International Journal of Medical Case Reports and Medical Research
OPEN ACCESS | Volume 5 - Issue 1 - 2026
ISSN No: 2994-6905 | Journal DOI: 10.61148/2994-6905/IJMCRMR
Hassan A Saad*, Mohamed Riad, Rasha S Elsayed, Mohamed E Eraky, Ahmed K El-taher Ashraf
Abdelmonem Elsayed University
*Corresponding Author: Hassan A Saad. Abdelmonem Elsayed University..
Received Date: March 19, 2023
Accepted Date: July 05, 2023
Published Date: July 22, 2023
Citation: Hassan A Saad, Mohamed Riad, Rasha S Elsayed, Mohamed E Eraky, Ahmed K El-taher Ashraf. (2023) “Retrospective study on the predictive survival variables and therapeutic response in differentiated thyroid cancer.”, International Journal of Medical Case Reports and Medical Research, 1(1); DOI: 10.61148/2994-6905/IJMCRMR/006.
Copyright: © 2023. Hassan A Saad. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly Cited.
Introduction: The most established endocrine problems are thyroid cancer. Differentiated thyroid cancers (DTCs) usually come in papillary and follicular forms [1]. Thyroid cancers are now more time-honored than ever, accounting for 1% of all cancer instances recognized yearly [2]. Follicular kinds have a better impact than aggressive anaplastic types, while follicular types have a higher outlook than papillary types.
Objective: How long-term survival for patients with unique thyroid carcinomas is predicted to be? Age, sex, bulk size, participation of lymph nodes, far away organ metastasis, surgical intervention, and differentiation
Methods: At the medical institution of Zagazig University, the surgical department, 123 patients obtained thyroid surgical process for differentiated carcinoma between 2018 and 2022. (96 for papillary sort most cancers and 27 for follicular kind cancer). Post-operative mortality, histopathology findings (multifocality and differentiation), local and distal lymphatic invasion,
Results: Follow-up At the surgical branch of the Zagzig University, ninety-six sufferers with papillary cancer underwent surgery; the typical patient age was once 43.7 /-16.0 years, and the male to girl ratio used to be 1:7. The 5-year mortality price after follow-up used to be 90.9% for papillary forms and 84.0% for follicular types, respectively. The average follow-up period was once 4.6 /- 4.9 years. Twenty-seven instances (average age: 49.5 /- 15.9 years, males: 7, females: 20,
male to girl ratio: 0.35%) underwent follicular carcinoma surgery.
Conclusions: Age type of pathological character of thyroid tumor affecting the survival of patients
Introduction and objectives:
The most acquainted endocrine illness is thyroid cancer. Differentiated thyroid cancers (DTCs) mainly come in papillary and follicular varieties [3]. Thyroid cancer is now prevalent for 1% of all cancer cases observed yearly, making it more frequent than ever [4]. The prognosis is higher for papillary varieties than follicular types, and it is more significant for follicular types than aggressive anaplastic types. Because of early prognosis and chemo-radiation treatments, lifespans have accelerated over the final 15 years [5]. Thyroid nodules are about four times greater common in girls than in men. In contrast, the median age is 47 years old, and every guys and women's well-known heights vary from sixty to sixty-ninety-nine years hhistorically[6].
Papillary carcinoma is the most frequent type of thyroid cancer, accounting for 65–80% of all thyroid malignancies. New nodules enhance at a fee of about 0.1% per yr when they first show; conversely, after publicity to head and neck radiation, they advance at a heap's quicker price (* 2% per year) [7].
The debate about the severity of ailments has been documented by way of long-term survival regardless of repeated illness. While hemithyroidectomy is a surgical desire for papillary and medullary carcinomas, it is additionally a surgical opportunity for follicular and hurtle mobile neoplasms. Patients with papillary, follicular, and Hurthle cellular carcinomas had 10-year relative mortality expenses of 93%, 85%, and 76%, respectively [8]. Early bleeding and recurrent nerve affection had been two of the surgery's complications; on the other hand, the recurrence—a hassle that happens less regularly with incomplete excision but more regularly with recurrent reoperation—was the most serious. [7]Total thyroidectomy is the most radical procedure for all sufferers because, primarily based on the final histology, it frequently indicates thyroid cancer, which is usually silent and no longer clinically ubuntupuntilntilre genuinely about to complete the operation.[9] Differentiated thyroid carcinoma (DTC) desires long-term follow-up after excision for explanations of residing quality, public health, and the propensity for recurrence. The outstanding existence of people with thyroid cancer is impacted by hypothyreosis, which has a one-month latency halt. Identify the kind of affected character, especially primarily based on the information, prognostic variables, and postoperative restoration period.[10]
Determining a long survival length will require consideration of the cases existing at the moment of treattreatingatingthe hazard of dying. In addition to the points of the tumor and the TNM categorization, a range of specific elements additionally affect survival. They have an impact on a range of factors, such as the form of surgery, the patient's immune system, the tumor's unresolved relationship with lymphocytic infiltration, and the patient's follow-up care for iodine deficiency and ionization, which have been seemed at the use of a variety of techniques, used to be as soon as examined via lookup organizations from the United States and Europe.[11]
People living with Cancer often speak about their favor of dying in the path of their first workplace visit. Therefore, it is critical to classify matters precisely to predict cancer-specific death. PTC and one-of-a-kind stable tumors are, in many instances, staged using the TNM (tumor, node, and metastasis) staging method developed through the American Joint Committee on Cancer (AJCC). This staging approach divides the tumor size into age classes and bills for the pprimaryimaryttumor'slloss-by, metastatic lymph nodes, and far-off metastases. In tumor registries around the world, the AJCC/TNM device is commonly used and performs nicely in the assessment of distinctive staging categories. [12] A few modifications in the most cutting-edge AJCC eighth model are supposed to amplify the accuracy of the disease-specific mortality prediction.[13]
It is fundamental to recognize three key differences. First, the diagnostic cutoff age increased from below forty-forty-five to fifty-five. This shift was supported by a global multicenter learn about involving nearly 10,000 patients, proving that sufferers older than 55 havlanguishinguishing between these levels III and IV disease. [14], so we selected patients below 40 years old. The minor extrathyroidal extension (mETE), also known as asymptomatic peri thyroidal invasion, has poor TThey they are not solely considered, ing whichwabecbecomebetobe also be reevaluated in the AJCC eighth version. (i.e., no longer visible on intraoperative view or imaging assessment). The previous AJCC 7th version labeled any tumor containing mETE as T3. [15]
Survival is, on the other hand, attainable despite conflicting debts involving its act on ongoing or relapsing sickness in the thyroid mattress or cervical lymph nodes. Due to these factors, the AJCC eighth model has divided the T3 classification into two categories: T3b for tumors with ETE, which is referred to as gross encroachment of the strap muscle, and T3a for umors more significant than 4 cm that are constrained to the thyroid gland. [16]
The Aim:
A- What is the prognostic determinant of papillary and follicular carcinoma growth survival?
B-Attributes of the patient and a tumor, obligatory surgical treatment techniques, the affordability of iodine, and prognostic variables.
C- response to different management
Methods:
Between 2018 and 2022, 123 sufferers acquired differentiated thyroid carcinoma surgical methods at the Zagzig University surgical department. 69 for papillary carcinoma and 27 for follicular carcinoma).average age: 43.7 /-16.0 years, male: 17, female: 79, male: woman ratio: 1:7). For papillary and follicular types, the 5-year mortality charge after follow-up was once as quickly as 90.9% and 84.0%, respectively and the follow-up time used to be on familiar 4.6 /- 4.9 years. Follicular carcinoma surgical operation used to be carried out on 27 men and women (average age: 49.5 /- 15.9 years, males: 7, females: 20). We totaled the data for 123 sufferers and brought the consequences of our retrospective research. Survival is influenced by the post-operative and working follow-up chart as accurately as the patients' connection for follow-up. Histology the specimens and findings for differentiated tumor types, lymph node affection distal spread, a couple of focality age considerable than forty years, and iodine supply also habits and in addition to discovering out the examples of approaches that might moreover prefer iodin 131 post-operatively include thyroidectomy, either total thyroidectomy or partial thyroidectomy ( lobectomy or near total). However, sufferers of the 1/3 form depart more thyroid tissue behind. Results of iodine consumption with or without radiotherapy
Exclusion and inclusion criteria:
All patients included in our study.
1-Except late metastic cases that already survival measurment has no role
1- non differentiated type of throid cancer
Surgical Treatment:
thyroid lobectomy versus total thyroidectomy:
The opportunity of thyroid cancer mortality or thyroid most cancers recurrence is unaffected by way of the preference between near total thyroidectomy NTT and total thyroidectomy TT (with or barring RAI therapy). A reliable study shows that after NTT, those with low-risk disorders can safely view the contralateral lobe. [17-18].
Indications for lobectomy versus total thyroidectomy:
For treating T1 and T2 tumors that are constrained to the thyroid because the amount of thyroidectomy has no bearing on DTC survival (39) .and, that recovery from recurrence following lobectomy is possible with no negative consequences for typical longevity. Still, theBut the total thyroidectomy must band e in T3, a T4 with risk of recurrent laryngeal nerve injury and parathyroid removal.
Treatment with Radioactive Iodine;
Only patients receiving TT and working towards the following objectives [21] should be given postoperative RAI consideration.
Results:
Follow-up At the surgical department of Zagazig University, ninety-six cases with papillary carcinoma acquired surgical remedy (average age: 43.7 /-16.0 years, male: 17, female: 79, male: woman ratio: 1:7). For papillary and follicular types, the 5-year mortality charge after follow-up was once as quickly as 90.9% and 84.0%, respectively and the follow-up time used to be on familiar 4.6 /- 4.9 years. Follicular carcinoma surgical operation used to be carried out on 27 men and women (average age: 49.5 /- 15.9 years, males: 7, females: 20). Enhanced CT is used for diagnosis of exiting malignant tumors that can differentiate between benign and malignant mass but can't differentiate between types of malignancy that done only after ct guided, or we guided accurate cut neThe figureiopsy. Figure, as a result, believes that patients ought to think about whether NTT has been positioned to exist. Patients' protection protocol from recurring against types of operation and techniques still disparity with some surgeons from recurrent laryngeal, parathyroid affection and hormonal depending after total thyroidectomy that protected in lobectomy or NTT near-total thyroidectomy, recurrent laryngeal nerve affection highly affected after recurrent thyroidectomy or even after total thyroidectomy, that difficult identified in the vicinity of the operative field figure 3 [22-23].Table 1

Figure 1: CT enhanced present thyroid carcinoma
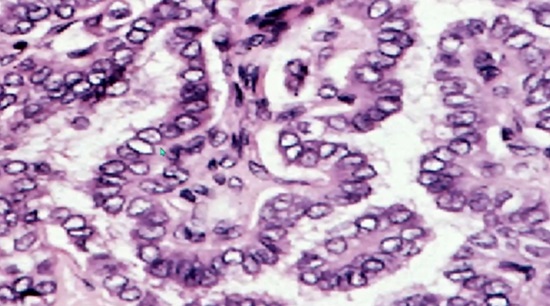
Figure 2: showing papillary thyroid cancer with loss of nuclei
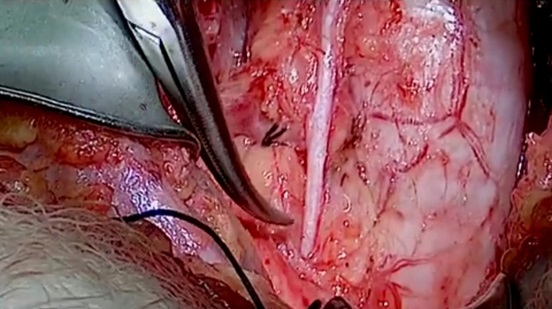
Figure 3: showing lt. Laryngeallaryngeal nerve.
|
Adaptation to Therapy |
Suggest the next steps follow |
|
Outstanding Response |
Early reduction in follow-up intensity, regularity, and TSH suppression level |
|
Intermediate and low hazards
|
Every 12–24 months, non-stimulated Tg and TgAb should be considered; if the results are negative, no further imaging is required. |
|
Uncertain Response |
Reduced follow-up intensity, regularity, and TSH suppression degree Active monitoring sequential imaging of vague tumors; Tg and TgAb without stimulation every 12 to 24 months |
|
defective biochemical
Structural Incomplete
|
Response TSH levels should be comparable to the Tg curve. Active surveillance means Tg levels that are stable or dropping every 6 to 12 months, non-stimulated Tg and TgAb, stimulated Tg if clinically necessary, and a 12-month neck ultrasound. Reduction of TSH (mild)Increased amounts of Tg or TgAb = More research individual strategy using hybrid, functional, or anatomical imaging. Reduction of TSH
Response Consider the actionable and non-actionable structural signs of disease when using an individualized strategy. Reduction of TSH
|
Table 1: shows follow-up tactics depending on how well the initial therapies worked.
|
Gender 0.28- 0.20 |
|
Age <0.0001 - 0.046 |
|
Size 0.48 0.20 |
|
T1-2-3-4 <0.0001 <0.0001 |
|
Distal spread <0.0001 <0.0001 |
|
Nodal positive 0.01 0.046 |
|
invasion 0.37 0.29 |
|
Surgery technique 0.47 0.11 |
|
Multiple facilities 0.47 0.6 |
|
Capsule invasion 0.05 0.08 |
|
Iodine 0.66 0.7 |
|
Gender - sex of patient; Age – age of patient over 40; |
Table 2: Survival factors of papillary and follicular cancer patients (Kaplan Meier curves - p-value) Papillary cancer Follicular cancer)
|
|
Papillary cc. |
Follicular cc. |
|
The age/years of patients 40< |
0.002 |
0.011 |
|
size of tumor |
<0.0001 |
0.003 |
|
Distal spread |
<0.0001 |
<0.0001 |
|
Nodal positive |
<0.0001 |
0.171 |
Table 3: Prognostic risk factors: Cox regression analysis (p)
|
Byar study(1979) All 507 Μ Μ Μ |
|
Cady results(1988) DTC 755 Μ Μ Μ |
|
Sanders outcome(1998) DTC 1019 Μ Μ Μ n.s. n.s. |
|
Mazzaferri study(1994) DTC 1355 Μ Μ Μ Μ Μ Μ Μ |
|
Sellers study (1992) DTC 212 n.s. Μ n.s. Μ Μ n.s. n.s. |
|
Simpson results(1987) PTC 1074 n.s. n.s. Μ n.s. n.s. n.s. n.s. |
|
Hay outcome (1987) PTC 860 n.s. Μ Μ Μ n.s. n.s. |
|
Hay outcome(1993) PTC 1779 n.s. Μ Μ Μ n.s. n.s. n.s. Μ |
|
Akslen study(1993) PTC 173 Μ n.s. n.s. n.s. n.s. n.s. n.s. n.s. |
|
Kashima (study1998) PTC 1533 n.s. n.s. n.s. Μ n.s. Μ |
|
Present our study PTC 386 n.s. n.s. Μ Μ Μ n.s. n.s. n.s. n.s. |
|
Simpson study (1987) FTC 504 n.s. Μ Μ Μ Μ Μ |
|
Mueller-G.study outcome (1990) FTC 149 n.s. n.s. Μ n.s. |
|
Shaha study(1995) FTC 228 n.s. Μ Μ Μ n.s. |
|
Present our study FTC 106 n.s. n.s. Μ Μ n.s. n.s. n.s. n.s. n.s. |
Table 4: Prognostic factors influencing survival Author Type N Gender Size pT4. Met. Node. Ulti. Infiltrate. Surg. Iodine
|
Benefits of a thyroid lobectomy over a complete thyroidectomy
|
disadvantages of partial thyroidectomy versus lobectomy |
|
reducing surgical dangers to enhance |
Surgical finish prognosis and radioactive iodine administration risk
|
|
Supplementing with thyroid hormone may not be required. |
Patients with thyroiditis or only a tiny amount of tissue may still need thyroid hormone supplements. |
|
similar longevity |
No indication of a rise in quality of life
|
|
If completion surgery is required, neither the surgical risk nor the result is changed. |
NSuitableble for patients with moderate and intermediate risks. Thyroglobulin may not be suitable for further testing. |
|
|
|
Table 5; lists the benefits and drawbacks of partial thyroidectomy versus total thyroidectomy.
|
Responsive |
Definition |
|
|
Outstanding Response |
There are no structural, biochemical, or clinical signs of an illness. |
Negative imaging with Nonstimulated Tg 0.2 ng/mL and Stimulated Tg 1 ng/mL plus Undetectable TgAb
|
|
Uncertain Response |
Biochemical or structural anomalies that are not specific enough to be reliably classified as benign or malignant |
Negative imaging with nonstimulated Tg 0.2 ng/mL and stimulated Tg 1 ng/mL plus undetectable TgAb |
|
Biochemical Incomplete Response readings over time at constant or increasing TSH levels
|
Absence of a localizable structural illness but abnormally elevated serum Tg and rising Tg TgAb levels |
Nonstimulated 0.2-1 ng/mL, Stimulated Tg 1-10 ng/mL, Stable or Declining TgAb values, and Unspecific MRI study results |
|
Incompletely structural tumors |
Response persistent or recently discovered, remote or local, and with or without abnormal Tg or TgAb |
Whether in anatomical (US, CT), functional (WBS), or hybrid (18FDG-PT/CT) imaging, structural evidence of illness |
Table 6: Risk stratification determined by treatment reaction 6–24 months after the first round of therapy (total thyroidectomy plus RAI)
Adapted from: Haugen and Cols. [2]Tuttle and Cols. [18] Momesso DP and cols.[ 22]
Tg: thyroglobulin; TgAb: thyroglobulin antibodies.
A thyroid hormone alternative is no longer necessary because thyroid tissue is preserved in PT. Outcome—outcomes In addition to a heightened strain on the body and mind, hypothyroidism may have a significant socioeconomic impact on the structure of early retirement or income loss. [24-25] Even after a lobectomy, many people, on the other hand, require hormone choice therapy, and 50% of human beings who endure hemithyroid surgery run the hazard of growing hypothyroidism [26].
Tg ranges may additionally also be much less complex to measure after TT. [27]
Response Strategies:
Long-term follow-up in DTC is essential to identify health issue recurrence in patients declared disease-free and disease improvement in patients with chronic conditions. A second goal is to accomplish control the side consequences of the preliminary therapy, such as hypothyroidism and hypoparathyroidism. As used to be already stated, the hazard of disease persistence or recurrence in LRPTC is relatively lw, and lowered individual follow-up depends upon the surgical manner and whether or no longer RAisasemployed. [29]. Patients on AS, as used to be previously stated, have a particular follow-up protocol.
Initial hazard of a continual or recurrent illness based on the patient's response to remedy 6–18 months after the unique treatment, follow-up techniques ought to be sophisticated. It ought to, more often than not, be predicated on Tg level, TgAb detection, and imaging results.
(stratifying threats dynamically). If the imaging scan reveals significant tumor foci, the patient's therapeutic reaction is classified as structurally incomplete.
The treatment reaction is instead classified as exceptionally good if Tg and TgAb levels are undetectable, indeterminate if blood Tg tiers are low, or biochemically incomplete if Tg tiers are high if the imaging check is negative. (Table 3). [30-31]
Followed up:
Following the whole thyroidectomy with or without radioiodine, Tg and TgAb tiers usually are the fundamental elements to consign response toe to the initial remedy and the follow-up after TT. According to RAI therapy, the metrics used to measure a patient's response to cure change. (Table 6).
Analysis of survival information:
I am using the Kaplan-Meier method, which takes into account tumor-specific death. Cox regression is used to analyze data. SPSS for Windows used to be as quickly used for statistical study. We in distinction the frequency and a while related with tumors of all varieties from a histological standpoint at some stage in two remarkable periods of TNM staging and operation method types.
According to the Kaplan-Meier survival curves, factors that have a terrible impact on sturdiness consist of age over 40, lalongomalongtastases, distal thyroidal invasion, lymph node invasion, and capsule infiltration. Survival was unaffected via multifocality, sex, the diploma of thyroidectomy (total or near-total vs. a lot less than near-total), or lymphocytic involvement. (Table 2).
Staging T4 tumors, which locally amplify spherical the thyroid gland, have decreased survival fees than T1, T2, or T3 stage tumors, which can be both papillary or follicular. Typically, sufferers with stage T4 tumors entirely require hospice procedures. There is no discernible version in the survival of stage T1, T2, and T3 cases. At the time of early diagnosis, 3 (0,035%) people with papillary carcinomas and 1 (0.037%) with the follicular crew had far-off metastases. Each cohort's sufferers passed away during the follow-up time: remote metastases and awful survivability in each category, according to Cox regression analysis (p), age, tumor size, distance friendly social ablbedspreadfect the prognosis of dddiffedifferentiateddthyroid carcinoma.
The result used to be marginally amended in each instance with the aid of lymphocytic infiltration, on the other hand, now, not significantly.
Discussion:
DTC instances have grown to be more rearrangements in PTCs established via radiation have been identified [32]. Two unique studied hazard variables are elongated standing goiter and family history. Chromosome loss or aneuploidy has been located in 10% of all papillary carcinomas and, more dominant recently, in 25–50% of all sufferers who leave out away as a remaining result of these lesions [17). Papillary kind is proximately perpetually linked with BRAF V600E mutation positivity [33]. The prognosis is significantly much less genuinely subsidiary for males, but the difference is customarily negligible. Gender used to be an impartial prognostic component for longevity; according to some sources,s the jeopardy of demise from most cancers was once roughly twice as immoderate for grownup adult males as it used to be for girls [34]. Albeit there is the same hazard of long-term survival for teenagers with thyroid carcinoma (80% at 20 years), the standardized mortality ratio is plenty more preponderant than prognosticated [34]. Up to 10% of differentiated thyroid carcinomas can invade the gland/lymph nodeand 's outer toughen-hen into the close with the avail of tissues, developing morbidity and mortality. As many as one-third of patients with domestically invasive tumors omit away from most cancers internal ten years, and recurrence fees are two cases more dominant [35]. One unearth information regarding determined nodal metastases
found in 36% of 8029 adults with papillary carcinoma, 17% of 1540 victims with follicular carcinoma, and up to 80% of youngsters with papillary carcinoma.[36]
An enlarged cervical lymph node can, moreover, b,e the definite signal of
thyroid carcinoma. In these patients, more than one nodal m case is typically placed at the surgical method [37-38]. Virtually 10% of victims with papillary carcinoma and up to 25% with far-off tumors embellished with follicular carcinoma. At the time of diagnosis, these metastases are conspicuous in about 50% of cases [39]. In 13 searches involving 1231 patients, the following have been the areas cited as a long way away metastases: lung (49%), bone (25%), every single lung and bone (15%), central worried machine (CNS) or unique remote tissues (10%) [40]. Patient age is one of the essential designators of the remaining result for patients with some distance awayAndtastases. And the tumor's metastatic location, its faculty to aurally perceive 131I, its appearance on a chest radiograph, its endured enhancement after one (131) I therapy, its age ameliorated than 45, and its gender in cases of follicular cancer [41]. The expeditious arm of chromosome eleven (11p) is misplaced as follicular adenomas progress, and effacements of the genes 3p, 7q, and 22q emerge to be concerned with the shift to follicular carcinoma [20]. RAS mutations or PAX8/peroxisome proliferator-activated (PPARc) rearrangements are current in follicular thyroid cancers[42].
Other than TNM relegation, different variables, such as tumor size, lymph node metastases, and far-off metastases, have an iimpactnosionof two sorts of differentiated thyroid cancer [43].
According to the findings of retrospective research, one-of-a-kind scoring structures have been developed. Table 4 compares statistics key authors believed to be impessentialements affecting their survival. In our cull, the two sublime varieties of differentiated carcinomas have been examined,exa the ned with and avail of one as having unique natural deportment. In the PTC and FTC groups, age is the quintessential prognostic quandary during early diagnosis. After age 40, mortality and recurrence quotes ascend; alternatively, older cases experience early recurrences and die after recurrences, which endorse expeditious mitosis and histological changes. The consequential and secondary tumors have a minimized uptake of the isotope 131I. Our findings show that papillary carcinomas were more hooked up and manifested themselves in the anterior than mundane, all via the length of our research. Widespread use more immensely colossal the diagnostic outcome.
All types of thyroid cancer; differentiated thyroid cancer; follicular cancer; infiltrate -- the presence of lymphocytic invasion; Iodine - consumption of iodine; a ways off metastasis, or met; Multif - a neoplasm with more than one foci; N stands for "patients," Present lymph node most cancers is referred to as a node, and n.s. pT4 – tumor size in the presence of extrathyroidal invasion; PTC stands for papillary cancer; patient's gender and sex; size—tumor measurement in the absence of extrathyroidal spread; surgical scope (complete or almost complete thyroidectomy versus a lot less than almost whole thyroidectomy); A 0.05 M-significant value. In the preceding 20 years, US-assisted aspiration for cytology and frozen section for the period of surgicahasocedure have ceased up commonplace. The share of stage T4 victims was once unaffected by using the upward jab in the range of victims with papillary carcinomas[44]. Best sturdiness is performed when thyroid gland nodes are dealt with early in the path of thyroid cancer, as is when thyroid carcinoma is operated on. [45]. Cytology's nodal distinction plays a significant phase in the surgical plan. Following surgical procedures, they did adequately for instances of cancer malignancy (C3-C5) that had been nice or suspicious. First, do away with one lobe if the high-quality needle check is negative; if the fixed pattern should, it should function as a whole thyroidectomy. Protection of the parathyroid and larynx repeatedly. If the frozen part is suspect and unclear, we go on to the almost complete section, where the ideal evaluation appears. Stage T1 solitary papillary carcinomas barring metastases, don't want any extra operations. During the research period, we carried out essential radical strategies on forty-five PTC sufferers in our hospital: 19 total and 26 near-total thyroidectomies, as correctly as eight lobectomies. Eighty-five situations required surgery to be finished. Thirty-six sufferers underwent theirfirstsura at are scurrentitalsent hospital, and we were recommended to them for their 2nd surgical system, notably based on their histology findings. The closing 12 situations involved 4 cases who underwent intraoperative frozen sections that failed to rule out malignancy or produced falsely benign (benign) diagnoses. Total thyroidectomies were performed in six instances, near-total thyroidectomies in fifteen cases, and lobectomies in one case. In 6 cases (27%), residual tumors had been found in the thyroid tissue as soon as removed. Twenty-five sufferers ucompletcomplete lobeeloblobe lobectomyyresect find-outfit-out periodriod, which is now not viewed as being sufficiently radical via using current therapeutic recommendations. This disproportionately wide variety can be attributed to the patients' opposition to extra surgery. Seven patients underwent FTC as the initial procedure, found through the ability of complete (in 3 patients) or almost whole (in 4 patients) thyroidectomies. Eight sufferers had profitable surgeries. Three of these patients had been recommended by another health center after their preliminary surgery. Histological evaluation of the remaining 4 cases revealed residual tumors in 1 of the specimens taken at some point of 4 complete and five almost total thyroidectomies. Between the groups, paresis of the recurrent laryngeal nerve occurred in 2.2–3.4% of instances and chronic hypoparathyroidism in 2.2–7.1%. According to the research, lymph node metastases occur between 35 and 60 percent more frequently in PTC sufferers than in FTC patients (15 to 20 percent less frequently). Its incidence in cases of childhood PTC can achieve 80%. They can moreover be located alongside papillary "microcarcinomas" (tumors much less than 1 centimeter in diameter), and they may be the preliminary clinical signal of the circumstance that prompts a diagnosis. 134 (34.7%) of our 386 PTC people had lymph node metastases. This approach might also reduce the extent of patients who initially gather a biopsy and then, as a stop result of the histology results, require a 2nd operation to furnish an everlasting surgical cure for the thyroid tumor. Local dissection (LD) or modified radical neck dissection (MRND) are two surgical methods that can tackle cervical lymph node metastases with a therapeutic or preventative measure. [46].
Less intense LD proponents contend that lymph node metastases do not affect survival. Neck dissection proponents contend that MRNDs executed as a preventative measure can become aware of lymph node metastases in up to 70% of cases with lousy palpation results. In most instances, completely the lymph nodes on the factor of thyroid, mo sand t cancers are affected. Forty-four LDs and 10 MRNDs had been carried on the e for the cervical lymph nodes that had metastasized to close-by organs on one occasion once as soon as palliative removal. In sixty-three individuals, more surgeries for recurrent lymph nodes involvemenwereen carried out. Eight sufferers required just one surgery, fous needed two more, one affected individual wanted three, and any other affected person desired four. Following LDs, four humans underwent some event surgery. Following MRNDs, there were sixteen Follow-up checks on seven patients with wrist recognize stagrecognizedrs primarily based on imaging techniques and histology-established lymph node metastases. We observed no proof that individuals with LDs the aid of myself had a greater relapse charge than those patients who had MRNDs; however, over the previous ten years, we have modified our method and now advocate performing MRNDs by the literature's recommendations. On the predictive value of the autoimmune response to thyroid carcinoma, the scientific literature is divided. High TSH or thyroid gland-specific antibody stages have been linked to malignant transformation, in accordance to some writers [47]., Others observed that papillary carcinoma cases with Hashimoto thyroiditis or lymphocytic infiltration had better prognoses [20]. Clinical and immunological lookup on differentiated thyroid carcinomas has produced findings that confirm the immune gadget performs a critical section in keeping the disease under control. Previously, each autologous human immune desktop and human carcinoma were transplanted into SCID (severe blended immune deficient) rodents. Our findings confirmed the magnitude of the immune system's function. Patients with PTC who had lymph node tumors were likelier to have seen lymphocytic infiltrations than those who did not. By at once sensitizing the lymphocytes in the lymph nodes, tumor cells accomplishing the regional lymph nodes motivate a more marked lymphocytic infiltration. This could be the purpose of the lower back of this phenomenon in PTC instances. Although there used to be no statistically sizable difference, lymphocytic infiltration was once as soon as related to a marginally higher prognosis in each PTC and FTC case in our sufferers throughout the study time. The unfolding of minimally invasive surgical cures in thyroid surgical operations is some other reason why it is essential to carefully sketch the scope of operations at the same time as bearing in mind the distinct prognostic factors[40]. Iodine isotopes, often 131I, had been current in excessive concentrations in the nuclear cloud, as is known adequately after radiation [48]. As a result, specialists are looking at how generally thyroid gland diseases, especially carcinomas, are occurring. By now, the majority of patients come with the papillary type, which is more common in younger due to radiation or genetic cause, and environmental factors and progresses aggressively and is accompanied by the aid of autoimmune thyroiditis [49 ].
In conditions the location the ailment is persistent or recurrent, a whole thyroidectomy can also also be necessary. Developing the quantity of recurrence threat factors (such as aggressive variants, ETE, pathologist-reported exceptional margins, gross disease invasion cautioned through the way of the surgeon, massive angioinvasion, or lymphovascular), or If the condition is chronic or constant, a total thyroidectomy may also be necessary. Containstains factors that increase the risk of recurrence (such as ETE, aggressive variants, significant margins reported by pathologists, or gross disorder reported by surgeons) invasion, substantial angioinvasion, or lymphovascular), or discovering evidence of a lymph node or distant metastasis after lobectomy
a good follow-up. The most appropriate time physique for complications-free thyroidectomy has been counseled to be three months. [28].
Finally, TT may also additionally restrict repeat costs and facilitate Tg stage monitoring (mainly when RAI is used); on the other hand, it will increase mortality. Comparatively speaking, the lobectomy preserves some inherent thyroid characteristics even as being plenty less invasive. Table 2
According to the latest research data, lobectomy is a plausible remedy for LRPTC sufferers during their disease's progression.
However, AS turns financially first-rate at age 69; additionally, after consulting with the endocrinologist and the surgeon, who need to additionally take into consideration the patient's socioesocioeconomic statusushniand c origin and get proper entry to pleasant care, the depth of surgical margin in LRPTC have to be determined: benefits and side effects of the procedures done in Table 5.
Monitoring Following Total Thyroidectomy and Lobectomy:
The findings of the neck US are primarily used to provide information on the follow-up of cases who have long gone through lobectomy. Introduction of benign tumors
These individuals may also fully receive ongoing follow-up. Tg and TgAb values over 12 months while on levothyroxine. To attain TSH levels in the usual or average range (0.5-2 IU/mL), levothyroxine dosage should be gradually increased. Interest assessments in specialized schools are debatable following 5–10 years aside from evidence of health problems ccausecausedhe possibilityrecurrminimalsminimal (69,70). Minor ailments t that can bar the issue be determined with neck US [50].
This study The choice for neck US monitoring is then again up for discussion, though, as sresearchershehavehas indicated that the danger of false-positive effects on neck US is excessive and may additionally result in inadequate remedy and follow-up. Or use CT for a more accurate diagnosis that gives the actual mass size and CT-guided true cute in follicular changes misdiagnosis. Fig.1
The histopathological type is crucial in the types of treatment and follow-up, and chemoradiation .further; the papillary type is the ccommonoreappearingafter after the histopathologic examination. The51]. The effect of these preliminary outcomes on affected character consequences has no longer been proven, and the ATA recommendations advocate easy surveillance for suspicious lymph nodes with a dimension of 10 mm (for lateral nodes) or eight mm (for central nodes) in the speedy axis. If there are no additional abnormalities in the preliminary neck ultrasound, we hope that a subsequent neck ultrasound would possibly now not be deliberate until three to 5 years after the preliminary treatment, if at all. In opposition to this, serum Tg ranges that increase over time generally suggest strengthening and persistent medical issues and should be examined with imaging tests. The modest rate of LRPTC's mortality, recurrence, and persistence enable safe guidelines for specialized approaches to management.[52]
Adjuvant radioactive iodine therapy after total thyroidectomy:
The choice to move on with adjuvant RAI therapy should consider the risks and advantages of RAI in patients with a low risk of recurrence and that delayed diagnosis of the disease does not shorten survival. Currently, the decision and recommendation for RAI treatment in this population of patients are primarily based on retrospective studies [12-53] showing no significant impact of adjuvant RAI therapy on overall or disease-free survival as well as prospective data from the NTCTCSG registry showing no significant impact of RAI treatment in low-risk patients [5-54] from multivariate analyses. Otheanotherer finding able 6
Ablation Resistant Tissues:
Used ablation after total thyroidectomy and In the setting of a typical cervical US, individuals with detectable TgAb levels and those with higher postoperative Tg levels may choose to explore. Multivariate analytics from numerous independent predictors of illness recurrence, according to research, is the postoperative serum Tg level. Other findings are in Table 6.
In summary, Papillary and follicular thyroid carcinomas have a correct prognosis. They have low tumor-related mortality rates, and contemporary diagnostic and therapeutic techniques have led to rising survival rates over the previous ten years. [15] By figuring out and using the predictive elements of survival, we can create a customized surgical method that addresses the scope of the surgical intervention, the need for follow-up care, and the regularity and extent of follow-up visits. The demographic parameters of the populace we studied with differentiated thyroid carcinomas have been the same as those published in different geographic areas. Cox regression evaluation located that in papillary carcinoma cases, table 5. While in sufferers with follicular carcinoma, age, more incredible thyroidal growth, and far-off metastases are quintessential prognostic variables, those with pT4 stage tumors, far-off metastases, and lymph node metastases are not. Although there was no discernible difference, lymphocytic infiltration suggested a marginally multiplied prognosis for every llary and follicular patient group. Iodine intake had no discernible impact on survival in either papillary or follicular carcinoma cases. However, in contrast to follicular carcinoma cases, the frequency of papillary carcinoma situations extended signifies the high iodine intake. This result is mainly attributable to using ultrasound imaging as a screening machine and cytological examination. Although re-operations are now no longer constantly necessary due to the fact pre- and intraoperative diagnostic methods are not constantly totally reliable, both one after the other or in combination, definitive operations are acknowledged to have the lowest incidence of problems (recurrent laryngeal nerve paresis and hypoparathyroidism). In cases of cervical lymphadenomegaly, pursuits diagnostic ultrasound imaging of the thyroid gland ought to be performed, followed, if required, by cytology (ultrasound-guided, if needed). This method could timelimit a range of cases which, at what, wins a biopsy and then, as a result of the histology results, require a 2nd operation to furnish a definitive surgical cure for the thyroid tumor itself. The choice of surgical technique depends on stages; radiotherapy is adjuvant and ablaremnantreminnet tumor.
Conclusions: