International Journal of Clinical Gynaecology and Obstetrics
OPEN ACCESS | Volume 3 - Issue 1 - 2025
ISSN No: 2836-0737 | Journal DOI: 10.61148/2836-0737/IJCGO
Edmund O. Ezirim 1, Emmanuel M. Akwuruoha 1, Chyke I. Amah1, Christian O. Onyemereze 1* and Augustine I. Airaodion 2
1Department of Obstetrics and Gynaecology, Abia State University Teaching Hospital, Aba, Nigeria.
2Department of Biochemistry, Lead City University, Ibadan, Oyo State, Nigeria.
*Corresponding author: Christian O. Onyemereze, Department of Obstetrics and Gynaecology, Abia State University Teaching Hospital, Aba, Nigeria.
Received: August 05, 2025 |Accepted: August 22, 2025 |Published: August 25, 2025
Citation: Edmund O. Ezirim, Emmanuel M. Akwuruoha, Chyke I. Amah, Christian O. Onyemereze and Augustine I. Airaodion,, (2025) “Knowledge, Attitude and Perception towards Premature Ovarian Insufficiency among Nigerian Women” International Journal of Clinical Gynaecology and Obstetrics, 5(1); DOI: 10.61148/2836-0737/IJCGO/040.
Copyright: © 2025 Christian O. Onyemereze. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: Premature ovarian insufficiency (POI), defined as the cessation of ovarian function before the age of 40 years, significantly impacts fertility, quality of life, and long-term health in affected women. Despite its clinical relevance, awareness and perceptions about POI among women in Nigeria remain poorly understood. This study assessed the knowledge, attitude, and perception (KAP) regarding POI among Nigerian women.
Materials and Methods: A hospital-based descriptive cross-sectional study was conducted among 300 Nigerian women aged 18–49 years attending gynecology clinics at Abia State University Teaching Hospital, Aba. Participants were selected using a systematic random sampling technique. Data were collected using a pretested, semi-structured interviewer-administered questionnaire covering sociodemographics, knowledge, attitudes, and perceptions of POI. Knowledge scores ≥50% were considered adequate, while Likert-scale mean scores determined positive attitudes and favorable perceptions. Data analysis was performed using IBM SPSS version 27, employing descriptive statistics, Chi-square tests, t-tests, and logistic regression, with p < 0.05 considered significant.
Results: The mean age of participants was 33.4 ± 7.1 years; 62.0% were married, and 48.3% had tertiary education. Awareness of POI was 47.0%, with only 42.7% demonstrating adequate knowledge. Infertility was the most recognized complication (62.7%), while awareness of hormonal therapy (34.7%) and risk factors (27.3%) was low. Positive attitudes were recorded in 57.0% of participants, and favorable perceptions in 53.0%. Significant correlations were found between knowledge and attitude (r = 0.412, p < 0.001), knowledge and perception (r = 0.368, p < 0.001), and attitude and perception (r = 0.529, p < 0.001). Higher education level was significantly associated with adequate knowledge (χ² = 27.51, p < 0.001), and marital status with positive attitude (χ² = 14.29, p = 0.002).
Conclusion: Knowledge of POI among Nigerian women is suboptimal despite generally positive attitudes and favorable perceptions. Educational interventions targeting women of reproductive age are essential to improve awareness, promote early diagnosis, and mitigate the health and social consequences of POI.
premature ovarian insufficiency, knowledge, attitude, perception, reproductive health, early menopause
Premature ovarian insufficiency (POI), also called primary ovarian insufficiency, is a clinical syndrome of impaired ovarian function occurring before age 40, characterized by menstrual disturbance and biochemical evidence of ovarian insufficiency (elevated gonadotropins with low estradiol) after exclusion of secondary causes [1]. POI is distinct from natural menopause because ovarian activity may be intermittent and spontaneous conception remains possible, though uncommon. Contemporary consensus statements stress standardized terminology (using “insufficiency,” not “failure”), clear diagnostic thresholds, and proactive, woman-centred care pathways. These points are captured in the 2024–2025 international guideline jointly developed by ESHRE, ASRM, the International Menopause Society and CRE-WHIRL, which provides 145 recommendations spanning symptoms, diagnosis, aetiology, sequelae and management [1,2].
POI represents a meaningful, but often under-recognized, component of women’s health need. Pooled global estimates suggest that approximately 3–4% of women experience POI, although prevalence varies with diagnostic criteria and population characteristics. A 2019 meta-analysis reported the combined prevalence of POI and early menopause worldwide and underscored substantial heterogeneity across regions and study designs [3]. More recent syntheses continue to report estimates around 3.5–3.7%, reinforcing that POI is not rare in reproductive-age populations. For health systems such as Nigeria’s, serving a large, youthful population, this translates into a sizeable absolute number of affected women, many of whom may be lost to follow-up or misclassified as having “functional” amenorrhoea or stress-related menstrual disturbances [4].
Aetiologies are heterogeneous and include genetic (e.g., X-chromosomal abnormalities, FMR1 premutation), autoimmune ovarian damage, iatrogenic causes (chemotherapy, radiotherapy, oophorectomy), infections and idiopathic forms. Regardless of cause, the downstream health sequelae are multi-systemic. Without timely diagnosis and appropriate hormone therapy until the average age of natural menopause, women with POI face elevated risks of low bone mineral density and fractures, adverse cardiometabolic profiles and potential cognitive and sexual-health impacts, alongside significant psychosocial distress. Current evidence and clinical guidance therefore recommend individualized counselling, cardiovascular and bone-health risk reduction, mental-health support and fertility counselling (including options such as oocyte donation) integrated into routine care [2,5].
Despite its burden, POI frequently goes unrecognized or is diagnosed late. Guidelines and reviews repeatedly note diagnostic delays attributable to symptom variability, low awareness among patients (and sometimes providers), and the misconception that menstrual irregularity in adolescents and young adults is “benign” or self-limiting. Such delays reduce the window to protect bone mass, optimize cardiometabolic health, and engage in timely fertility and psychosocial counselling. Evidence also links longer time to diagnosis with lower bone mass, highlighting a modifiable pathway of harm through earlier recognition and treatment. These realities justify public-facing education and provider training, particularly in settings where routine reproductive-endocrine evaluation is less accessible [6,7].
In Nigeria, empirical work on POI specifically, especially population-based assessments of knowledge, attitudes and perceptions (KAP), remains scarce. However, adjacent literature on menopause and infertility awareness reveals important gaps that likely generalize to POI. Studies in tertiary facilities and community samples have documented variable or low awareness of menopausal health and limited understanding of available treatments and assisted reproductive technologies; these findings suggest that many women may not recognize POI symptoms early or may hold misconceptions about its causes and management [8-10]. Against this backdrop, and given the stigma and psychosocial burden documented for infertility and reproductive disorders more broadly, there is a pressing need to generate Nigeria-specific evidence on women’s knowledge, attitudes and perceptions toward POI to inform context-appropriate health education and service delivery strategies.
The convergence of (i) non-trivial prevalence, (ii) significant multisystem sequelae, (iii) preventable harm from delayed diagnosis, and (iv) likely awareness gaps in Nigerian contexts creates a compelling rationale for a focused KAP study among Nigerian women. Such evidence can guide locally resonant communication strategies, refine primary-care and gynecology referral pathways, and support national policy on adolescent and women’s health, including integration with fertility services and bone- and heart-health screening protocols consistent with international guidance. This study, thus, assessed the knowledge, attitude, and perception (KAP) regarding POI among Nigerian women.
MATERIALS AND METHODS
Study Design
A hospital-based descriptive cross-sectional study design was employed to assess the knowledge, attitude, and perception (KAP) towards premature ovarian insufficiency (POI) among Nigerian women attending gynecology and related outpatient clinics at ABSUTH. This design was chosen because it enables the collection of data at a single point in time to determine the current status of awareness, beliefs, and attitudes toward POI in the target population.
Study Area
This study was conducted at the Abia State University Teaching Hospital (ABSUTH), Aba, located in Aba South Local Government Area of Abia State, Nigeria. ABSUTH is a tertiary healthcare facility that serves as a referral center for primary and secondary health institutions within Abia State and neighboring states, including Imo, Rivers, Akwa Ibom, and Cross River. The hospital provides a wide range of medical, surgical, obstetric, gynecologic, and diagnostic services. The Obstetrics and Gynecology Department, which served as the primary site for this research, offers antenatal, postnatal, family planning, and gynecological outpatient services, in addition to managing specialized clinics for infertility, menopause, and other reproductive health concerns.
Study Population
The study population comprised Nigerian women aged 18–49 years who presented at the gynaecology outpatient clinic or were admitted to the gynecology wards during the study period. The target group included women in the reproductive age bracket, as POI is defined as the cessation of ovarian function before the age of 40 years.
Inclusion and Exclusion Criteria
Inclusion criteria
Exclusion criteria
Sample Size Determination
The sample size was calculated based on Cochran’s formula for population proportion estimation, following the methodology described by Ezebuiro et al. [11]:
n = Z2(Pq)e2
The formula components are defined as follows:
A recent study conducted by Agaba et al. [12] reports the prevalence of POI in Nigerian women as 22.9%
P = 22.9% = 0.229
q = 1 – 0.229
= 0.771
n = 1.962(0.229 x 0.771)(0.05)2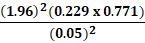
n = 3.8416 x (0.1766)0.0025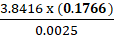
n = 0.67830.0025 = 271.31
= 271.31
Although the initially calculated minimum sample size was 271, it was increased to 300 to accommodate an anticipated 10% rate of non-response.
Sampling Technique
A systematic random sampling technique was employed. Daily laboratory registers at Federal Medical Centre, Umuahia were used as the sampling frame, and every 3rd eligible participant was selected until the required sample size was achieved. The sampling interval (3) was determined by dividing the average daily number of eligible patients by the daily recruitment target as described by Akwuruoha et al. [13].
Sampling Technique
A systematic random sampling method was employed. The outpatient register was used as a sampling frame. Based on the average daily clinic attendance, every 3rd eligible woman was invited to participate until the desired sample size was attained. For inpatients, eligible participants were recruited consecutively.
Study Instrument
Data was collected using a pretested, semi-structured interviewer-administered questionnaire developed based on literature review and adapted from previously validated KAP studies on reproductive health disorders. The instrument was divided into four sections:
The questionnaire was pretested among 30 women in a similar setting outside the study site to assess clarity, validity, and reliability. Necessary modifications were made based on feedback. Cronbach’s alpha for internal consistency was 0.82, indicating good reliability.
Data Collection Procedure
Data collection was carried out over a period of eight weeks by a team of four trained research assistants who were healthcare professionals with experience in questionnaire administration. Each participant was approached in the waiting area, and the study objectives were explained in detail. Informed consent was obtained before commencing the interview. Privacy was ensured during the interview process to encourage honest responses.
Variables
Dependent Variables
Independent Variables
Data Management and Analysis
Data collected were coded and entered into IBM SPSS Statistics version 27 for analysis. Descriptive statistics (frequencies, percentages, means, and standard deviations) were used to summarize variables. Knowledge scores were computed based on correct responses, with a cut-off of ≥50% correct answers considered adequate knowledge. Attitude and perception scores were generated from Likert-scale items, with mean scores used to classify responses into positive/favorable and negative/unfavorable categories. Inferential statistics included: Chi-square test for associations between categorical variables, Independent t-test for comparing mean scores between groups. Logistic regression to identify independent predictors of adequate knowledge, positive attitude, and favorable perception. Statistical significance was set at p < 0.05.
Ethical Considerations
Written informed consent was obtained from each participant before enrollment. Anonymity and confidentiality were maintained by using unique identification codes instead of personal names. Participation was voluntary, and participants could withdraw from the study at any stage without consequences.
RESULTS
The study involved 300 participants, most of whom were aged 35–39 years (24.67%), married (62.00%), had tertiary education (48.33%), and resided in urban areas (63.00%). The majority were of Igbo ethnicity (76.00%), with traders (29.67%) and civil servants (24.67%) forming the largest occupational groups (Table 1).
Regarding knowledge, less than half (47.00%) had heard of premature ovarian insufficiency (POI), and only 42.67% demonstrated adequate knowledge (≥50% score). Awareness was highest for infertility as a complication (62.67%), while knowledge of causes (32.33%) and risk factors like smoking/alcohol (27.33%) was low (Table 2).
Attitudinally, most respondents agreed that POI is a serious reproductive health problem (73.00%) and that affected women should seek early treatment (79.00%). However, fewer believed it could be prevented through lifestyle changes (57.67%) or that discussing POI is important to reduce stigma (70.34%) (Table 3).
In terms of perception, just over half (53.00%) had a favourable view. Most said they would promptly seek medical care if diagnosed (78.33%), but fewer felt personally at risk (34.33%) or thought community awareness was adequate (28.33%) (Table 4).
Overall, mean knowledge, attitude, and perception scores were 46.72 ± 18.54, 3.72 ± 0.81, and 3.48 ± 0.93, respectively, with higher proportions showing positive attitudes (57.00%) and favourable perceptions (53.00%) than adequate knowledge (42.67%) (Table 5).
Correlation analysis revealed significant positive associations between all KAP domains, with the strongest relationship between attitude and perception (r = 0.529, p < 0.001) (Table 6). Chi-square tests indicated that age, education, occupation, marital status, and family history of early menopause were significantly associated with one or more KAP categories (Table 7).
Table 1: Sociodemographic Characteristics of Participants
|
Variable |
Frequency (n = 300) |
Percentage (%) |
|
Age Group (years) |
||
|
18–24 |
47 |
15.67 |
|
25–29 |
58 |
19.33 |
|
30–34 |
66 |
22.00 |
|
35–39 |
74 |
24.67 |
|
40–45 |
55 |
18.33 |
|
Marital Status |
||
|
Single |
79 |
26.33 |
|
Married |
186 |
62.00 |
|
Divorced/Separated |
21 |
7.00 |
|
Widowed |
14 |
4.67 |
|
Educational Level |
||
|
No formal education |
12 |
4.00 |
|
Primary |
41 |
13.67 |
|
Secondary |
102 |
34.00 |
|
Tertiary |
145 |
48.33 |
|
Occupation |
||
|
Unemployed |
58 |
19.33 |
|
Trader |
89 |
29.67 |
|
Civil servant |
74 |
24.67 |
|
Artisan |
46 |
15.33 |
|
Professional |
33 |
11.00 |
|
Ethnicity |
||
|
Igbo |
228 |
76.00 |
|
Yoruba |
27 |
9.00 |
|
Hausa |
21 |
7.00 |
|
Others |
24 |
8.00 |
|
Residence |
||
|
Urban |
189 |
63.00 |
|
Rural |
111 |
37.00 |
Table 2: Knowledge about Premature Ovarian Insufficiency
|
Knowledge Item |
Frequency (n = 300) |
Percentage (%) |
|
Heard of POI before |
141 |
47.00 |
|
Knows that POI can occur before age 40 |
132 |
44.00 |
|
Correctly identifies at least 2 symptoms |
119 |
39.67 |
|
Aware of common causes (autoimmune, genetic, iatrogenic) |
97 |
32.33 |
|
Knows infertility is a complication |
188 |
62.67 |
|
Knows about hormonal therapy as treatment |
104 |
34.67 |
|
Identifies that smoking/alcohol can increase risk |
82 |
27.33 |
|
Knows diagnostic tests (FSH, estradiol) |
88 |
29.33 |
|
Adequate Knowledge (≥50% score) |
128 |
42.67 |
|
Inadequate Knowledge (<50% score) |
172 |
57.33 |
Table 3: Attitude towards POI (n = 300)
|
Statement |
Strongly Agree n (%) |
Agree n (%) |
Neutral n (%) |
Disagree n (%) |
Strongly Disagree n (%) |
|
POI is a serious reproductive health problem |
102 (34.00) |
117 (39.00) |
51 (17.00) |
20 (6.67) |
10 (3.33) |
|
Women with POI should seek early treatment |
124 (41.33) |
113 (37.67) |
33 (11.00) |
20 (6.67) |
10 (3.33) |
|
POI can be prevented through healthy lifestyle |
77 (25.67) |
96 (32.00) |
68 (22.67) |
41 (13.67) |
18 (6.00) |
|
Talking about POI is important to reduce stigma |
89 (29.67) |
122 (40.67) |
54 (18.00) |
23 (7.67) |
12 (4.00) |
Table 4: Perception about POI (n = 300)
|
Statement |
Strongly Agree n (%) |
Agree n (%) |
Neutral n (%) |
Disagree n (%) |
Strongly Disagree n (%) |
|
I am at risk of developing POI |
39 (13.00) |
64 (21.33) |
102 (34.00) |
59 (19.67) |
36 (12.00) |
|
POI would negatively affect marital life |
84 (28.00) |
117 (39.00) |
56 (18.67) |
26 (8.67) |
17 (5.67) |
|
If diagnosed, I would seek medical care promptly |
126 (42.00) |
109 (36.33) |
37 (12.33) |
20 (6.67) |
8 (2.67) |
|
Community awareness about POI is adequate |
31 (10.33) |
54 (18.00) |
79 (26.33) |
82 (27.33) |
54 (18.00) |
Table 5: Overall KAP Scores
|
Component |
Mean ± SD |
Category |
Frequency (n = 300) |
Percentage (%) |
|
Knowledge Score |
46.72 ± 18.54 |
Adequate |
128 |
42.67 |
|
Inadequate |
172 |
57.33 |
||
|
Attitude Score |
3.72 ± 0.81 |
Positive |
171 |
57.00 |
|
Negative |
129 |
43.00 |
||
|
Perception Score |
3.48 ± 0.93 |
Favourable |
159 |
53.00 |
|
Unfavourable |
141 |
47.00 |
Table 6: Correlation Analysis of KAP Scores (n = 300)
|
Variables |
r |
p-value |
|
Knowledge vs. Attitude |
0.412 |
<0.001 |
|
Knowledge vs. Perception |
0.368 |
<0.001 |
|
Attitude vs. Perception |
0.529 |
<0.001 |
Table 7: Chi-Square Analysis between Sociodemographic Variables and KAP Categories
|
Variable |
χ² |
df |
p-value |
|
Age group × Knowledge category |
12.84 |
5 |
0.025 |
|
Marital status × Attitude category |
14.29 |
3 |
0.002 |
|
Educational level × Knowledge category |
27.51 |
3 |
<0.001 |
|
Occupation × Perception category |
10.73 |
4 |
0.030 |
|
Family history of early menopause × Knowledge category |
8.64 |
1 |
0.003 |
DISCUSSION
The sociodemographic data show that the majority of participants were aged between 30–39 years (46.7%), primarily married (62%), possessed tertiary education (48.3%), and resided in urban areas (63%). The high representation of educated, urban-dwelling women suggests a potentially elevated baseline awareness, which may influence KAP (knowledge, attitude, perception) results. This demographic pattern aligns with similar Nigerian reproductive health surveys, such as those on family planning, where urban and educated women were found to have higher knowledge and more favorable attitudes [14].
Knowledge levels about POI were moderate: 47% had heard of POI, 44% knew it could occur before age 40, and only 42.7% scored adequately overall. While knowledge about infertility as a POI complication (62.7%) was relatively high, awareness of risk factors (smoking/alcohol: 27.3%) and diagnostic measures (29.3%) lagged considerably. These findings mirror regional patterns in reproductive health literacy; for example, a study on cervical cancer in South Africa also revealed awareness of the disease, but significant deficits in specific understanding and screening knowledge [15]. Moreover, in LMIC surveys on COVID-19 in Nigeria and Egypt, education level strongly correlated with better knowledge, a trend reflected here, where tertiary education was significantly associated with adequate POI knowledge (χ² = 27.51, p < 0.001) [16].
The attitude findings were encouraging: 73% recognized POI as a serious reproductive issue, and nearly 80% believed in early treatment. Furthermore, over two-thirds supported prevention through lifestyle and acknowledged the importance of discussing POI to reduce stigma. These attitudes are consistent with other Nigerian reproductive studies where positive attitudes toward family planning were commonly reported (e.g., 93.8% positive attitude toward family planning in Ebonyi State) [14]. Notably, marital status strongly correlated with attitude (χ² = 14.29, p = 0.002), possibly reflecting that married women, driven by fertility concerns, are more likely to perceive reproductive conditions as serious and “seek early treatment.”
Perception results were mixed. While a majority acknowledged the potential negative impact of POI on marital life (67%) and expressed a readiness to seek medical care if diagnosed (78.3%), only 34.3% felt personally at risk, and a substantial 45.3% believed community awareness was inadequate. Such disparity, where individuals recognize importance yet feel insulated and undervalue communal knowledge, echoes findings in infertility-related stigma literature: in Africa, infertility often carries heavy social stigma and is widely misunderstood [17,18]. This suggests that, although personal readiness to act is strong, broader perception of community awareness remains low, a gap requiring targeted public-health messaging.
The overall KAP scores reveal an imbalance: 57.3% had inadequate knowledge, while more than half exhibited positive attitudes (57%) and favorable perceptions (53%). This discrepancy highlights a common phenomenon in health literacy: positive attitudes and perceived susceptibility can exist even when factual understanding is limited. In support, a West African COVID-19 study similarly found that positive attitudes sometimes outpaced actual knowledge levels [19].
Robust and statistically significant correlations between knowledge and attitude (r = 0.412), knowledge and perception (r = 0.368), and attitude and perception (r = 0.529) were observed (all p < 0.001). These moderate to strong correlations affirm theoretical models like the Knowledge-Attitude-Practice framework, underscoring that increased knowledge positively impacts attitudes and perceptions. Comparable correlation strengths have been reported in KAP studies on other health issues in Nigeria and elsewhere [16,19].
Chi-square analysis further highlighted that younger age groups and those with lower education were more likely to have inadequate knowledge, reinforcing the notion that younger and less educated women are more vulnerable to knowledge gaps in reproductive health. Interestingly, occupation was associated with perception (χ² = 10.73, p = 0.030), implying that economic and social roles, such as being a trader or professional, modulate how women perceive their risk and the seriousness of POI. Lastly, having a family history of early menopause significantly predicted better knowledge (χ² = 8.64, p = 0.003), suggesting that personal or familial experience drives awareness.
Comparatively, data on POI knowledge, attitude, and perception in Nigerian populations remains scarce, making direct comparisons difficult. However, several studies in other LMIC contexts reveal similar trends: for instance, a qualitative study among Iranian women with POI demonstrated significant psychological distress and lack of awareness, emphasizing how knowledge deficits contribute to emotional suffering [20]. Among healthcare providers in Brazil, about 53% correctly diagnosed POI, while fewer than 10% demonstrated full etiological understanding [21]. This data confirms that both laywomen and even professionals exhibit limited knowledge about POI globally.
Although Nigerian women generally have positive attitudes and favorable perceptions toward POI, knowledge gaps are evident, particularly regarding risk factors, diagnosis, and prevention. Education level, age, marital status, occupation, and family history consistently influence KAP outcomes. This suggests that public-health interventions must prioritize tailored educational content, focusing not only on raising awareness but also on imparting actionable knowledge about POI.
CONCLUSION
This study highlights significant knowledge deficiencies regarding POI among Nigerian women, despite generally positive attitudes and perceptions. Enhancing educational outreach, alongside reinforcing provider training, will be vital in addressing POI awareness, reducing misconceptions, and supporting reproductive health among Nigerian women.