Journal of Dermatology and Venereology
OPEN ACCESS | Volume 4 - Issue 1 - 2026
ISSN No: 3065-677X | Journal DOI: 10.61148/3065-677X/JDV
Garima Anandani 1*, Vaishali Bhankhodia 1, Parth Goswami 1, Yash Thesiya 2, Avani Dangar 2, Rinkal Madhudiya 3
1Assistant Professor, Department of Pathology, AIIMS Rajkot.
2Senior Resident, Department of Pathology, AIIMS Rajkot.
3Assistant Professor, Department of Dermatology, Venereology and Leprosy, AIIMS Rajkot.
*Corresponding author: Garima Anandani, MD Pathology, Assistant Professor, Department of Pathology, Academic Block, AIIMS Rajkot, Parapipaliya, Khanderi, Rajkot, Gujarat.
Received: December 17, 2025 | Accepted: December 24, 2025 | Published: December 26, 2025
Citation: Anandani G, Bhankhodia V, Goswami P, Thesiya Y, Dangar A, Madhudiya R., (2025) “Biphasic Primary Localized Cutaneous Amyloidosis: An Unusual Case Report” Journal of Dermatology and Venereology, 3(2); DOI: 10.61148/3065-677X/JDV/060.
Copyright: © 2025 Garima Anandani. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cutaneous amyloidosis is a skin disorder where amyloid deposits in skin usually without affecting the rest of the body. It includes macular, lichen, nodular and biphasic types, with lichen amyloidosis being the most common. It usually appears on the shins, forearms, and upper back as dark, itchy spots and plaques. The condition may be caused by chronic scratching and friction, which harm skin cells and lead to amyloid formation. Genetic factors, especially in Asian populations, increase risk, and mutations in certain genes have been linked to this disorder. Diagnosis is typically confirmed through a biopsy showing specific deposits in the skin that react positively to certain stains.
Herein, we report a 26-year-old woman with a severe itching on her lower legs and forearms. Biopsy indicated a diagnosis of cutaneous amyloidosis. It was identified to be a biphasic primary cutaneous localized amyloidosis after ruling out systemic amyloidosis. Treatment included topical corticosteroids, a retinoid, and emollients, leading to improvement without recurrence or systemic disease at a six-month follow-up.
cutaneous amyloidosis, severe itching, biphasic, primary localized
Nevus spilus (NS), also known as speckled lentiginous nevus, spot on spot, Cutaneous amyloidosis encompasses a range of conditions marked by amyloid accumulation in the skin, devoid of systemic involvement [1]. It is primarily categorized into macular, lichen, and nodular varieties, with lichen amyloidosis being the most prevalent. The condition generally impacts the shins, forearms, and upper back, manifesting as hyperpigmented papules and plaques with severe itching [3].
The pathophysiology is believed to entail persistent scratching and friction, resulting in keratinocyte destruction, death, and subsequent amyloid production from keratin filaments [4]. Genetic predisposition significantly influences outcomes, especially in Asian populations, where a higher prevalence has been recorded [5]. Mutations in the OSMR and IL31RA genes have been associated with atopy and pruritic dermatoses [6].
Cutaneous amyloidosis is epidemiologically more common in Southeast Asia and South America, with studies indicating incidence rates of 10–15% in Taiwan and specific areas of Brazil [7]. It is infrequent among Western populations [8]. The majority of instances are documented in the fifth to sixth decades of life, making its manifestation in younger persons, as exemplified by our case, atypical [9].
Histopathological examination is the definitive diagnostic method, revealing acellular eosinophilic amorphous deposits in the papillary dermis that exhibit positive staining with Congo red and demonstrate apple-green birefringence under polarized light [10].
Case Presentation
We report a 26-year-old female with a history of atopy, who presented with severe itching and scratching over bilateral lower legs and forearms for past six months. Local examination revealed rippled macules and papules coalescing into plaques and patches on bilateral lower legs and forearms (Fig-1). A biopsy was performed on the right medial malleolus of the right leg.

Figure 1: Local examination showing macules and papules coalescing into plaques and patches on leg.
Grossly single skin covered greyish white tissue bit measuring 0.3x0.3x0.2 cm was received. On microscopic examination, epidermis showed irregular acanthosis with presence of intraepidermal acellular eosinophilic amorphous accumulation. The superficial dermis also showed acellular eosinophilic accumulation adhering at the dermo-epidermal junction, perivascular and peri-adnexal areas (Fig-2). The eosinophilic deposits discoloured red under Congo red staining and apple green when viewed with polarized light. A diagnosis of cutaneous amyloidosis was made.
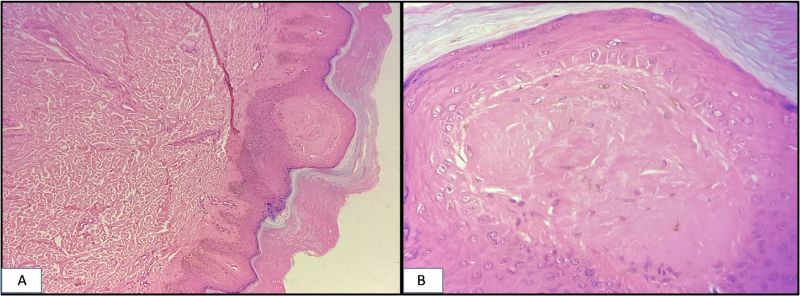
Figure 2: Epidermis showing irregular acanthosis with presence of intraepidermal acellular eosinophilic amorphous accumulation. (Haematoxylin & Eosin stain) A.100X magnification B. 400X magnification.
No familial history of systemic illnesses was present. In contrast to hereditary amyloidosis, an autosomal dominant disorder usually manifesting between the ages of 5 and 15, our patient was 26 years old. To exclude primary systemic amyloidosis, chest radiography, abdomen ultrasonography, urinalysis, and complete blood count tests were conducted, all of which yielded normal results and indicated no evidence of a systemic component of amyloidosis. After exclusion of systemic amyloidosis, the case was diagnosed to be biphasic primary cutaneous localised amyloidosis. The patient was managed and improved with topical corticosteroids (mometasone), topical retinoid (tazarotene), and emollients (liquid paraffin). At 6 months follow-up, there were no signs of recurrence or systemic disease.
Discussion
The clinical classification of amyloidosis, based on patient presentation, categorizes it into main, secondary, familial, and isolated forms. The prevalent clinical amyloid types include AL, AA, ATTR, and Ab2M, categorized by the specific protein involved. Cutaneous amyloid deposits are observed in 29-40% of primary systemic amyloidosis patients, but are exceedingly uncommon in other systemic variants. When cutaneous amyloidosis is not indicative of systemic amyloidosis, it is referred to as primary localized cutaneous amyloidosis [11].
There are four varieties of primary localized cutaneous amyloidosis: nodular amyloidosis, macular amyloidosis, lichen amyloidosis, and a combined form of lichen and macules known as biphasic amyloidosis. Lichen is the predominant subtype distinguished by many, localized or widespread, clustered papules with a preference for the shins. Macular is defined by numerous brown-grey macules with a reticulated or rippling pattern, predominantly affecting the upper back. Nodular is the rarest kind, characterized by firm pink to brown nodules predominantly affecting the extremities. The size of nodules ranges from several millimeters to centimeters and may merge to form plaques [12]. The primary symptom of macular and lichen amyloidosis is pruritus, which is hardly observed in the nodular variant [11].
Most documented instances of cutaneous amyloidosis arise in the fifth to sixth decade, in contrast to our case, which appeared in the third decade. Chang et al. performed an epidemiological investigation in Taiwan, revealing that the average age of onset was between 50 and 60 years, with a female predominance of 2:1 [7]. In contrast, our patient was significantly younger, indicating an early onset variation maybe associated with her atopic history. Morales-Callaghan et al. delineated a correlation between cutaneous amyloidosis and an atopic predisposition, highlighting the significance of IL-31–mediated pruritus in the pathogenesis of amyloid formation [13]. This aligns with our case, as the patient had a personal history of atopy, indicating that pruritic dermatoses may expedite amyloid deposition.
Wong et al. posited that persistent scratching and friction are critical pathogenic catalysts in lichen amyloidosis [5]. The patient exhibited intense pruritus and excoriation for six months, which aligns with this observation and corroborates the "filamentous degeneration" hypothesis. Cheng et al. investigated families with OSMR gene mutations and demonstrated the hereditary transmission of primary localized cutaneous amyloidosis [14]. Conversely, our patient lacked a familial history of analogous lesions, indicating that the condition may also manifest sporadically in young adults without a genetic susceptibility.
Miteva and Romanelli evaluated therapeutic alternatives and observed diverse reactions to corticosteroids, retinoids, and phototherapy [9]. In our investigation, the patient exhibited significant clinical improvement with topical corticosteroids and retinoids, aligning with prior data. In contrast to certain resistant cases necessitating phototherapy or laser treatment, our patient exhibited a favourable response to first-line therapy. Local amyloidosis has a propensity to advance to a systemic illness in at least 7% of cases, with reported rates reaching up to 50%. The necessity for follow-up remains to be proven due to this extensive gap [11].
Conclusion
This case highlights a rare presentation of biphasic primary localized cutaneous amyloidosis in a young adult with an atopic background, an age group in which the condition is infrequently reported. The findings support the role of chronic pruritus and scratching in amyloid deposition, even in the absence of genetic or familial predisposition. Histopathology with Congo red staining remains pivotal for diagnosis, and thorough evaluation is essential to exclude systemic involvement. Early recognition and appropriate topical therapy can result in good clinical outcomes, though long-term follow-up is warranted due to the potential risk of systemic progression.
Conflict of interest
The authors declare no conflict of interest.
Ethical statement
The authors confirm that we have adhered to the ethical policies of the journal. No identification details of the patient are shared.
Consent
Written informed consent was obtained from the patient to publish this report in accordance with the journal's patient consent policy.
Funding
No funds were received or used.