International Journal of Interventional Radiology and Imaging
OPEN ACCESS | Volume 3 - Issue 1 - 2025
ISSN No: 3065-6702 | Journal DOI: 10.61148/3065-6702/IJIRI
Arjun Anil 1*, Jawahar Rathod2, Shivprasad Jaybhay3, Shubham Yadav4, Aman Yusuf Khan5, Vishwas P6
1Senior Resident, Department of Interventional Radiology, Trauma Care Centre, Government Medical College and Hospital, Nagpur, Maharashtra.
2Professor and Head, Department of Interventional Radiology, Trauma Care Centre, Government Medical College and Hospital, Nagpur, Maharashtra.
3Assistant Professor, Department of Interventional Radiology, Trauma Care Centre, Government Medical College and Hospital, Nagpur, Maharashtra.
4Senior Resident, Department of Interventional Radiology, Trauma Care Centre, Government Medical College and Hospital, Nagpur, Maharashtra.
5Senior Resident, Department of Interventional Radiology, Trauma Care Centre, Government Medical College and Hospital, Nagpur, Maharashtra.
6Senior Resident, Department of Interventional Radiology, Trauma Care Centre, Government Medical College and Hospital, Nagpur, Maharashtra.
*Corresponding author: Arjun Anil, Senior Resident, Department of Interventional Radiology, Trauma Care Centre, Government Medical College and Hospital, Nagpur, Maharashtra.
Received: August 25, 2025 | Accepted: September 01, 2025 | Published: September 15, 2025
Citation: Anil A, Rathod J, Jaybhay S, Shubham Yadav, Aman Y Khan, Vishwas P., (2025) “Endovascular Cystic Artery Embolization in Cystic Artery Pseudoaneurysms: A Case Series showing Targeted Approach in Management of rare cause of Visceral Hemorrhage.” International Journal of Interventional Radiology and Imaging, 3(1); DOI: 10.61148/3065-6702/IJIRI/047.
Copyright: © 2025 Arjun Anil. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Cystic artery pseudoaneurysm (CAP) is an exceedingly rare vascular anomaly, often presenting with life-threatening upper gastrointestinal or intra-abdominal hemorrhage, associated with inflammatory or iatrogenic etiologies, such as calculus cholecystitis biliary interventions. Due to rarity and nonspecific presentation, CAP poses significant diagnostic and therapeutic challenges. This case series analyzes CAPs managed via selective endovascular embolization using microcatheter and embolic agents. Diagnostic imaging, procedural technique, and post-intervention interventions outcomes were reviewed. A concise review of literature is also undertaken to contextualize the clinical and technical aspects of this therapeutic strategy. Further surgical management was done as indicated. This case series underscores the value of a targeted endovascular approach, timely identification and intervention in addressing rare yet critical vascular emergencies within the hepatobiliary system
Cystic artery pseudoaneurysm ; Embolization ; Visceral Hemorrhage
CASE REPORT:
Cystic Artery Pseudoaneurysm (CAP) with hemorrhage is a rare life-threatening condition which can result in mortality if prompt treatment is not provided. Commonly associated with iatrogenic injury, like laparoscopic chocystectomy, it can also be secondary to acute calculus cholecystitis, Idiopathic, in acute pancreatitis and post traumatic. (1,2)
Acute cholecystitis can result in severe inflammation leading to thrombosis of vasa vasorum of the CA leading to vessel wall damage thus formation of pseudoaneurysm (PSA). (3,4) Patients present with obstructive jaundice, upper abdominal pain and Upper GI bleed (Quinke’s Triad), haemobilia and shock (1)(5)
The Cystic artery (CA) primarily originates from the right hepatic artery, supplying the GB and cystic duct in 79% to 89% of the population (Figure 1a and 1b). (6) Coursing through Calot's triangle, passing posterior to the cystic duct before bifurcating into superficial anterior and deep posterior branches at the gallbladder neck, forming extensive vascular network.(6) Variations are common. CA may arise from Left, Common Hepatic, or Gastroduodenal arteries.(7) Studies report double CA and variations in the artery's course relative to the cystic duct and Calot's triangle.(7)Understanding variations is crucial during endovascular procedures to prevent inadvertent embolization of hepatic artery and other branches.
Endovascular embolization is the minimally invasive procedure done by IR and it is the go-to emergency management for CAP for controlling active bleeds, helps in stabilizing the patients to recover from hemodynamic shock after which patient is further surgically or conservatively managed depending upon etiopathology.
The approach begins with percutaneous access preferentially under USG guidance, commonly via the Common Femoral Artery (CFA) under LA. A 5/6-French sheath is inserted, and a selective angiogram is performed using a catheter such as a Cobra C1 or Simmons S1 to identify the celiac trunk and subsequently the hepatic arterial system. A microcatheter (e.g. Progreat microcatheter 2.9 -2.7 Fr, 130 cms (Terumo Global, Japan) is advanced into the CA using fluoroscopic guidance. Super selective catheterization is critical to prevent non-target embolization and preserve hepatic arterial flow. Embolization is then performed using coils (e.g., detachable or pushable platinum coils), polyvinyl alcohol (PVA) particles, or liquid embolic agents such as N- butyl cyanoacrylate (NBCA) depending on the vessel's anatomy and operator preference.
Post-embolization angiography confirms occlusion of the PSA and cessation of flow. The technique is highly effective, offers rapid hemostasis, and avoids the morbidity associated with surgical intervention.
CASE 1:
Clinical history: A 47y/M patient presented to the surgery casualty with severe abdominal pain in the last 2 days with 3 episodes of melena and 1 episode of hematemesis. He has Tachycardia and hypotension. Hemoglobin- 5.5 gm% and WBC -15,700x109 /L. LFT revealed bilirubin at 3.4 mg/dL.
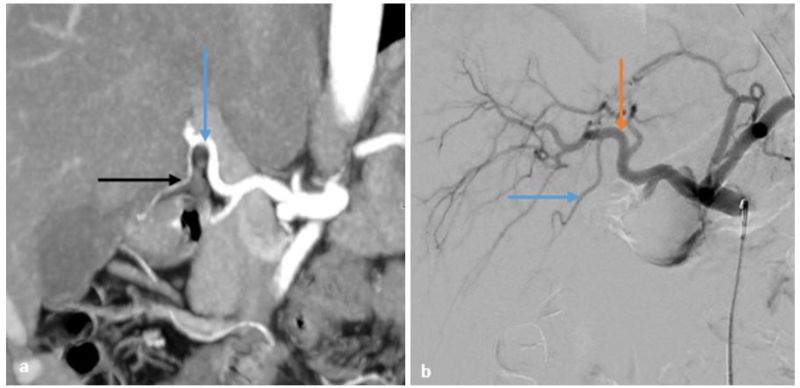
Figure 1: 1a- CT Angiography MPR image showing Right hepatic artery ( Blue arrow) and Cystic artery ( Black arrow); 1b- DSA image showing Right Hepatic artery (Orange arrow) and Cystic artery (Blue arrow)
Imaging: USG à Acute calculus cholecystitis with echogenic content in the CBD and mild central IHBRD. CECT showed a distended gall bladder with multiple large calculi (Figure 2a-d) and was surrounding a hypodense sac like structure which showed complete filling of contrast. Lesion measures 28 x 42 x 36 mm and was diagnosed as a CAP probably secondary to acute calculus cholecystitis (Figure 2a-d). There was also suspicion of a rent in the wall of fundus of the gall bladder.
Intervention: Right CFA approach was taken to cannulate Celiac Trunk. A microcatheter was used to cannulate CA(Figure 2 e-h).The cystic artery angiogram revealed a ruptured cystic artery with a large PSA. The microcatheter was taken distally and the PSA was embolized with 25% Cyanoacrylate Glue. (Figure 2 e-h).
Post embolization patient was taken up for laparoscopic cholecystectomy due to risk to post embolization ischemia, perforation and sepsis. A gangrenous GB was seen intraoperatively and subtotal cholecystectomy was done (Figure2 i-l). The patient returned after 2 weeks with abdominal pain, fever and had developed infected collections in the right hypochondrium and pelvis. The collections were drained and patient was discharged.
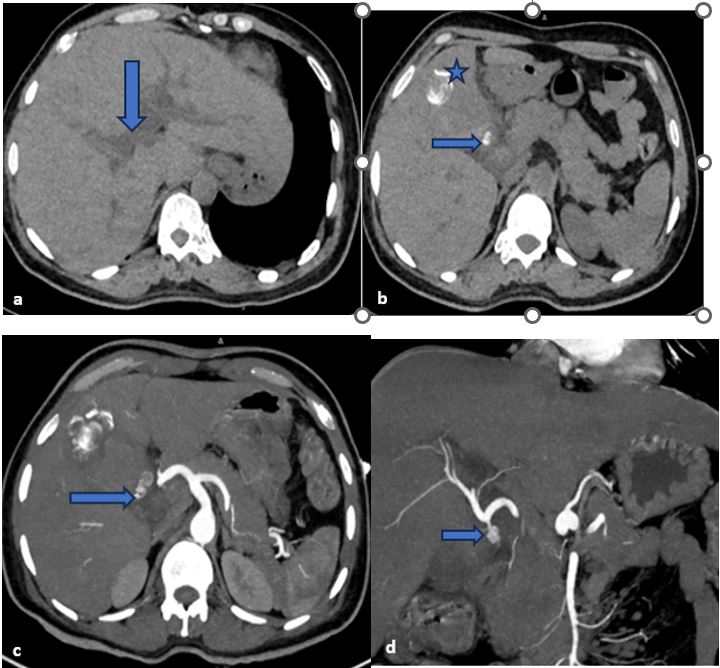
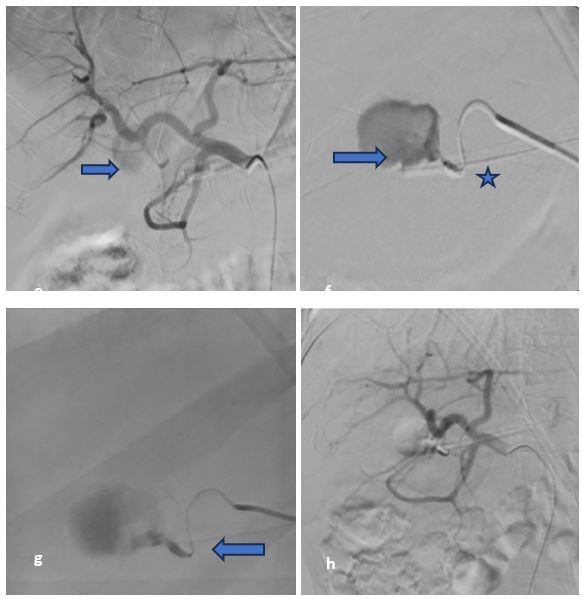
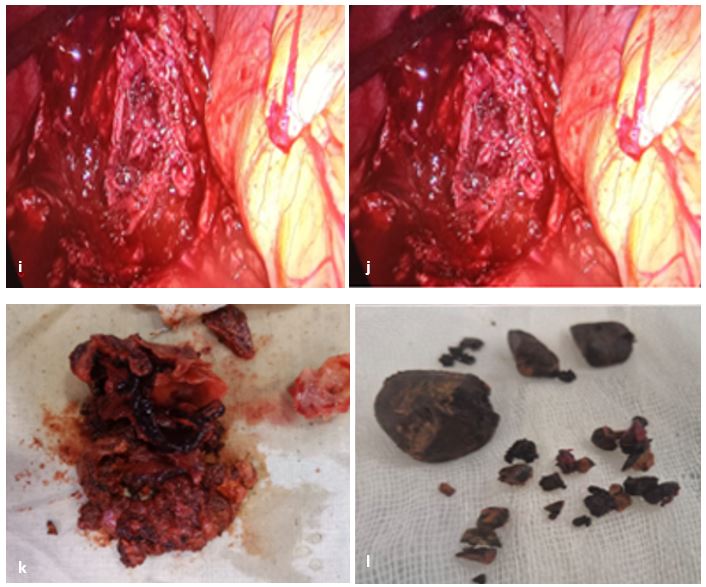
Figure 2 – Plain and contrast phase images of CECT abdomen of the patient a&b) Plain CT image showing bilobar intrahepatic biliary radicle dilation( Blue vertical arrow) b) Multiple intraluminal calculi within gall bladder( Blue star) and a calculus at the GB neck( Horizontal blue arrow). c) shows pseudoaneurysm arising from cystic artery (Blue horizontal arrow). D) MPR coronal image
showing cystic artery pseudoaneurysm (Blue horizontal arrow). 2e-f Angiography and trans-arterial embolization of cystic artery. e) Common hepatic artery angiogram showing cystic artery arising from right hepatic artery with large pseudoaneurysm (Horizontal blue arrow) f) Super selective angiogram from distal cystic artery (Blue star) opacifying the pseudoaneurysm (Horizontal blue arrow) g) Glue injection to embolize the pseudoaneurysm (Horizontal blue arrow) h) Post embolization angiogram revealing exclusion of the pseudoaneurysm and cystic artery from circulation. 2i-l)Laparoscopic resection of ruptured gall bladder i) and l) show laparoscopic partial resection of gall bladder k) Resected gall bladder l) extracted calculi.
Case 2:
Clinical history: A 42 yr/M with complaints of right hypochondriac pain for past 2 days with fever for past 24 hours. Hypotension with deranged LFT and elevated WBC counts was noted.
Imaging: USG revealed thickened edematous GB wall and heterogenous content within lumen. Eccentric foci of color uptake with ying yang sign seen was intraluminally (Figure 3 a). CT angiography showed a contrast filled saccular lesion measuring 12*9*14 mm within GB lumen with pericholecystic fluid collection and definitive rent in GB fundus. (Figure 3 b-d).
Intervention: Using right CFA approach celiac and common hepatic arteries were cannulated. CA was cannulated using Progreat microcatheter (Terrumo). Angiography showed the pseudoaneurysm. The embolization was attempted using pushable coils however the coils migrated into PSA sac.The feeder was embolized using 20% Cyanoacrylate Glue + Lipiodol combination. Post embolization runs showed complete exclusion of the lesion from the arterial system (Figure3 e-h). Patient was transferred to surgery where the Cholecystectomy was done as there was already a rent in the GB fundus. Patient then discharged.
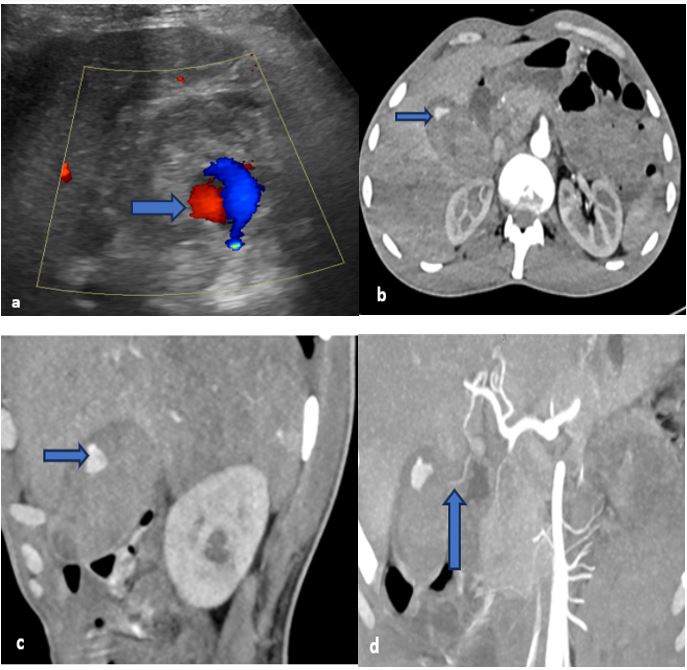
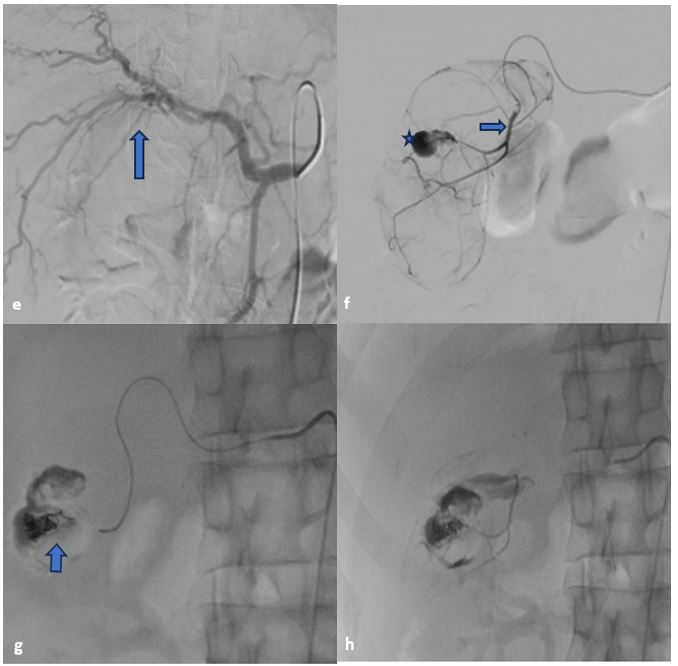
Figure 3– 3a showing Ying yang sign within gallbladder lumen (Blue arrow). 3b showing a hyperenhancing pseudoaneurysm in the GB lumen (Horizontal bluearrow). 3c- MPR sagittal section showing pseudoaneurysm (Horizontal blue arrow). 3d- MPRimage showing course of cystic artery (Vertical blue arrow). 3e- Figure shows origin and course of Cysticc artery (Blue vertical arrow); 3f- Figure shows pseudoaneurysm, from Cystic artery(Blue star) and super selectively cannulated cystic artery using microcatheter. 3g- Coil mass within pseudoaneurysm (Blue Arrow); 3h- Figure showing glue cast with embolized pseudoaneurysm.
Case 3:
Clinical History: A 30Y/M patient who had blunt abdominal trauma to the upper right quadrant developed severe pain, deranged LFT and anemia.
Imaging: CECT showed a small intraluminal GB PSA with GB wall edema and heterodense content within the GB and pericholecystic minimal free fluid. (Figure 4 a&b).
Intervention: Using right CFA approach celiac trunk and common hepatic artery were cannulated. Using microcatheter CA was super selectively cannulated and angiographic runs taken which showed a small pseudoaneurysm arising from the branch of cystic artery. The feeder branch was embolized using pushable coil 2*7 mm. (Nester, Cook,US) with occlusion of front and backdoor accesses (Figure 4 c &d). Patient was then transferred to Surgery and was then taken up for cholecystectomy. Post procedure patient was discharged successfully and is doing well.
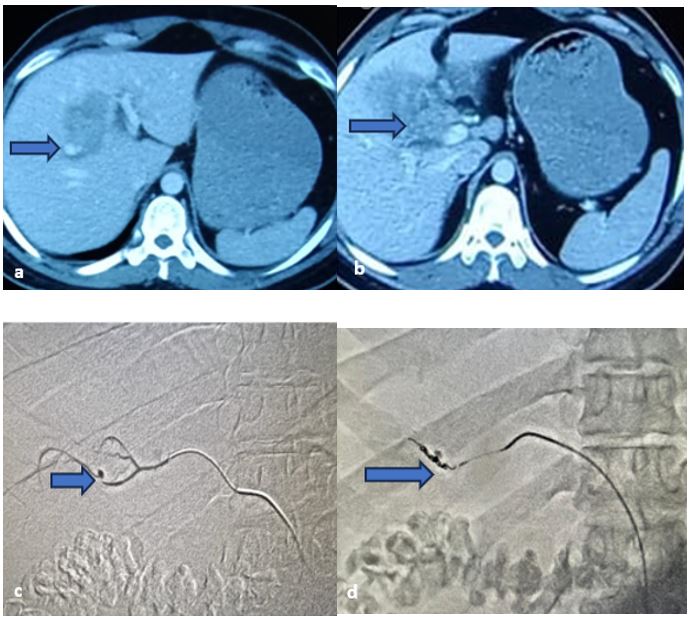
Figure 4: a- CECT angio, arterial phase showing a pseudoaneurysm within GB lumen (Bluearrow); b- Pericholecystic hepatic hypodensities and pericholecystic fluid collecttion; c-Superselective cyctic artery run showing pseudoaneurysm (Blue arrow); d- Coil embolization of the feeder artery.
Case 4:
Clinical History: A 28-year-old female who had acute on chronic pancreatitis and had underwent laparotomy and peritoneal wash presented with bloody output from one of her drains and a rapidly falling hemoglobin
Imaging: CECT showed a small intraluminal GB PSA within the gall bladder neck with peri-cholecystic free fluid. (Figure 5a). There is a large peripherally enhancing collection extending from infrahepatic region, along right paracolic gutter into pelvis (Figure 5b)
Intervention: Using right CFA approach celiac trunk and common hepatic artery were cannulated. Using microcatheter CA was super selectively cannulated and angiographic runs taken which showed a small pseudoaneurysm arising from the branch of cystic artery (Figure 5 c). The cystic artery was embolized using 20% Cyanoacrylate Glue with occlusion of front and backdoor accesses (Figure 5d). Patient was then transferred to Surgery and was kept under observation where she gradually improved and she did not develop ischemic cholecystitis. She was later taken up for laparotomy (1 week later) and drainage of the collection with peritoneal wash and cholecystectomy, however she eventually succumbed to hospital associated infections.
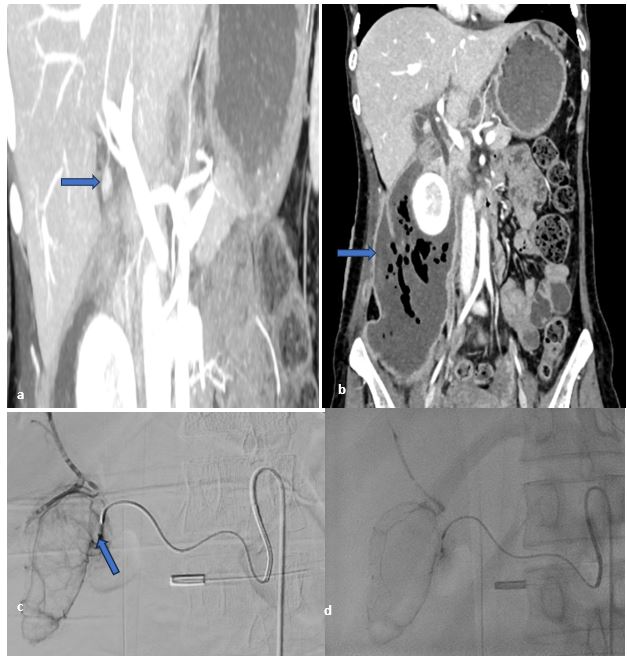
Figure 5: a- CT angio, arterial phase coronal MIP imagesshowing a pseudoaneurysm within GB neck (Blue arrow); b- CECT venous phase coronal images showing Large peripherally enhancing collection extending from infrahepatic region, along right paracolic gutter into pelvis (blue arrow); c- Superselective cyctic artery run showing pseudoaneurysm (Blue arrow); d- Glue cast post glue embolization.
|
Case No. |
Etiology |
Embolization Agent |
Surgery done |
Outcome |
|
1 |
Acute Cholecystitis |
Cyanoacrylate Glue |
Subtotal cholecystectomy |
Patient stabilized and discharged |
|
2 |
Acute Cholecystitis |
Cyanoacrylate Glue + Coils |
Total cholecystectomy post gallbladder rupture |
Patient stabilized and discharged |
|
3 |
Blunt Abdominal Trauma |
Cyanoacrylate Glue + Coils |
Total cholecystectomy |
Patient stabilized and discharged |
|
4 |
Acute on Chronic pancreatitis |
Cyanoacrylate Glue |
Total cholecystectomy + collection drainage + peritoneal wash |
Demise due to infections |
The above table is the summary of all 4 cases with their outcomes, showing the various causes of cystic artery pseudoaneurysm and its management through a combined endovascular plus surgical approach.
Discussion:
CAP is a rare condition and the reason for its occurrence in a case of acute cholecystitis is still not clear, even though it is one of the most common causes for the condition.(8) Arterial wall weakening, especially the adventitia, secondary to acute surrounding inflammation of the gall bladder is one hypothesis.(3,4) Other cause of CAP if post cholecystectomy or any other iatrogenic injury, or sometimes even in blunt trauma of abdomen or acute pancreatitis as we can see in this paper.(9) Older literature and case reports have shown that this condition is more common in older individuals, usually seen above 70 years of age, however this was not seen our cases as our patients were middle age males.
Haemobilia is the most common presentation, however there is a need for high clinical suspicion to detect haemobilia.(1)The classical Quincke’s triad of right upper quadrant pain, upper GI bleed and jaundice is seen only in 22-35% of the cases.(5) 82.1% of the cases present with upper abdominal pain, 64.4% with upper GI bleed and 58% with jaundice.(8) Obstructive jaundice was secondary to blood in the CBD which was evident on our CT scan. Morbidity in patients with CAP is high as condition may deteriorate rapidly due to multiple factors including Hemodynamic shock, Rapid derangement of Liver function and early onset sepsis.(1) Our patients presented with features of upper GI bleed (hematemesis and melena), hemodynamic shock, upper abdominal pain and obstructive jaundice.
USG is the first line radiological investigation in upper abdominal pain and was the first radiological investigation our patients underwent. However, the sensitivity of USG for detecting cystic artery pseudoaneurysm is low and we have to depend on ancillary findings like IHBR and echogenic contents in the gall bladder and CBD to raise a suspicion. CECT abdomen is the go-to investigation for detection of pseudoaneurysms and to detect the associated complications like hemoperitoneum and CBD obstruction.(4) MR angiogram can be advised in patients where CECT cannot be done like in cases of chronic kidney disease or contrast allergy.(1) The diagnosis of all four patients in our institute was confirmed on CECT abdomen.
Endovascular embolization is the first line of treatment on identification of CAP as it is minimally invasive and can be done under LA on emergency basis. All 4 of our patients were taken up in Cath lab on emergency basis for arterial embolization to control the internal hemorrhage and to stabilize the vitals. Technical success rate was 100% in all our 4 cases. Embolization agents including both liquid as well as coils. Some researchers have described percutaneous direct Thrombin injection into PSA using real time USG and Doppler. However this carries great risk of inadvertent embolization of other vessels with risk of Hepatic and bowel ischemia and infarction.(10)
It has also been noted that none of our patients developed features of ischemic cholecystitis post cystic artery embolization. Although the majority of the patients underwent early elective cholecystectomy, case 4 where the entire cystic artery and its branches were embolized with NBCA, also did not result in ischemic cholecystitis even after the patient was kept under observation for 1 week and the cholecystectomy was done 1 week later
Patients would have needed to undergo emergency laparotomy and vascular control if the if the endovascular procedure would not have been provided. However, post successful embolization all the 4 patients underwent elective cholecystectomy with excellent outcomes.
Conclusion:
Although CAP is a rare entity, Acute Cholecystitis is one of the most common surgical ailments in the world. Patient of acute cholecystitis presenting with unexplained Anemia, Hemoperitoneum, Malena or hematemesis should always alert the physician for suspected CAP. Physician should send emergency call to IR for such patient as the patient can deteriorate rapidly. Endovascular management with its minimally invasive nature is the go-to management for almost all such emergencies and with the combined efforts of an IR followed by surgery for such patients is lifesaving with excellent prognosis.
Conflict of Interest:
Authors declare they have no conflict of interest.