Journal of Dermatology and Venereology
OPEN ACCESS | Volume 4 - Issue 1 - 2026
ISSN No: 3065-677X | Journal DOI: 10.61148/3065-677X/JDV
Belén Burgos Vico*, Claudia García Sierra, Luis Miguel Redondo González
Resident physician in oral and maxilofacial surgery at the Rio Hortega University Hospital in Valladolid, Spain.
*Corresponding author: Belén Burgos Vico, Resident physician in oral and maxilofacial surgery at the Rio Hortega University Hospital in Valladolid, Spain.
Received: October 01, 2025 | Accepted: October 13, 2025 | Published: October 29, 2025
Citation: Belén B Vico, Claudia G Sierra, Redondo González LM., (2025) “Cervical Eccrine Hidradenoma.” Journal of Dermatology and Venereology, 3(2); DOI: 10.61148/3065-677X/JDV/058.
Copyright: © 2025 Belén Burgos Vico. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Eccrine hidradenoma is a rare benign tumor of the skin appendages that most commonly affects women aged 37.2 years and over. It is a slow-growing, solid, asymptomatic tumor that can be confused with other similar entities, so the histology of the specimen is essential to guide the diagnosis. It rarely undergoes malignant transformation, so its only treatment is surgical removal.
This article presents the case of a patient with a tumor in the right mandibular angle that, after removal, turned out to be an eccrine hidradenoma.
eccrine, mandibular, hidradenoma
Eccrine hidradenoma is a rare benign tumor originating from the eccrine sweat glands. Although it is most commonly found on the skin of the head, trunk, and extremities, its occurrence in the cervical region is exceptionally uncommon and presents diagnostic and therapeutic challenges. In the field of oral and maxillofacial surgery, the management of such lesions is particularly significant due to their proximity to vital anatomical structures and their potential to mimic other benign or malignant neoplasms of salivary, cutaneous, or soft tissue origin.
Accurate knowledge of the clinical, histopathological, and imaging characteristics of cervical eccrine hidradenoma is essential to establish an appropriate differential diagnosis and to plan a complete surgical excision, which remains the treatment of choice. However, its rarity means that few cases have been reported in the literature, underscoring the importance of documenting new cases and surgical experiences that can enhance the understanding of this entity.
The present article aims to describe the diagnostic and surgical management of eccrine hidradenoma located in the cervical region,
Clinical Case
We present the case of a 33-year-old male patient referred by his primary care physician for a progressively growing mass at the angle of the right mandible, which had been present for approximately two years. He had not presented any previous infections or symptoms, nor had he suffered from any infectious processes.
On examination, the patient presented a mass at the tail of the right parotid gland, elastic in consistency, painless, and not adherent to any deeper planes. It measured approximately 4 x 3 cm. No cervical lymphadenopathy was palpated. An intraoral examination revealed no significant abnormalities.
After the examination, it was decided to request an imaging test to see the extent of the tumor and a fine needle aspiration (FNA).
The CT scan of the neck with intravenous iodinated contrast revealed an oval image measuring 21 x 16 x 24 mm (AP x T x CC) located in the subcutaneous tissue at the level of the mandibular angle and the tail of the right parotid gland, superficial to the deep cervical fascia. It presented hypodense contents (probably cystic), with a thin, hyperenhancing wall and a small, 7 x 5 mm intraluminal hyperdense image adjacent to its posterolateral wall. The findings were suggestive of a soft tissue tumor, but radiologically nonspecific. No pathologically apparent laterocervical lymphadenopathy was observed.

Imagen 1: coronal CT scan shows a nodule on the right side, superficial to the deep cervical fascia.
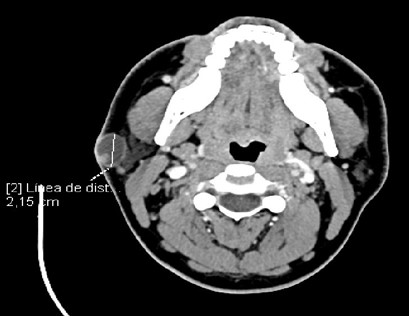
Imagen 2: axial CT scan shows a nodule on the right side at the level of the mandibular angle.
The FNA of the tumor revealed material compatible with cystic contents, negative for malignant cells.
After the tests, it was decided to perform resection of the tumor under local anesthesia and sedation using a submandibular approach and layered dissection. Layered closure was achieved with subcutaneous absorbable sutures and non-absorbable skin sutures.
The sample was sent for histological study, the report of which was: deep dermal cystic formation with a hyperplastic, solid, papillary epithelial lining, composed of small and medium-sized eosinophilic cells, without atypia, and an eccrine phenotype. Focally, a deposit of amorphous eosinophilic material with cellular debris was identified within the lesion. The conclusion was: right submandibular mass consistent with eccrine hidradenoma.
Results.
The patient made a good recovery. He had no bleeding or infection episodes during the postoperative period. He has been followed up with no signs of local or distant recurrence.
Discussion.
Eccrine hidradenoma, also known as nodular hidradenoma, clear cell myoepithelioma, solid cystic hidradenoma, clear cell eccrine sweat gland adenoma, or eccrine acrospiroma (1) is a rare tumor belonging to the family of cutaneous appendage tumors. It is a benign, solitary, asymptomatic, skin-colored tumor arising from the intraepidermal and dermal portion of the internal sweat duct, located primarily in the dermis.
The review by Hernández-Pérez and Cestoni-Parducci showed a mean age of onset of around 37.2 years, with the most common site of presentation being the scalp. The male/female ratio was 1:1.7 (2).
The diagnosis of this type of tumor is histological, consisting of lobulated masses located in the dermis that can extend into the subcutaneous tissue (3). Furthermore, it is usually well-circumscribed and encapsulated, with cystic foci and tubular lumens containing homogeneous eosinophilic material, as seen in our case. The wide variety of cutaneous appendage tumors makes immunohistochemistry essential in many cases to differentiate tumors with ambiguous histopathological characteristics. In the case of eccrine hidradenoma, malignant transformation is rarely observed (4); however, a thorough differential diagnosis is important, as it can be confused with other entities such as lipoma, squamous or basal cell epithelioma, mucous cyst, and so on.
Furthermore, cutaneous appendage tumors may be associated with genetic syndromes such as Birt-Hogg-Dubé, Cowden, and Muir-Torre syndromes, and it is important to rule them out in the case of multiple tumors.
The treatment of this tumor is always surgical, referring the specimen to pathological anatomy for confirmation diagnosis (5).
The interest of this clinical case lies in the rarity of this type of tumor and the limited literature available regarding its diagnosis and management.
Conflicts of Interest.
The authors explicitly declare that there are no conflicts of interest related to the preparation, development, or publication of this article.