Journal of Dermatology and Venereology
OPEN ACCESS | Volume 4 - Issue 1 - 2026
ISSN No: 3065-677X | Journal DOI: 10.61148/3065-677X/JDV
Ikrame BEJJA*, Hanane BAYBAY, Sara ELLOUDI, Meryem SOUGHI, Zakia DOUHI, Fatima Zahra MERNISSI
Department of Dermatology, Hassan II University Hospital Center, Fez, Morocco.
*Corresponding author: Ikrame BEJJA, Department of Dermatology, Hassan II University Hospital Center, Fez, Morocco.
Received: November 05, 2025 | Accepted: November 10, 2025 | Published: November 15, 2025
Citation: BEJJA I, BAYBAY H, ELLOUDI S, SOUGHI M, DOUHI Z, Fatima Z MERNISSI., (2025) “Malignant Transformation in Nevus Spilus: Is it a Real?.” Journal of Dermatology and Venereology, 3(2); DOI: 10.61148/3065-677X/JDV/059.
Copyright: © 2025 Ikrame BEJJA. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Nevus spilus (NS) is a rare melanocytic lesion characterized by a light brown background with darker macules and papules. Although melanoma arising from NS is infrequent, it can occur and poses a risk for malignant transformation. We report the case of a 60-year-old female with a history of hypertension who presented with a melanoma originating from a congenital nevus on the right thigh, which had undergone recent changes. The patient consulted at a late stage of metastases, with the culpable lesion being the degenerated nevus spilus. This case underscores the necessity of vigilant monitoring and early detection of changes in nevi, particularly in concealed areas.
Melanoma, Nevus spilus, Congenital nevus, dermoscopy
Nevus spilus (NS), also known as speckled lentiginous nevus, spot on spot, spotty nevus, or nevus on nevus, is a skin lesion found in approximately 0.2% to 2.3% of the population, rendering it a relatively uncommon condition [1]. This lesion is characterized by darkly pigmented macules and/or papules over a background of hyperpigmentation. While there have been documented cases of melanoma developing within NS, the extent of its malignant potential remains uncertain. This report presents a patient with synchronous melanomas arising from a nevus spilus, underscoring the importance of awareness and vigilance in monitoring these lesions for signs of transformation.
Case report :
A 60-year-old female patient with a history of hypertension was referred by gynecologists to our facility for evaluation of a potential primary breast melanoma. The onset of her condition dates back four months when the patient presented with mastodynia and a palpable lesion in the left breast, prompting her consultation with gynecologists. This was followed by an echomammography, which revealed a 2 cm tissue lesion located in the axillary extension of the left breast, classified as ACR4. They subsequently performed a biopsy, and the histological results were consistent with an undifferentiated tumor process expressing PS100, Melan A, HMB45, and a Ki-67 index of 30% in immunohistochemistry, compatible with the diagnosis of melanoma. Dermatological examination revealed a brown muscular plaque on the posterior aspect of the right thigh, ovular in shape, well-defined with irregular contours, measuring 5 cm in its major axis, containing islands of hyperpigmentation with multiple clustered brown papules of elastic consistency (Figure 1). Dermoscopic examination showed a blue-white veil in certain areas, perifollicular hyperpigmentation, and a polymorphic vascular pattern (figure 2). Examination of the lymphatic regions demonstrated two firm, painless, and fixed right inguinal lymphadenopathies with respect to the deep plane, without other anomalies. Upon further interrogation of the patient regarding the thigh lesion, she confirmed its congenital nature with a recent undetermined change in evolution. The diagnosis of melanoma arising from a congenital nevus was suggested. A biopsy was performed, revealing a dermal tumor proliferation composed of melanocytes with moderate cellular density, organized in sheets while respecting the "grenz zone," with good maturation in depth. The cells displayed mild to moderate cytonuclear atypia without functional activity, concluding a diagnosis of moderately atypical dermal melanocytic proliferation. An additional immunohistochemical assessment showed expression of Melan A, PS100, and a Ki-67 index of 10%. All findings support the diagnosis of melanoma on a congenital nevus with a Breslow thickness of 4 mm, without vascular invasion or nerve invasion. A staging workup was conducted, revealing multiple metastases in the cerebral, osseous, pulmonary, hepatic, and peritoneal regions. The patient was then referred to oncology for management.

Figure 1 : Clinical image of Nevus Spilus on the thigh surmounted by multiple brown and another bluish papules
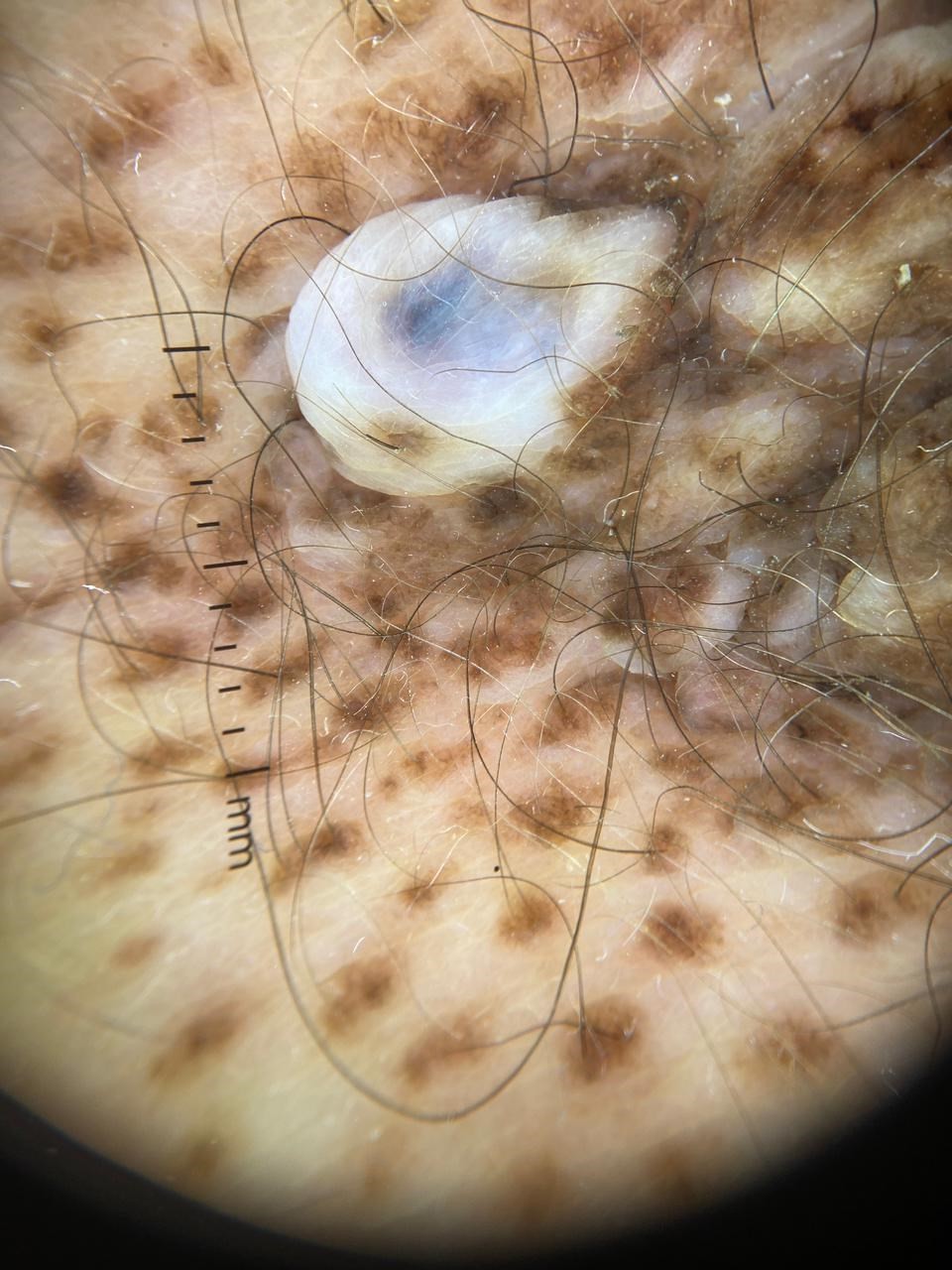
Figure 2 : Dermoscopy showing a blue-white veil, perifollicular hyperpigmentation, and a polymorphic vascular pattern
Discussion:
First described by Burkley in 1842 [2], naevus spills (NS) is characterized by a café-au-lait spot overlaid with more pigmented macules or papules. Histologically, it corresponds to lentiginous melanocytic hyperplasia with basal pigmentation, overlaid by a naevocellular nevus. Based on their size, three types are distinguished, similar to congenital nevi [3]: small NS (<1.5 cm), medium-sized NS (1.5-19.9 cm), and giant NS (>20 cm). Depending on their topography, a zosteriform type can also be identified, following a dermatomal distribution. Beyond classification by size and topography, Happle delineated two specific types of nevus spilus. The nevus spilus maculosus is a flat lesion featuring dark brown spots over a light brown base. Histologically, this type shows that the underlying pigmentation results from hyperpigmentation in the basal keratinocytes, while the darker spots are attributed to junctional melanocytes organized in nests [4,5]. In contrast, the papular nevus spilus is characterized by dark brown papules or nodules on a light brown background, which may also contain small dark spots. Histopathological examination of this type reveals characteristics of both superficial and deep congenital nevi, with the presence of melanocytes located in both the papillary and reticular dermis [4].
Since its discovery, this lesion has been widely debated, particularly for the possible occurrence of melanoma within the lesion. The first case of degeneration into melanoma was described by Perkinson in 1957 [6]. The precise risk of malignant transformation in NS is not well-defined, but it is believed to be between 0.13% and 0.2%. In cases where melanoma develops, its prognosis and management are similar to those of other types of melanoma. The risk of malignant degeneration within nevi is estimated to range from 0.13% to 0.2%.Nevi acquired in early childhood or congenital nevi, particularly those of the macular type and larger than 4 cm, especially giant and zosteriform variants, appear to be linked to an increased risk [7]. Additionally, the presence of dysplasia in the histology of a nevus constitutes a risk factor for malignant degeneration [7]. Melanoma manifests in approximately 60% of cases on small or medium-sized nevi, with 24% arising on zosteriform nevi and 16% on giant nevi [8,9]. An analysis of the existing literature reveals that the majority of cases involving malignant transformation predominantly occurred in Caucasian and Black patients. These cases had an average age of diagnosis at 49 years, with a female predominance and were more commonly located on the trunk (64%) compared to the limbs (36%) [10]. Melanoma associated with nevi generally manifested as a single tumor; however, there have been reports of multiple melanomas developing from the same nevus in some previous cases. Among the various subtypes, superficial spreading melanoma was the most commonly identified, accounting for 68%, while nodular melanoma and in situ melanoma each represented 16% [7, 8].
At present, there is no standardized method for the management of nevus spilus (NS). It is recommended that patients perform regular self-examinations to detect any changes in their nevi, in conjunction with a structured long-term follow-up that includes dermoscopy or, when available, confocal microscopy [7, 11, 12, 13]. This approach, combined with prudent biopsy of any concerning lesions, could enhance the early detection of melanoma. The literature does not support prophylactic excision of NS in the absence of histological confirmation of dysplasia or malignancy [7]. Conversely, in situations involving dysplasia or malignant melanoma, complete excision of NS is warranted [7, 10].
Due to the location of the lesion in a concealed area of the body, which was inaccessible to visual examination, our patient unfortunately could not detect any changes in her nevus and consequently sought medical advice too late, at a stage of metastasis.
Conclusion:
To clarify the biological behavior of NS and to develop standardized management guidelines, additional research is essential. Enhanced awareness and regular monitoring are vital for early detection and improved outcomes in patients with nevus spilus, particularly those with congenital variants.
Patient Consent Verbal informed consent was obtained from the patient for publication of this case report and accompanying images.
Conflict of Interest
The authors declare no conflict of interest.
Funding
The authors received no financial support for the research, authorship, or publication of this article.