International Journal of Integrative and Complementary Medicine
OPEN ACCESS | Volume 2 - Issue 1 - 2025
ISSN No: 2836-2810 | Journal DOI: 10.61148/IJICM
Jose Luis Turabian
Specialist in Family and Community Medicine.
Health Center Santa Maria de Benquerencia. Regional Health Service of Castilla la Mancha (SESCAM), Toledo, Spain.
*Corresponding author: Jose Luis Turabian, Health Center Santa Maria de Benquerencia Toledo, Spain.
Received: July 05, 2025 |Accepted: July 20, 2025 |Published: August 04, 2025
Citation: Jose Luis Turabian, (2025) “Long Covid-19 Show Significantly Decreased Prevalence Trend In 2025 Versus 2022 In A General Medicine Clinic In Toledo (Spain)..” International Journal of Integrative and Complementary Medicine, 1(1). DOI: 10.61148/ 10.61148/IJICM/ 002.
Copyright: © 2025 Jose Luis Turabian. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background
Five years after the start of the COVID-19 pandemic, the evolution of the frequency of Long-Term COVID-19 is not well known.
Objective
To analyze the variation in the frequency of Long-Term COVID-19 in 2022 compared to 2025.
Methodology
Comparison of the prevalence of Long-Term COVID-19 among two cross-sectional descriptive studies: 1) patients with Long-Term COVID-19 (symptoms prolonged beyond 12 weeks) on October 31, 2022, and 2) the prevalence of Long-Term COVID-19 on May 31, 2025, in the same population in general medicine in Toledo (Spain).
Results
For a population of 2,000 people seen at the study clinic, 27 cases of Long COVID-19 were found on October 31, 2022 (crude prevalence of 1.35%) and 3 cases on May 31, 2025 (crude prevalence of 0.15%) [p-value = .000011]. Long COVID-19 cases in May 2025 vs. October 2022 occurred in middle-aged individuals (> 45 and < 65 years): 100% vs. 33% [Fisher exact test = 0.05], and 100% vs. 48% were women [Fisher exact test = 0.2276].
Conclusion
The frequency of Long COVID-19 has decreased significantly from 2022 to 2025. Cases currently predominate in middle-aged women.
COVID-19; SARS-CoV-2; Long COVID-19 condition; General Practice; Epidemiology
The coronavirus disease (COVID-19), caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), was first reported in China in December 2019 and spread rapidly in many countries. COVID-19 is a devastating disease that has infected millions of people since the beginning of 2020, through its multisystemic manifestations that vary widely in severity (1).
The Centers for Disease Control and Prevention confirmed its first case of COVID-19 in the US in early 2020, and eight months later, the World Health Organization (WHO) described a post-viral condition called Long COVID-19. Since then, millions of Americans, about 8% of those with acute COVID-19, have also been diagnosed with Long COVID-19 (2).
Because of new SARS-CoV-2 infections continue to occur today, despite advances in vaccines, antiviral medications, and preventative measures. Long COVID-19 remains a significant public health problem (3, 4)
The risk of developing long-term COVID-19 has been reported to have decreased significantly since the start of the pandemic (5). However, the overall evidence on the risk of long-term COVID-19 symptoms in general populations remains unknown (6). Thus, five years after the onset of COVID-19, it is unknown how many people have long COVID-19. The difficulty of diagnosis, the lack of knowledge among many professionals, and the lack of biological markers complicate the recognition and management of the disease (7). Temporal changes during the COVID-19 pandemic, including the evolution of SARS-CoV-2 and vaccination, may have affected the risk and burden of post-acute sequelae. However, it is unclear whether the risk and burden of post-acute sequelae have changed throughout the pandemic (5).
In this context, we present a study to analyze the variation in the prevalence of long-term COVID-19 (presence of prolonged symptoms for at least 12 weeks) in 2022 compared to 2025 in a population of a general medicine outpatient clinic.
Material And Methods
Design and emplacement
Comparison of data between two cross-sectional descriptive studies:
1) patients with Long COVID-19 on October 31, 2022, already published (8).
2) patients with Long COVID-19 on May 31, 2025.
Both studies were carried out in the same population of patients treated in a general medicine office in the Health Center Santa Maria de Benquerencia, Toledo (Spain), which has a list of 2,000 patients > 14 years of age (in Spain, the general practitioners [GPs] care for people > 14 years of age, except for exceptions requested by the child's family and accepted by the GP).
Objective
To analyze the variation in the prevalence of Long COVID-19 in 2022 compared to 2025.
Criteria of Long-COVID-19
Due to the novelty and diversity of its manifestations, various terms and definitions have been proposed for persistent COVID-19, although none have gained widespread acceptance and support from patients, physicians, researchers, or government agencies (9). In our 2025 cross-sectional study, we retained the criteria used in the 2022 cross-sectional study to allow for comparability (8).
Basically, long-COVID-19 was diagnosed by the presence of prolonged symptoms for at least 12 weeks, lasting at least 2 months, after acute COVID-19 infection that are not explained by an alternative diagnosis (10). WHO defines long-COVID-19 as a post-COVID-19 condition that occurs among persons with probable or confirmed SARS-CoV-2 infection, usually 3 months from the onset of COVID-19, that lasts for at least 2 months, and cannot be explained by an alternative diagnosis (11-13).
Inclusion criteria
1. Patient with confirmed SARS-Co-2 infection or with high clinical suspicion in the case of patients in the 1st wave (where out-of-hospital diagnostic tests were not performed).
2. Presence of one or more symptoms or signs as more frequent in Long COVID-19 (Asthenia, Headache, Arthralgia, Dyspnea, Insomnia, Myalgia, Chest pain, "Brain fog", Rashes, Tachycardia, Anosmia/Dysgeusia, Dysthermia, Cough, Depression, Erratic pain, Muscle pain, fatigue, anorexia and mood swings), and others associated with acute SARS-Co-2 infection, which persists for more than 12 weeks, and for which there is no alternative explanation. Symptoms may be new onset following recovery from acute covid-19, or persist from the initial illness. Symptoms can also fluctuate or relapse and remit over time; they may be chronically maintained or progress to complete recovery in subsequent months.
Exclusion criteria
1.-Patients with specific sequelae of acute infection were not included:
A) Pathologies that are not part of the acute infection, persistent, that appear during the COVID-19 infection
B) Pathologies that are not part of the acute infection, persistent, with appearance after the resolution of the initial symptoms (COVID-19 post-infection pathologies)
C) Pathologies that are not part of the acute infection, but appear as a consequence of the organic damage caused by the severe infection (true sequelae of COVID-19).
2. The symptom or symptoms were already present before the infection. This would be a previous pathology aggravated or reactivated by COVID-19.
3. The symptom or symptoms were not present in the initial picture, they appear after the resolution of the initial picture. Post-infection COVID-19 symptoms or pathologies.
Statistic analysis
The bivariate comparisons were performed using the Chi Square test (X2) or Fisher Exact Test when necessary (according to the number the expected cell totals).
Ethical issues
No personal data of the patients were used, but only group results, which were taken from the clinical record
Results
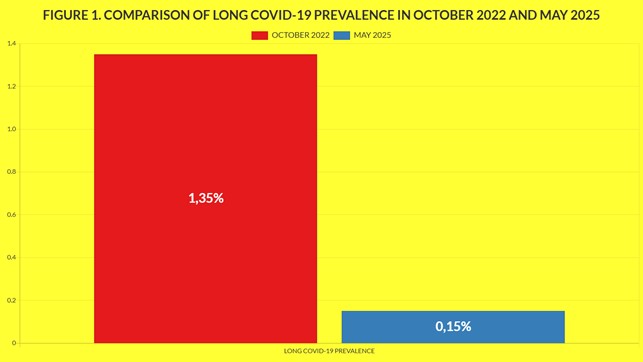
For a population of 2000 people attended in the clinic object of the study, 27 cases of Long COVID-19 were found on October 31, 2022 (crude prevalence of 1.35%) and 3 cases on May 31, 2025 (crude prevalence of 0.15%) [p-value = .000011]. Cases of Long COVID-19 on May 2925 vs. on October-2022 were of 100% vs. 33% in people of middle ages (> 45 and < 65 years) [Fisher exact test = 0.05], and 100% vs. 48% women [Fisher exact test = 0.2276] (TABLE 1, FIGURE 1).
Table 1: Comparison Of Long Covid-19 Prevalence In October 2022 And May 2025
|
VARIABLES |
LONG COVID-19 IN OCTOBER 2022 |
LONG COVID-19 IN MAY 2025 |
STATISTICAL SIGNIFICANCE |
|
TOTAL |
27/2.000 (1.35) |
3/2.000 (0.15) |
X2=19.3451. p-value is .000011. Significant at p < .05. |
|
> = 65 years |
7/27 (26) |
0 |
Fisher exact test= 1. NS |
|
> 45 and < 65 years |
9/27 (33) |
3/3 (100) |
Fisher exact test= 0.05. NS |
|
Women |
13/27 (48) |
3/3 (100) |
Fisher exact test= 0.22. NS |
( ): Denotes percentages
NS: Not significant at p< .05.
Figure 1: Comparison Of Long Covid-19 Prevalence In October 2022 And May 2025
Discussion
1. Main findings
Our main findings were:
1. The crude prevalence of long COVID-19 in the study clinic was significantly lower in May 2025 compared to the prevalence in October 2022: 1.35% vs. 0.15%.
2. Long COVID-19 cases in May 2025 vs. October 2022 were predominantly in middle-aged individuals (> 45 and < 65 years) [100% vs. 33%] and women [100% vs. 48%].
Since 2020, SARS-CoV variants cover the alpha, beta, gamma, delta, and omicron spectrum. In Spain, the Alpha variant was dominant during 2020. In August 2021, the Delta variant accounted for 90% of total cases in Spain. In May 2022, the Omicron variant was the dominant one in Spain after having displaced the Delta variant. The predominant variants in Spain during 2023 were those of the XBB family. In January 2024 in Spain, XBB.1.5-like + F456L accounted for 42% and BA.2.86 for 44% of positive cases. In July and August 2024, the KP.3 lineage was detected in 84% of cases. In September 2024, the incidence of the XEC variant of the coronavirus, a new Omicron subvariant was increasing markedly in Spain. At that time, it was the second most common strain in cases recorded in September, although still far behind the main KP.3.3, with an incidence of 13% (14, 15).
On the other hand, in Spain, in November 2022, more than 60% of people over 80 years of age, and 37% of people over 60 years of age, already had the second booster dose of the COVID-19 vaccine (16, 17). And 60% of the population over 80 years of age has already received the vaccine adapted against the COVID-19 subvariants of the 2023/2024 campaign (18).
In any case, the results must be evaluated with caution. In Spain, since April 28, 2022 there was a new "Surveillance and Control Strategy Against Covid-19" that included the non-performance of diagnostic tests, which were focused only on those over 60 years of age (19). This means that positive cases have been counted with tests carried out in health services and with tests carried out at home and later reported to the GP. Thus, there is probably an underreporting.
2. Comparison with other studies
Existing evidence suggests wide variations in estimates of the prevalence and incidence of long COVID-19 due to differences in study populations, recruitment methods, follow-up periods, and sample sizes (20). Regarding the prevalence of long-term COVID-19, it is important to note that many studies assess it through self-reports/questionnaires, which may lead to potential detection bias (21).
A cohort study conducted in China in 2020 that followed COVID-19 patients 6 months after discharge from acute infection included 1,733 patients, 1,265 (76%) reported symptoms during follow-up (22). In 2021, the UK Office for National Statistics followed more than 20,000 people who tested positive since April 2020; it found that 14% still reported symptoms after at least 12 weeks (23).
The risk of developing Long COVID-19 has been reported to have significantly decreased since the start of the pandemic. A study conducted between March 1, 2020, and January 31, 2022, found that among vaccinated individuals, the 1-year cumulative incidence of Postacute Sequelae of SARS-CoV-2 Infection was 5.34 events per 100 people during the Delta era and 3.50 events per 100 people during the Omicron era (difference between the Omicron and Delta eras, −1.83 events per 100 people). Vaccinated individuals had a lower 1-year cumulative incidence of Postacute Sequelae of SARS-CoV-2 Infection than unvaccinated individuals. About 70% of the decrease was assessed to be attributable to vaccination (vaccines reduce the risk of severe acute infections, which are linked to a higher risk of Long COVID-19; vaccines also help the body’s immune system clear the virus more quickly, reducing the likelihood of lingering viral particles), and the remaining 30% was related to changes in viral characteristics (as SARS-CoV-2 evolved, it changed in ways that might have made people less susceptible to developing Long COVID-19) (5, 24).
In a study in France during the first wave (March-May 2020) or the second wave (September-November 2020), among participants aged 15 years and older in a national population-based cohort, the risk of post-COVID symptoms was 14.6% in March-May 2020, compared with 7.0% in September-November 2020 (25).
Using data from a self-administered online survey in a national, cross-sectional, observational cohort study in Italy, sponsored by the Cardiovascular Prevention Laboratory of the Istituto di Ricerche Farmacologiche Mario Negri IRCCS, and conducted in collaboration with a large network of GPs, between October 2021 and December 2022 among 1,108 individuals aged 18 years and older, the prevalence of Long COVID-19 was assessed in 29% of patients (26). Other data from the first 2 years of the pandemic (March 2020 to January 2022) indicate that initially, approximately 10% of people who suffered COVID-19 infections developed long COVID-19.
Currently, this risk has decreased to approximately 3.5% among vaccinated people. Some research shows that early COVID-19 strains and earlier variants such as Delta appeared to produce more severe forms of long-term COVID-19 than later strains. Researchers found that the rate of new long-term COVID-19 cases decreased with each variant from the pre-Delta through Omicron eras, and that the number of cases was significantly lower in vaccinated cohorts (2). In the United States alone, survey data published in 2023 and 2024 indicate that approximately 7% of adults and more than 1% of children—numbering 15 to 20 million Americans and more than 60 million globally—have had long COVID-19 (9). According to the latest count in 2024, about 18% of those surveyed by the Centers for Disease Control and Prevention said they had experienced long COVID (27).
In a systematic review of long COVID-19 using a secondary analysis of data collected from anti-coronavirus therapy trials in a substantial number of countries around the world (Argentina, Brazil, Canada, Colombia, Ecuador, Egypt, India, Nepal, Pakistan, the Philippines, Russia, Saudi Arabia, South Africa, and the United Arab Emirates), 25% of patients with previous symptomatic COVID-19 reported possible symptoms of long COVID-19. This study showed that the frequency of long COVID-19 may be higher in countries with lower income levels: 30% versus 14%; and in patients of Arab or North African ethnicity (36%) (28).
In Spain, there is no official registry of patients with Long COVID-19, but it is estimated that more than two million Spaniards continue to experience symptoms months after contracting the disease (29). And 70% are women (30). Another measure of the magnitude of the phenomenon is sick leave. In Spain, the percentage of patients who develop Long COVID-19 after being on sick leave due to COVID-19 has been declining: in the first year, the estimate was 16% of those infected, while it is now approximately 4%. In the case of seriously hospitalized patients, the proportion skyrockets: between 60% and 80% require sick leave due to Long COVID-10 (7).
In summary, our study confirms the significant decrease in the prevalence of Long COVID-19 today, which is predominant in middle-aged women. However, since this reduction in prevalence is likely due to the change in SARS-CoV variants and the vaccination rate, it is not possible to transfer our data to other contexts. Furthermore, since COVID-19 cases continue to occur, it is also impossible to predict its future course. In any case, maintaining the vaccination rate is likely to be a key factor in maintaining or reducing the incidence of Long COVID-19.
Limitations and strengths of the study
1. The population and investigator were the same in both studies, which could allow for reliable results that could be generalizable to similar populations.
2. The number of cases was small, which may hide differences between the groups.
3. There is likely underreporting of Long COVID-19, especially in the 2025 cross-sectional study, as neither diagnostic testing was systematically performed for acute cases nor screening for asymptomatic patients.
Conclusions
In the context of general medicine in Toledo (Spain), the frequency of Long COVID-19 has decreased significantly from 2022 to 2025, and cases currently predominate in middle-aged women. However, given that cases of COVID-19 continue to occur despite the high vaccination rate in the population, the risk of Long COVID-19 is not negligible and should be taken into account.