International Journal of Medical Case Reports and Medical Research
OPEN ACCESS | Volume 5 - Issue 1 - 2026
ISSN No: 2994-6905 | Journal DOI: 10.61148/2994-6905/IJMCRMR
Shiwei Ren
Orthopedics Department of the 960th Hospital of the Joint Logistics Support Force of the People's Liberation Army of China Shandong Jinan,250031.
*Corresponding author: Zhengqi Chang, Department of Orthopaedics, the 960th Hospital of PLA 25 shifan Road, Tianqiao District, Jinan, Shandong, 250031, China.
Received: January 04, 2026 | Accepted: January 08, 2026 | Published: January 20, 2026
Citation: Ren S, Chang Z., (2026) “A Comparative Study on the Efficacy of Compressed Sponge Versus Ordinary Sponge
in the Treatment of Primary Spinal Infections.” International Journal of Medical Case Reports and Medical Research, 5(1); DOI: 10.61148/2994-6905/IJMCRMR/0176.
Copyright: © 2026 Zhengqi Chang. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Objective: This study aimed to investigate the clinical characteristics and application advantages of compressed sponges in the treatment of primary spinal infections by comparing and analyzing the clinical data of patients treated with compressed sponges versus ordinary sponges.
Methods: A retrospective analysis was conducted on the clinical data of 21 patients diagnosed with primary spinal infection who were admitted to our hospital between July 2019 and June 2024. All patients underwent debridement via an expanded foraminal approach combined with negative pressure wound drainage. Based on the type of sponge used during surgery, patients were divided into a compressed sponge group (n=11) and a regular sponge group (n=10). Baseline demographic and clinical characteristics—including age, body mass index (BMI), and SITE score—as well as preoperative and postoperative Visual Analog Scale (VAS) pain scores, sponge implantation time, intraoperative blood loss, and average daily postoperative drainage volume were recorded and analyzed using appropriate statistical methods.
Results: All 21 patients experienced significant short-term improvement in pain symptoms following surgery. However, compared with the regular sponge group, the compressed sponge group demonstrated significantly shorter sponge implantation time, reduced intraoperative blood loss, and increased average daily postoperative drainage volume, with all differences being statistically significant (P < 0.05).
Conclusion: In the management of primary spinal infections, the use of compressed sponges offers notable clinical advantages over regular sponges, including reduced surgical duration, decreased intraoperative blood loss, and improved postoperative drainage efficiency.
Spinal infection; Expanded foraminal approach; Closed negative pressure drainage; Compressed sponge; Regular sponge; Short-term efficacy
Spinal infectious diseases refer to a series of infectious diseases caused by different pathogenic microorganisms in the vertebral bodies and surrounding soft tissues of the spine and its appendages, accounting for approximately 2% - 7% of all musculoskeletal system infections in the body [1]. In recent years, the incidence of spinal infection has been on an annual upward trend. At present, the incidence of spinal infection is as high as 1/100,000 - 1/200,000 [2].
There are a variety of treatment methods for spinal infections. Surgical treatment is an important measure for treating spinal infections.The traditional lumbar TILF decompression surgery requires extensive dissection of the bilateral paravertebral muscles and removal of the lamina. Postoperatively, complications such as spinal paravertebral muscle atrophy and spinal instability are prone to occur [3], the expansion of intervertebral foramen approach has the advantages of less trauma, less bleeding, and maintaining spinal stability than traditional TILF decompression surgery [4].The expanded intervertebral foramen approach with VSD drainage is a treatment method that involves expanding the intervertebral foramen to thoroughly remove infectious foci within the intervertebral space. Subsequently, a VSD (Vacuum Sealing Drainage) negative-pressure sponge is implanted into the intervertebral space through the expanded foramen. This creates a continuous negative-pressure suction force around the infectious foci in the spinal intervertebral space, and exudate, necrotic tissue, and bacteria are suctioned out of the body via the closed negative-pressure drainage system [5]. Currently, studies have shown that continuous VSD negative pressure drainage can disrupt the growth environment of bacteria in the body and reduce local edema and bacterial load [6]. Negative pressure drainage of VSD has been successfully applied in the treatment of spinal infections [7]. For the traditional VSD negative pressure sponge, due to its large size, it needs to be carefully trimmed and molded multiple times during the implantation process, which leads to an increase in the operation time and the amount of bleeding. Based on this, our department has innovatively adopted compressed VSD negative-pressure sponges: the traditional VSD negative-pressure sponges are compressed into cylindrical shapes with a diameter of approximately 1 cm, making it easy and convenient to implant into the intervertebral space by expanding the intervertebral foramen. This study retrospectively analyzed the clinical data of 21 cases of spinal infection treated with compressed negative pressure sponges and ordinary negative pressure sponges, and is reported as follows.
Materials and Methods
Inclusion and Exclusion Criteria
Inclusion Criteria: (1) Patients diagnosed with a single-segment thoracolumbar intervertebral space infection, confirmed through clinical manifestations, laboratory findings, and imaging examinations; (2) Presence of epidural or paravertebral abscess formation; (3) Failure of conservative management with antibiotic therapy.
Exclusion Criteria: (1) Involvement of two or more mobile spinal segments by the infectious lesion; (2) Patients with severe comorbidities rendering them unable to tolerate general anesthesia or the prone position; (3) Incomplete medical records or loss to follow-up.
General Information
A retrospective analysis was conducted on patients who were admitted to our department from July 2019 to June 2024 and diagnosed with spinal infection by imaging examinations or bacterial culture. All patients underwent expanded intervertebral foramen approach combined with vacuum sealing drainage (VSD)surgery, and were divided into two groups according to the different methods of implanting negative-pressure sponges during the operation: the compressed sponge group (11 cases) and the conventional sponge group (10 cases). The baseline data of the two groups of patients on admission were as follows: In the compressed sponge group, the average age was 58.90±10.19 years, and the average body mass index (BMI) was 23.74±4.16 kg/m²; in the conventional sponge group, the average age was 61.45±11.68 years, and the average BMI was 23.34±3.72 kg/m². Regarding the Spinal Infection Treatment Evaluation (SITE) score: the compressed sponge group had a score of 6.40±1.17, while the conventional sponge group had a score of 6.45±1.57. Statistical analysis showed that there were no statistically significant differences in the above baseline indicators between the two groups (P>0.05). In terms of the Visual Analogue Scale (VAS) score: The pre-operative and post-operative VAS scores of the compressed sponge group were 6.50±0.85 and 2.80±0.79, respectively; The pre-operative and post-operative VAS scores of the conventional sponge group were 6.54±1.04 and 2.64±0.67, respectively. Statistical comparison revealed no significant differences in the pre-operative and post-operative VAS scores between the two groups (P>0.05).
Table 1: Comparison Table of Data for Two Groups of Patients
|
Parameter |
Compressed sponge group |
Ordinary sponge group |
Statistic (Z) |
P value |
|
Age (years) |
58.90±10.19 |
61.45±11.68 |
-0.531 |
0.601 |
|
BMI (kg/m²) |
23.74±4.16 |
23.34±3.72 |
-0.07 |
0.944 |
|
SITE (points) |
6.40±1.17 |
6.45±1.57 |
-0.182 |
0.855 |
|
Preoperative VAS (points) |
6.50±0.85 |
6.54±1.04 |
-0.109 |
0.914 |
|
Postoperative VAS (points) |
2.80±0.79 |
2.64±0.67 |
-0.461 |
0.645 |
|
Implantation time (min) |
6.55±1.51 |
20.60±2.55 |
-3.866 |
0.001 |
|
Intraoperative blood loss (mL |
77.27±4.34 |
113.20±3.67 |
-3.874 |
0.001 |
|
Postoperative drainage volume (mL |
65.09±3.02 |
54.30±2.83 |
-3.879 |
0.00 |
Surgical methods
Both groups of patients underwent surgery via the expanded intervertebral foramen approach. Abscesses, granulation tissue, and necrotic discs were completely removed with scrapers, reamers, and spatulas. After cleaning, negative pressure sponges were implanted.
Compressed sponge group: The diameter of the compressed sponge was fixed at 1 cm. According to the height of the intervertebral space measured after debridement, the sponge was trimmed to an appropriate length, implanted into the intervertebral space, and fixed. A biological semipermeable membrane was used to quickly cover the surface sponge over the wound and the surrounding skin tissue. A negative-pressure drainage system was immediately established, with the negative pressure maintained at 125 mmHg (1 mmHg = 0.133 kPa) [8] (Figure 1-A).
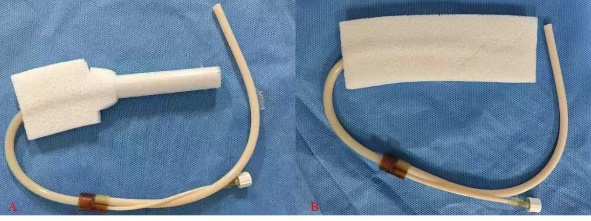
Ordinary Sponge Group: The size of the traditional VSD (Vacuum Sealing Drainage) sponge was approximately 10 cm × 15 cm × 1 cm. Based on the diameter of the intervertebral foramen and the height of the intervertebral space measured after debridement, the sponge was trimmed to an appropriate size. After gentle retraction and protection of the nerve roots, the sponge was carefully inserted into the intervertebral space using long forceps and subsequently sutured securely to the wound margin. A biological semipermeable membrane was used to quickly cover the surface sponge over the wound and the surrounding skin tissue. A negative-pressure drainage system was immediately established, with the negative pressure maintained at 125 mmHg (1 mmHg = 0.133 kPa) (Figure 1-B).
Evaluation Indicators
The duration of sponge implantation into the intervertebral space during surgery, intraoperative blood loss, and the mean daily drainage volume on postoperative day 3 were compared between the two groups, with statistical analysis performed accordingly.
Statistical Methods
Statistical analysis was performed using SPSS 22.0 software. Measurement data were expressed as mean ± standard deviation (x±s). When the data followed a normal distribution, the independent samples t-test was used for comparison between the two groups; when the data showed a non-normal distribution, the rank-sum test was applied. Enumeration data were tested using the chi-square test (χ² test) or Fisher's exact probability test. A P-value less than 0.05 (P<0.05) was considered statistically significant.
Results
Both groups of patients successfully underwent the surgical procedures without complications. A comparative analysis of perioperative outcomes revealed that the mean implantation time in the compressed sponge group was 6.55 ± 1.51 minutes, significantly shorter than the 20.6 ± 2.55 minutes observed in the conventional sponge group. Intraoperative blood loss was also markedly lower in the compressed sponge group (77.27 ± 4.34 mL) compared to the conventional sponge group (113.2 ± 3.67 mL). With regard to postoperative drainage, the compressed sponge group exhibited a higher mean drainage volume (65.09±3.02 mL) than the conventional sponge group (54.3±2.83 mL), indicating more effective fluid clearance. Statistical analysis demonstrated that the differences in implantation time, intraoperative blood loss, and postoperative drainage volume between the two groups were all statistically significant (P < 0.001). Detailed results are presented in Table 1. These findings suggest that the use of compressed sponges is associated with reduced operative duration, decreased intraoperative bleeding, and improved postoperative drainage compared to conventional sponges.
Discussion
In the surgical management of spinal infections, multiple operative approaches are available. The conventional posterior decompression combined with debridement typically involves a single posterior approach to resect the ipsilateral lamina, facet joint, or costotransverse joint, along with a segment of adjacent rib, and occasionally the spinous process when necessary [3]. This strategy aims to preserve the integrity of the ipsilateral pedicle and contralateral facet joints as well as partial lamina, thereby minimizing disruption to spinal stability [9–11]. The expanded intervertebral foramen approach necessitates removal of only a portion of the lamina and facet joint, while preserving the ipsilateral pedicle along with the majority of the lamina and facet joints. This technique involves less dissection of surrounding soft tissues, offering the advantages of reduced trauma, minimized bleeding, and better preservation of lumbar facet joint stability [4, 12, 13]. The expanded intervertebral foramen approach achieves comparable decompression to conventional TILF surgery, enables thorough debridement of infected lesions, and simultaneously minimizes iatrogenic tissue damage while mitigating the risk of infection dissemination.
Vacuum sealing drainage (VSD) technology has matured significantly in managing spinal infections. Clinical studies confirm that VSD-generated negative pressure effectively reduces local bacterial load, resolves interstitial edema, enhances blood perfusion, and promotes cellular proliferation with granulation tissue formation. This approach improves perioperative infection control safety and efficacy while minimizing iatrogenic impact on neural structures, dura mater, and vasculature. For primary spinal infections, negative pressure suction devices demonstrate superior short-term clinical outcomes compared to conventional surgery [14-17].Regarding negative pressure sponge implantation, traditional methods position the sponge superficially to the deep fascial layer. Although distanced from nerve roots for enhanced safety, this technique fails to deliver negative pressure directly to intervertebral lesions, resulting in inadequate drainage and prolonged treatment cycles [18, 19]. Xing Hao et al. demonstrated that transforaminal implantation of the sponge into the intervertebral space enables immediate aspiration of exudates, necrotic debris, and pathogens. This disrupts bacterial microenvironments, accelerates granulation tissue development, and significantly shortens spinal infection treatment duration [20].
Comparative analysis of compressed versus conventional sponges in expanded intervertebral foramen approach surgeries demonstrated significant advantages of compressed sponges in reducing operative duration, minimizing intraoperative blood loss, and achieving optimal postoperative drainage efficacy. No statistically significant intergroup differences were observed in perioperative complication rates. These findings indicate that compressed sponges offer enhanced clinical utility and greater practical adoption potential in spinal surgical workflows.
Comparative analysis of compressed versus conventional sponges demonstrated significant advantages of compressed sponges in reducing operative duration, minimizing intraoperative blood loss, achieving effective postoperative drainage, and decreasing surgical trauma. As a retrospective case-control study with limited sample size, these findings necessitate further validation through large-scale, multicenter randomized controlled trials with medium-to-long-term follow-up.
Conflict of Interest
The authors declare no competing financial or non-financial interests relevant to this work.
Author Contributions
Shiwei Ren:Conceptualized the study design; conducted data collection and curation; prepared the original draft. Zhengqi Chang: Acquired funding resources; performed surgical interventions and clinical validation; supervised manuscript preparation and critical revision.
Funding
This research was supported by Natural Science Foundation of Shandong Province (Award Number: ZR2023MH331; Grant Recipient: Zhengqi Chang).