Journal of Dermatology and Venereology
OPEN ACCESS | Volume 3 - Issue 1 - 2025
ISSN No: 3065-677X | Journal DOI: 10.61148/3065-677X/JDV
Pacheco-Santiago LD1, Dominguez-Espinosa AE 2, Elizalde Hernández PD3, Erize-Herrera JA4.
1Department of Medicine Internal, Hospital Regional “Lic. Adolfo López Mateos”, Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado, Mexico City, Mexico.
2Department of Dermatology and Dermatopathology, Hospital general de zona 8 "Gilberto Flores Izquierdo" IMSS. Mexico City, Mexico.
3Department of Dermatology. Hospital general de zona y medicina familiar N°1 IMSS Chetumal Quintana Roo, Mexico.
4Department of Dermatology, Hospital Regional “Lic. Adolfo López Mateos”, Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado, Mexico City, Mexico.
*Corresponding author: Pacheco-Santiago LD, Department of Medicine Internal, Hospital Regional “Lic. Adolfo López Mateos”, Instituto de Seguridad y Servicios Sociales de los Trabajadores del Estado, Mexico City, Mexico.
Received: May 22, 2025
Accepted: May 30, 2025
Published: June 03, 2025
Citation: Pacheco-Santiago LD, Dominguez-Espinosa AE, Elizalde Hernández PD, Erize-Herrera JA., (2025) “Cutaneous B-Cell Lymphoid Hyperplasia: Case Report.” Journal of Dermatology and Venereology, 3(1); DOI: 10.61148/3065-677X/JDV/020.
Copyright: © 2025 Pacheco-Santiago LD. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cutaneous benign lymphoid hyperplasia (CBLH) is a benign reactive lymphoid proliferation that may mimic cutaneous B-cell lymphomas, posing a diagnostic challenge to dermatopathologists (1). Clinically, it presents as nodular (2), papular, or plaque-like lesions that are often erythematous in appearance. Histopathological examination typically reveals dense lymphocytic infiltrates with follicular organization and tingible body macrophages. In this article, we present the case of a 41-year-old woman diagnosed with CBLH, describing the clinical presentation, histopathological findings, and a review of the current literature.
B-Cell; lymphomas; dermatology; dermatopatology
Case Report
A 41-year-old woman with no significant medical history presented with a two-and- a-half-month history of a gradually enlarging lesion. The patient was asymptomatic and had not received any prior treatment.
Physical examination revealed localized dermatosis in the left malar region, characterized by an exophytic lesion measuring 1.3 cm in diameter. The lesion was hemispherical and reddish-violaceous in color, with well-defined borders and a shiny surface, and was situated on the basis of diffuse edema.
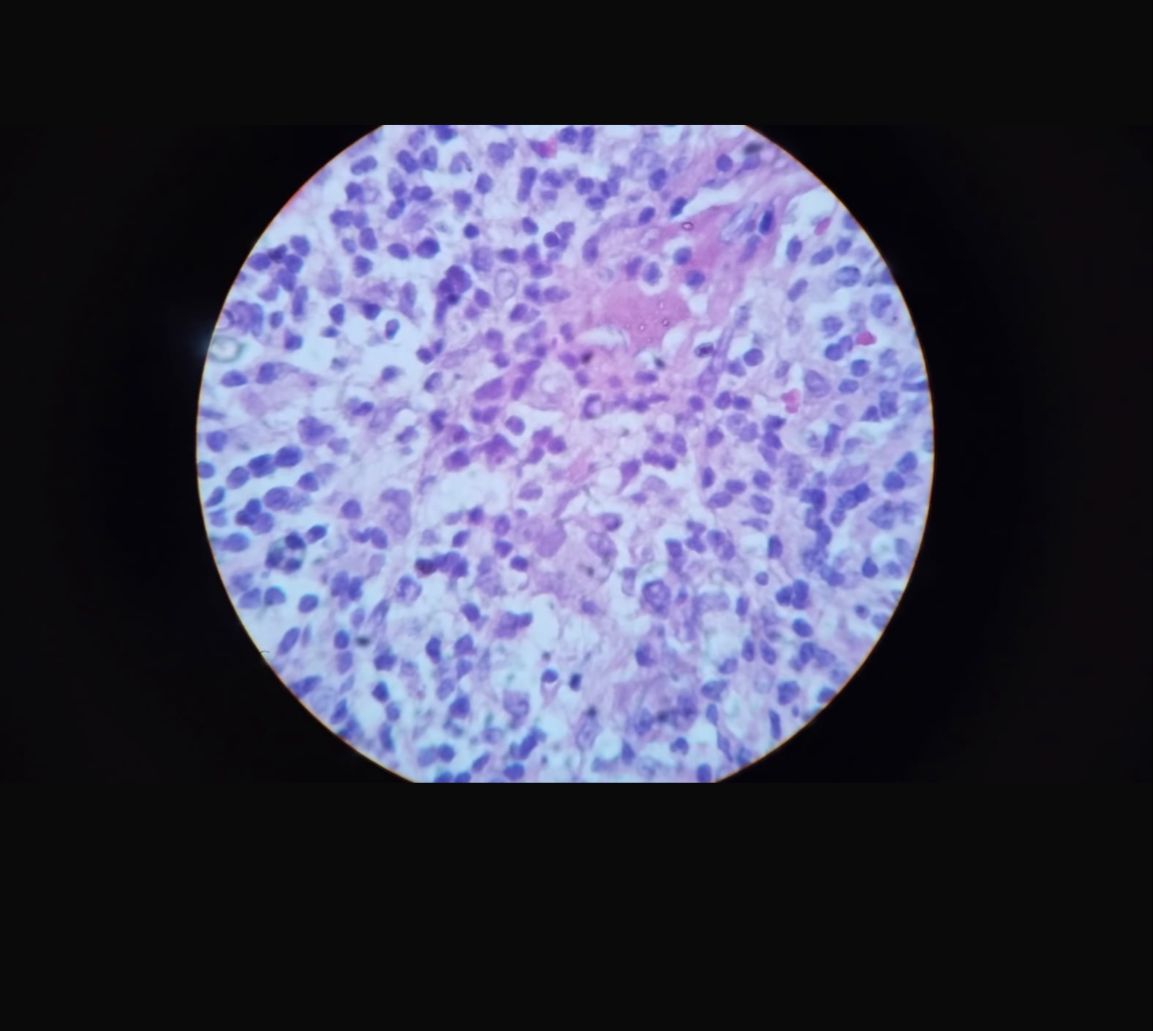
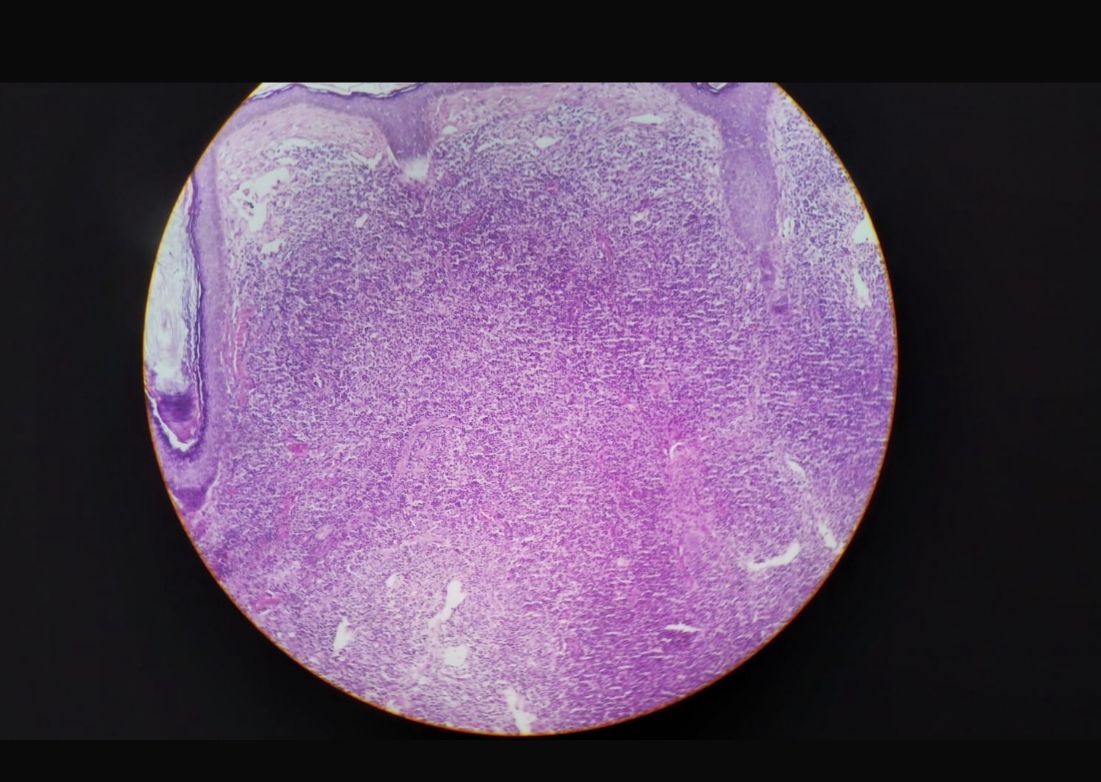
Complete excision of the lesion was performed under clinical suspicion of cutaneous lymphoma. Histopathological analysis revealed a dense dermal lymphocytic infiltrate involving the full thickness of the dermis, with the formation of lymphoid follicles and the presence of “tingible body macrophages.” Small lymphocytes, histiocytes, and plasma cells were also observed. Immunohistochemical staining revealed a polyclonal pattern with positivity for CD20, CD21, and CD23.
Introduction
Cutaneous lymphoid hyperplasia (CLH) is a benign lymphoproliferative disorder that presents as a reactive proliferation of B lymphocytes in the skin. It has been associated with various conditions, including infections, drug reactions, and trauma (3,4).
Although considered a benign entity, the literature describes the potential for malignant transformation in persistent or recurrent cases. Singh et al., for example, documented the progression of CLH to primary cutaneous marginal zone lymphoma in patients with long-term clinical follow-up, highlighting the need for continuous monitoring in atypical cases (5). It has been reported that atypical CLH can evolve into overt lymphoma, underlining the importance of repeated biopsies to assess for signs of malignant transformation (2,6).
On the other hand, some authors suggest that CLH represents an intermediate state, proposing that clonal CLH may have the potential to progress to lymphoma, based on histopathological and genetic studies (7).

Discussion
Cutaneous lymphoid hyperplasia is included among the benign hyperplastic B-cell lymphoid infiltrates of the skin, along with angiolymphoid hyperplasia, Kimura disease, and Castleman disease (8). CBLH, formerly referred to as lymphocytoma cutis, most commonly affects women, with a peak incidence in the fourth decade of life. It typically appears on the head and neck, especially the face, although cases involving the trunk and upper extremities have also been reported. In rare cases, it may involve mucosal sites such as the oral cavity (9).
Clinically, lesions present as nodular, papular, or infiltrated plaque-like growths, ranging from 2 to 5 cm in diameter, with reddish-violaceous to reddish-brown coloration, and a firm consistency on palpation (10,11). In many instances, they may be mistaken for infections, tumors, or inflammatory skin diseases (12).
Risk factors associated with CBLH include prior infections, such as Lyme disease caused by Borrelia burgdorferi, and the use of certain medications, including antidepressants and antihistamines (13,14). There have also been reports of cases following invasive procedures such as vaccinations and minor surgeries (12,15).
CBLH may clinically and histologically mimic cutaneous lymphomas, underscoring the importance of correlating the clinical presentation with histopathological findings. A report by the Society for Hematopathology and the European Association for Haematopathology highlighted multiple cases in which CBLH resembled cutaneous lymphomas, emphasizing the need for detailed immunohistochemical evaluation (16).
Key histopathological features of CBLH include nodular or diffuse B-cell proliferation with a well-defined follicular architecture, networks of follicular dendritic cells positive for CD21 and CD23, and a high proliferative index (elevated Ki-67 in germinal centers) (17). Plasma cells and eosinophils are often found at the periphery of germinal centers, along with “tingible body macrophages”—histiocytes that have phagocytosed cellular debris (18).
Cutaneous marginal zone lymphoma (CMZL) can closely resemble CBLH both clinically and histologically, making differentiation challenging. CBLH represents a benign reactive lymphoid proliferation that may arise in response to chronic antigenic stimulation, such as infections or persistent inflammation. Conversely, CMZL is a low-grade B-cell lymphoma that may also develop following chronic antigenic stimulation (6,19).
Histologically, CMZL is characterized by a diffuse infiltrate of marginal zone cells, Dutcher bodies, and monoclonal expression of immunoglobulin light chains, which are absent in CBLH. Additionally, CMZL may show a dermal or subcutaneous diffuse infiltration pattern and a B:T cell ratio of ≥3:1 on immunohistochemistry, whereas CBLH typically shows a more localized and polyclonal lymphocytic infiltrate (19).
Follicle center lymphoma (FCL) is another important differential diagnosis. It is characterized by atypical neoplastic follicles lacking mantle zones, the absence of polarization, confluence, and absence of tingible body macrophages, which are not typical of benign lymphoid hyperplasia (20).
FCL may also show reduced follicular proliferation (as measured by MIB-1), CD10 and Bcl-6 positivity outside follicles, and Bcl-2 expression within follicular cells, all of which are indicative of malignancy (21,22).
Treatment depends on the disease severity and triggering factors. Topical or intralesional corticosteroids may be sufficient for localized lesons. However, in more extensive or resistant cases, systemic corticosteroids, methotrexate, and hydroxychloroquine have been effective, resulting in lesion reduction within four months and no recurrence after one year of follow-up (7). In persistent or recurrent cases, localized radiotherapy or intralesional rituximab administration have shown efficacy (23).
The prognosis of CBLH is generally favorable, with spontaneous resolution occurring within weeks or months in a minority of cases, and asymptomatic persistence in others. Nonetheless, progression to cutaneous lymphoma has been reported in patients with chronic lymphomas (16).
Conclusion
Cutaneous lymphoid hyperplasia is a dermatosis characterized by reactive infiltration of lymphocytes in the skin. Its differential diagnosis is broad and includes true cutaneous B-cell lymphoma.