of IA were spacing in five, one had single mother and one had failure or non-use of contraceptive put together. In 3 PHCs of Melghat region, 16 cases of SA,(5 of 6-9 weeks pregnancy, 6 of 10-13 weeks and 5 of 14-17 weeks) and in 3 SCs, 9 cases of SA, (7 of 10-13 weeks and 2 of 14-17 weeks)were recorded for the whole year. All were managed by nurse midwives medically. There were no records of IA in the PHCS and SCs of Melghat region also. In PH of Amravati of randomly seen, 5 records of SA, (4 of 6-9 weeks and one of 10-13 weeks managed surgically) and5 IA, 3 surgically and 2 medically managed by specialists .Indications were nonuse of contraception in one, health reasons in four.
Discussion
The MTP Act stipulates that all public sector facilities at the primary health center (PHC) level and higher are to provide abortion services, but such services are rarely available at the lower levels of the public health care system, which often serve as the first access point for reproductive
health care, including abortion. Indeed, recent multistate abortion facility assessments estimate that only 5–58% of PHCs offer abortion services [2]. PHCs not offering these services commonly cite the absence of a provider trained in surgical methods or the lack of equipment and/or infrastruc-ture required to provide surgical abortion services as barriers. The MTP Act stipulates that all public sector facilities at the primary health center (PHC) level and higher are to provide abortion services, but such services are rarely available at the lower levels of the public health care system, which often serve as the first access point for reproductive health care, including abortion. Indeed, recent multistate abortion facility assessments estimate that only 5–58% of PHCs offer abortion services [2]. PHCs not offering these services commonly cite the absence of a provider trained in surgical methods or the lack of equipment and/or infrastruc- ture required to provide surgical abortion services as barriers. The MTP Act stipulates that all public sector facilities at the primary health center (PHC) level and higher are to provide abortion services, but such services are rarely available at the lower levels of the public health care system, which often serve as the first access point for reproductive health care, including abortion. Indeed, recent multistate abortion facility assessments estimate that only 5–58% of PHCs offer abortion services [2]. PHCs not offering these services commonly cite the absence of a provider trained in surgical methods or the lack of equipment and/or infrastruc-ture required to provide surgical abortion services as barriers.The Medical Termination of Pregnancy Act of India stipulates that all public sector facilities, PHCs to higher centre need to provide abortion services, but such services are rarely available at the PHCs, which serve as the second access point for reproductive health care, including abortion care. Khan et al [5] did multistate abortion facility assessments and reported that only5–58% of PHCs offered abortion services. PHCs were not offering abortion services and commonly sited reasons were the absence of trained provider or lack of equipment or infrastructure required to provide surgical abortion services as barriers. Study by Mundle et al [6] suggested that good community outreach should be an essential component of successful medical abortion provision in rural settings. The medical officers and health providers at the PHCs ,including community health outreach workers, have long-standing relationships with the community. They ultimately inform women about the availability of the services and serve as an entry point for home visits to trace women who needed information and help. Mundle et al [6] also reported that medical abortion provision was sure feasible and acceptable in an Indian rural PHC. Study suggested that introduction of medical abortion at lower levels of the health-care system could increase access to safe abortion in rural India. Of 50% SA records seen half were of first trimester in MC of Wardha, all of first trimester in Amravati, managed by specialists, 70% surgically as well as medically in both the districts. No case was managed only medically. More awareness about medical means is needed. There were two MCs in the district in addition to DH, SDH and rural hospitals, still women waited till second trimester for IA in Wardha. In Amravati district IA cases recorded were of first trimester. It is well known that complications are more in second trimester and needed to be avoided. Probably because of abortion law, all IA cases in PH recorded were of first trimester with contraception failure or nonuse of contraception as indication. For second trimester IAs two authorized signatures were needed. In Wardha 70% SA cases were of 6-9 weeks and 30% of10-13 weeks pregnancy and in Amravati district 60% were of 6-9 weeks, 20% 10-13 weeks and 20% of 14-18 weeks pregnancy and were managed by medical officers, 90% surgically and 10% medically in Wardha and 60% surgically and 40% by medication in Amravati. Again it reflected availability / no availability of skilled persons. As per records 50% IA were performed for unwanted pregnancy without use of contraception, 30% for spacing with no contraception, 20% had health reasons recorded without any details of health problems women might be having. Ten to 20% records had single mother recorded. Single mother as a reason for IA was at all levels. There was visible high unmet need with probably no knowledge or use of emergency contraception. Wherever spacing was recorded it was not possible to know whether anything was done for planning family. Similarly failure or no use of contraceptive were recorded together. It made a big difference between failure of contraception and no use of contraception for policies, programs as well as services. Also method might not have been effective or use was wrong. It is essential to know whether it is nonuse or failure because both will need different actions. Also it was not possible to know what were the health reasons which were recorded at all levels of health care. It is essential for health of women that details are known. Further it is essential to have some formatting in tools used for records with clear indication as it will help in making policies, programs, planning services and for actions at community level too. In Amravati district most commonly recorded reason was spacing (80%). In Sewagram region PHCs and SCs had no records of abortion management as higher facilities were easy to crest. In Melghat region at SCs and PHCs SA were recorded, majority of first trimester pregnancy, managed by nurse midwives medically as usually there were no doctors available. There were no records of IA in Amravati peripheral health facilities also. There was no evidence in any records that women had sex selective abortions. There seemed a lot of difference what was recorded in the health facility and what was found in abortion study in villages of Melghat block of Amravati, Sewagram region of Wardha(unpublished). It is essential that PHCs and SCs to have infrastructure and women know about availability of abortion services so that they can easily access them and whatever services are provided are recorded properly. Kapp et al [7] advocated that high-quality abortion service should be offered to women with choice between abortion methods with provision of the one they preferred. Berer [8] further reported that abortion services not only needed to be treated as a bonafide form of health care but also completely reconceptualized, particularly because of the influence of medical abortion pills. Abortion care is a fundamental part of women’s reproductive health care. Surgical and medical abortion methods are safe and effective throughout the gestational age range wherein abortions are performed but risks increase with the increase in duration of pregnancy being terminated, rates of complications remain low and comparable between surgical and medical techniques. Study by Dickson et al [9] revealed service provision in provinces was inadequate or lacking in South Africa. Although in the first years following the new legislation efforts were made to establish abortion services. This Study revealed gross inequality in service availability. Strategies for improving coverage were suggested. The same was found in peripheral HF in the present study too. A lot of awareness is needed. Gallo et al [10] did a study about abortion services in Mozambique and reported that women reported lengthy waiting times from arrival to treatment. Less than half the women said they received follow-up care information, and only 27% of women wanting to avoid pregnancy said they had received a contraceptive method. Use of dilatation and curettage was far more common than medical or aspiration abortion methods. Chaturvedi et al [4] did a study and overall, 48% of facilities reported an ability to provide safe surgical abortion services. Of public centers, 32% reported the ability compared to 100% among private centers while 18% of public centers and 77% of private centers had performed an abortion in the last 3 months. The availability of abortion services was higher at higher facility levels with better equipped and skilled personnel availability, in urban areas and in private sector facilities. Mizana et al [11] did a facility based cross sectional study in South West Ethiopia reported that the majority of women delayed the decision of safe abortion services. Place of residence of the women, lack of formal education, history of previous abortion and late confirmation of pregnancy were the determinant factors for women’s decision for safe abortion. It is essential to work on awareness creation of the timing of safe abortion and complications of delay abortion especially for the women from rural area.
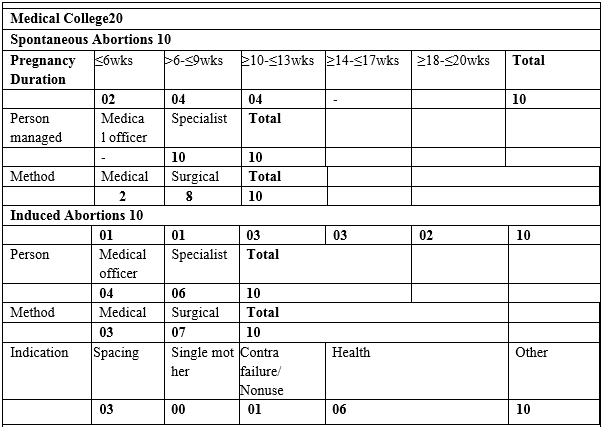
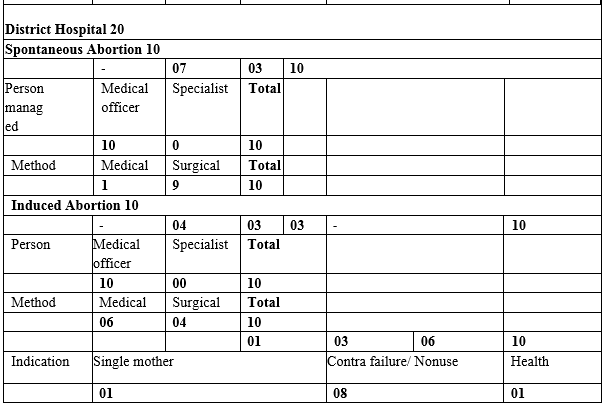
Table 1: Abortion Records at Health Facilities Of Wardha.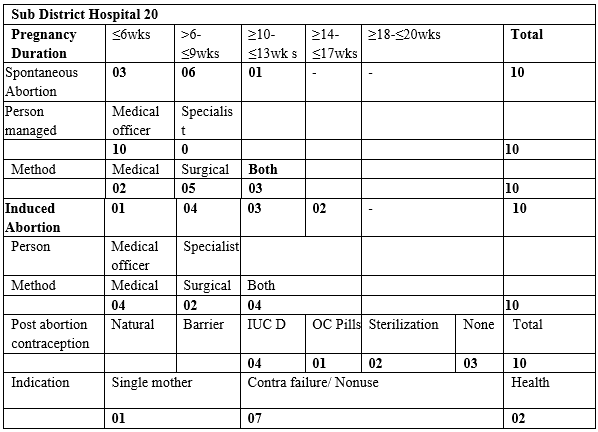
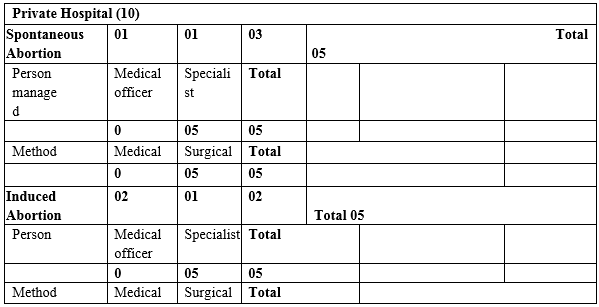
Table I: Abortion Services Recorded at Health Facilities Of Wardha. B
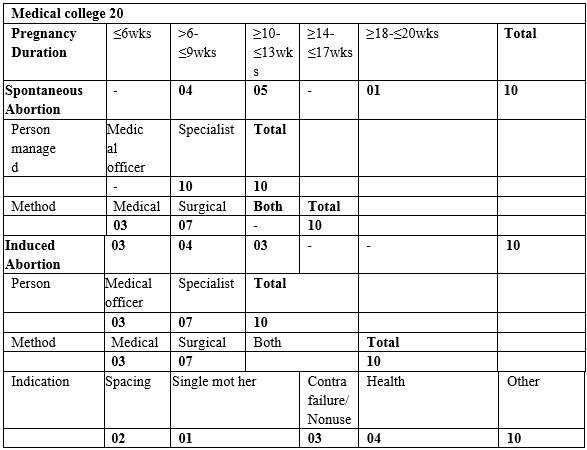
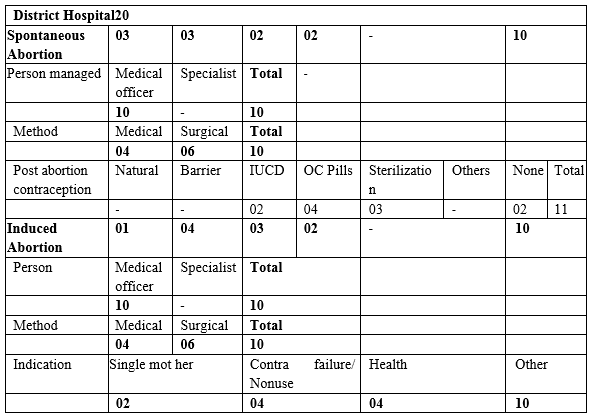
Table II: Abortion Records at Amravati District A
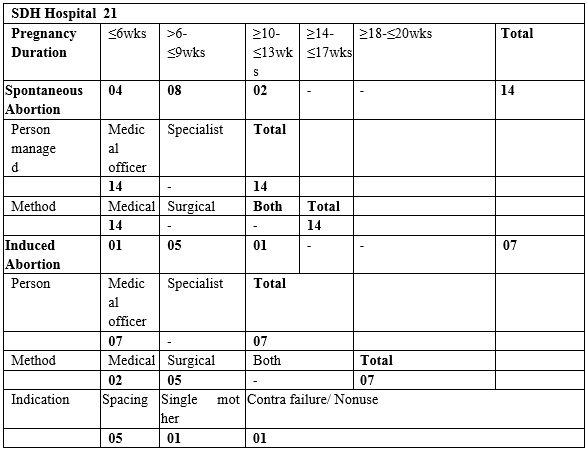
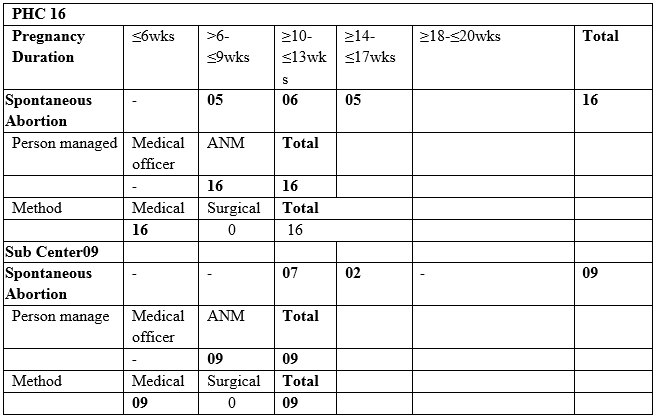
Table II: Abortions Recorded in Amravati District B
Acknowledgement
We are grateful to the Indian Council of Medical Research (ICMR), New Delhi for the financial support for doing the study and everybody connected with the study. We thank the rural tribal women for the cooperation in conducting the study. Thanks are due to colleagues Dr. Suchi Jain, Dr. Naina Kumar, Dr. Ketki, research assistants and office staff for the information collected and help in analysis of the data and documentation.