International Journal of Clinical Gynaecology and Obstetrics
OPEN ACCESS | Volume 3 - Issue 1 - 2025
ISSN No: 2836-0737 | Journal DOI: 10.61148/2836-0737/IJCGO
C. O. Onyemereze 1, A. K. Eze 1, O. O. Adesina 2, I. O. Abali 3, E. O. Ezirim 1, E. M. Akwuruoha 1, K. K. Mba 4, C. J. Mba 4 and A. I. Airaodion 5*
1 Department of Obstetrics and Gynaecology, Abia State University Teaching Hospital, Aba, Nigeria
2Department of Medical Laboratory Science, Babcock University, Ilishan. Ogun State, Nigeria
3Department of Surgery, Abia State University, Uturu, Nigeria
4Department of Physiology, Abia State University, Uturu, Nigeria
5Department of Biochemistry, Lead City University, Ibadan, Oyo State, Nigeria
*Corresponding author: Airaodion A. I., Department of Biochemistry, Lead City University, Ibadan, Oyo State, Nigeria.
Received: November 29, 2024
Accepted: December 06, 2024
Published: December 10, 2024
Citation: Airaodion A. I., C. O. Onyemereze, A. K. Eze, O. O. Adesina, I. O. Abali, E. O. Ezirim, E. M. Akwuruoha, K. K. Mba, C. J. Mba. (2024). “Predictors of Vaginal Bleeding and Birth Outcome among Expectant Mothers in a Tertiary Health Facility in Southeast Nigeria”. International J of Clinical Gynaecology and Obstetrics, 4(2); DOI: 10.61148/ 2766-8614 /IJCGO/039
Copyright: © 2024 Airaodion A. I. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background:
Vaginal bleeding in early pregnancy is a significant concern that may impact maternal and fetal outcomes. This study evaluates the predictors of vaginal bleeding and birth outcomes among expectant mothers in a tertiary health facility in Southeast Nigeria.
Materials and Methods:
A prospective descriptive study was conducted from January 2021 to December 2022. Data were collected from 3893 participants <20 weeks gestation using structured questionnaires and hospital records. Participants were categorized into two groups: those with vaginal bleeding and those without. Predictors of vaginal bleeding were analyzed using chi-square tests, with p<0.05 considered significant.
Results:
The prevalence of vaginal bleeding was 23.5% (914/3893). Significant predictors included the use of herbal remedies or non-prescribed medications (p=0.016), irregular antenatal attendance (p=0.030), engagement in strenuous physical activities (p=0.008), and pre-existing medical conditions (p=0.002). Women with vaginal bleeding had higher rates of preterm deliveries (58.21% vs. 3.93%) and lower packed cell volume (PCV) and iron levels compared to those without bleeding (p=0.031 and p=0.009, respectively).
Conclusion:
Predictors such as the use of non-prescribed medications, irregular antenatal care, physical strain, and pre-existing conditions are associated with vaginal bleeding in early pregnancy. This underscores the need for early antenatal interventions and education to improve maternal and birth outcomes.
Introduction:
Pregnancy is a complex physiological process influenced by numerous factors that can have significant implications for maternal and fetal outcomes. Vaginal bleeding during pregnancy is a critical obstetric condition that can arise from various causes and is a significant predictor of adverse birth outcomes, including preterm delivery, low birth weight, and perinatal mortality (Hinkle et al., 2020). Understanding the predictors of vaginal bleeding and their relationship with birth outcomes is essential for effective prenatal care, particularly in resource-limited settings such as Southeast Nigeria.
Vaginal bleeding during pregnancy can occur at any trimester and may signal complications that require immediate medical intervention. Bleeding in the first trimester is often associated with implantation, ectopic pregnancy, or miscarriage, while bleeding in the second and third trimesters is frequently linked to placenta previa, placental abruption, or preterm labor (Ahmed et al., 2022). The prevalence of vaginal bleeding varies globally, with higher rates reported in low- and middle-income countries (LMICs) due to disparities in healthcare access and quality (Khan et al., 2021). Early identification and management of risk factors associated with vaginal bleeding are crucial to improving maternal and neonatal outcomes.
Birth outcomes, including gestational age, birth weight, and neonatal survival, are influenced by maternal health, environmental factors, and healthcare interventions. Adverse outcomes such as preterm birth, intrauterine growth restriction, and stillbirth are more prevalent in LMICs, where access to antenatal care is often suboptimal (World Health Organization [WHO], 2023). Vaginal bleeding during pregnancy is a well-documented risk factor for poor birth outcomes. Studies have shown that even minor bleeding episodes can compromise placental function, leading to inadequate fetal growth and development (Ayalew et al., 2021).
In Nigeria, the burden of adverse maternal and neonatal outcomes remains a public health concern. The maternal mortality ratio in Nigeria is among the highest globally, with hemorrhagic complications being a leading cause (National Population Commission [NPC] & ICF, 2019). Southeast Nigeria, in particular, faces unique challenges related to healthcare infrastructure, cultural practices, and socioeconomic disparities, which contribute to poor pregnancy outcomes (Onoh et al., 2020). Vaginal bleeding during pregnancy in this region is often underreported due to stigma and limited access to skilled healthcare providers, exacerbating its impact on maternal and fetal health.
Predictors of vaginal bleeding include maternal age, parity, prior obstetric history, and underlying medical conditions such as hypertension and infections (Ezeama et al., 2022). Behavioral factors, such as smoking and inadequate antenatal care, also play a role (Hinkle et al., 2020). In the context of Southeast Nigeria, socioeconomic factors such as poverty, limited education, and lack of access to emergency obstetric care further compound the risk.
Despite the known association between vaginal bleeding and adverse birth outcomes, there is a paucity of region-specific data in Southeast Nigeria. Existing studies often focus on isolated predictors without exploring their combined effects or their relationship with healthcare practices and birth outcomes. This research aims to bridge this gap by identifying predictors of vaginal bleeding and their implications for birth outcomes among expectant mothers in a tertiary health facility in Southeast Nigeria. Such evidence is critical for developing targeted interventions and policies to improve maternal and neonatal health in the region.
This study is significant for several reasons. First, it contributes to the growing body of evidence on maternal health challenges in LMICs, providing context-specific data for Southeast Nigeria. Second, it informs clinical practice by highlighting modifiable risk factors that healthcare providers can address during antenatal care. Third, the findings can guide policymakers in allocating resources and designing interventions to reduce the burden of adverse birth outcomes associated with vaginal bleeding.
Materials and Methods:
Study Design:
This prospective descriptive study was carried out for two years, from January 2021 to December 2022. All patients <20 weeks gestation who attended the antenatal clinic or who presented to the emergency department were included in this study. Data were collected using a structured, interviewer-administered questionnaire, as well as from the antenatal outpatient department registration record, emergency department registration record, and hospital medical records. About 3893 participants were recruited for this study. Participants were assured of the confidentiality of their responses, and data was anonymized to protect their identity. Informed consent was obtained from all participants, and they were informed of their right to withdraw from the study at any time without any consequences to their medical care. Participants were divided into the following two groups:
• Women with vaginal bleeding in early pregnancy (<20 weeks)
• Women without vaginal bleeding in early pregnancy (<20 weeks).
Inclusion criteria:
Singleton pregnancy complicated with vaginal bleeding <20 weeks gestation.
Exclusion criteria:
1. Multiple pregnancy
2. Chronic hypertension
3. Local cervical pathology such as erosion and polyp
Statistical Analysis:
The collected data was analyzed using the Microsoft Excel (2019 version). Descriptive statistics such as frequencies and percentages were used to summarize the demographic characteristics and prevalence and severity of vaginal bleeding. Chi‑square test was used to compare the predictors of vaginal bleeding and values were considered significantly different at p<0.05.
Results:
The socio-demographic profile (Table 1) shows that the majority of participants (54.79%) were aged between 30–39 years, while only 3.57% were below 20 years. Educational attainment was relatively high, with 64.14% having secondary education and 25.76% attaining tertiary education. Most participants (95.38%) were married, reflecting the predominance of stable family units. Regarding employment, 45.7% were public sector employees, followed by private sector employees (23.94%) and self-employed individuals (22.19%). Students and the unemployed represented 4.98% and 3.19% of the population, respectively.
Table 2 outlines the obstetric history of participants. A significant proportion (46.62%) had been pregnant 2–3 times, with fewer reporting more than five pregnancies (1.44%). Regarding parity, 31.26% had delivered 2–3 times, while 28.74% had no deliveries. Vaginal bleeding during previous pregnancies was reported by 22.17%, while 50.37% did not experience it, and 27.46% found the question inapplicable, likely due to no prior pregnancies.
Key predictors of vaginal bleeding are identified in Table 3. The use of herbal remedies or non-prescribed medications was significantly associated with vaginal bleeding (17.94% vs. 6.98%, p = 0.016). Similarly, rare antenatal care attendance was more common among those with vaginal bleeding (37.31%) compared to those without (4.30%, p = 0.030). Strenuous physical activity also had a strong association, reported by 42.01% of participants with vaginal bleeding compared to 23.73% without (p = 0.008). Pre-existing medical conditions were another significant predictor (35.45% vs. 16.38%, p = 0.002).
Figure 1 illustrates that vaginal bleeding had a profound impact on pregnancy outcomes. Among participants who experienced vaginal bleeding, 58.21% delivered preterm, compared to only 3.93% in the non-bleeding group. Conversely, 96.07% of pregnancies without bleeding reached term, while this was true for only 41.79% of those with bleeding. This underscores the adverse effect of vaginal bleeding on pregnancy duration.
Table 4 demonstrates the detrimental impact of vaginal bleeding on hematological parameters. Pregnant women with vaginal bleeding had significantly lower packed cell volume (PCV) levels (28±7.67%) compared to those without bleeding (34±5.33%, p = 0.031). Iron levels were also substantially reduced among those with vaginal bleeding (11.06±4.10 μmol/L) relative to the non-bleeding group (19.77±3.24 μmol/L, p = 0.009), indicating a heightened risk of anemia in this subgroup.
|
Socio-Demographic Information |
Frequency (n = 3893) |
Percentage (%) |
|
Age (in Years) |
|
|
|
Below 20 |
139 |
3.57 |
|
20-29 |
993 |
25.51 |
|
30-39 |
2133 |
54.79 |
|
40 and above |
628 |
16.13 |
|
Educational Level |
|
|
|
No formal Education |
78 |
2.00 |
|
Primary Education |
315 |
8.09 |
|
Secondary Education |
2497 |
64.14 |
|
Tertiary Education |
1003 |
25.76 |
|
Marital Status |
|
|
|
Single |
62 |
1.59 |
|
Married |
3713 |
95.38 |
|
Divorced/Widowed |
118 |
3.03 |
|
Employment Status |
|
|
|
Unemployed |
124 |
3.19 |
|
Self-employed |
864 |
22.19 |
|
Private sector employee |
932 |
23.94 |
|
Public sector employee |
1779 |
45.70 |
|
Student |
194 |
4.98 |
Table 1: Socio-Demographic Information of Participants
|
Variable |
Frequency (n = 3893) |
Percentage (%) |
|
How many times have you been pregnant including this present one (gravida)? |
|
|
|
1 |
1069 |
27.46 |
|
2-3 |
1815 |
46.62 |
|
4-5 |
953 |
24.48 |
|
More than 5 |
56 |
1.44 |
|
How many deliveries have you had (parity)? |
|
|
|
None |
1119 |
28.74 |
|
1 |
1022 |
26.25 |
|
2-3 |
1217 |
31.26 |
|
4 or more |
535 |
13.74 |
|
Did you experience vaginal bleeding during previous pregnancies? |
|
|
|
Yes |
863 |
22.17 |
|
No |
1961 |
50.37 |
|
Not Applicable |
1069 |
27.46 |
Table 2: Obstetric History of Participants
|
Variable |
Vaginal Bleeding (n = 914) |
No Vaginal Bleeding (n = 2979) |
p-value |
|||
|
Frequency |
Percentage (%) |
Frequency |
Percentage (%) |
|
||
|
Age (in Years) |
|
|
|
|
0.541 |
|
|
Below 20 |
38 |
4.16 |
101 |
3.39 |
||
|
20-29 |
247 |
27.02 |
746 |
25.04 |
||
|
30-39 |
505 |
55.25 |
1628 |
54.65 |
||
|
40 and above |
124 |
13.57 |
504 |
16.92 |
||
|
Do you smoke or use tobacco products? |
|
|
|
|
0.891 |
|
|
Yes |
3 |
0.33 |
08 |
0.27 |
||
|
No |
911 |
99.67 |
2971 |
99.73 |
||
|
Do you consume alcohol? |
|
|
|
|
0.725 |
|
|
Yes |
21 |
2.30 |
38 |
1.28 |
||
|
No |
893 |
97.70 |
2941 |
98.72 |
||
|
Do you take any herbal remedies or non-prescribed medications? |
|
|
|
|
0.016* |
|
|
Yes |
164 |
17.94 |
208 |
6.98 |
||
|
No |
750 |
82.06 |
2771 |
93.02 |
||
|
How often do you attend antenatal care? |
|
|
|
|
0.030* |
|
|
Weekly |
104 |
11.38 |
585 |
19.64 |
||
|
Every two weeks |
347 |
37.96 |
732 |
24.57 |
||
|
Monthly |
122 |
13.35 |
1534 |
51.49 |
||
|
Rarely |
341 |
37.31 |
128 |
4.30 |
||
|
Do you engage in strenuous physical activities or heavy lifting? |
|
|
|
|
0.008* |
|
|
Yes |
384 |
42.01 |
707 |
23.73 |
||
|
No |
530 |
57.99 |
2272 |
76.27 |
||
|
Do you have access to clean water and sanitation? |
|
|
|
|
0.067 |
|
|
Yes |
722 |
78.99 |
2012 |
67.54 |
||
|
No |
192 |
21.01 |
967 |
32.46 |
||
|
Do you have any pre-existing medical conditions? (e.g., hypertension, diabetes) |
|
|
|
|
0.002* |
|
|
Yes |
324 |
35.45 |
488 |
16.38 |
||
|
No |
590 |
64.55 |
2491 |
8362 |
||
Table 3: Predictors of Vaginal Bleeding
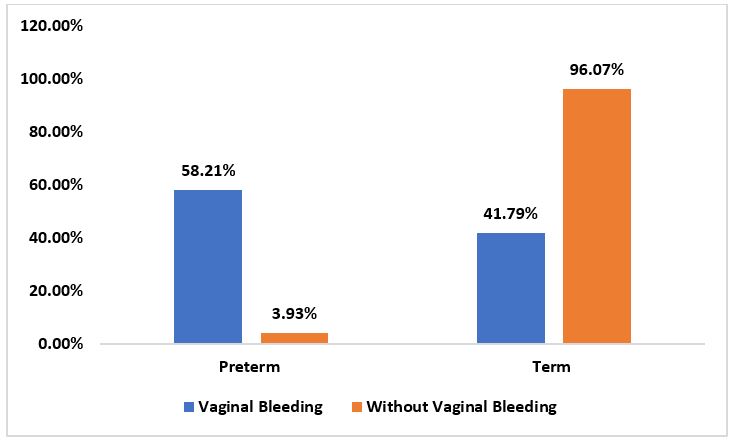
Figure 1: Pregnancy Outcome
|
Variable |
Vaginal Bleeding (n = 914) |
No Vaginal Bleeding (n = 2979) |
p-value |
|
PCV (%) |
28± |
34± |
0.031* |
|
Iron (umol/L) |
11.06±4 |
19.77± |
0.009* |
Table 4: Effect of Vaginal Bleeding on Packed Cell Volume (PCV) and Iron Level of Pregnant Women
Discussion:
The socio-demographic characteristics of participants in this study reveal a population primarily aged 30–39 years (54.79%), with a high level of secondary education (64.14%) and a predominance of married individuals (95.38%). This finding aligns with studies conducted by Ndubuisi et al. (2022) and Ibeh et al. (2021), who reported that the majority of expectant mothers accessing tertiary health facilities in Southeast Nigeria are within their reproductive peak (30–39 years) and have at least secondary education. High marital prevalence may also indicate that married women are more likely to seek antenatal care in tertiary facilities.
A significant proportion of participants (22.17%) experienced vaginal bleeding during prior pregnancies. Previous studies, such as those by Adeleke et al. (2023), corroborate this prevalence of vaginal bleeding in 20%–25% of pregnancies in sub-Saharan Africa. Gravidity and parity distributions suggest that multigravida and multiparous women are predominant, consistent with findings by Obianyo et al. (2020), which associated higher gravidity and parity with increased antenatal care utilization in Nigeria.
Participants who used herbal remedies or non-prescribed medications were significantly more likely to experience vaginal bleeding (p = 0.016). This is consistent with findings from studies by Anozie et al. (2022) and Okonkwo and Umeora (2021), which identified the use of unregulated herbal products as a risk factor for vaginal bleeding and other pregnancy complications due to their potential uterotonic or anticoagulant effects.
Participants who rarely attended antenatal care were significantly more likely to report vaginal bleeding (p = 0.030). This finding aligns with studies by Adebayo and Olorunfemi (2023), which emphasized the protective role of consistent antenatal care in identifying and managing pregnancy complications early. Lack of regular antenatal care may lead to delayed diagnosis and treatment of conditions that predispose to vaginal bleeding.
Engaging in strenuous physical activities or heavy lifting was another significant predictor (p = 0.008), supporting evidence from Uchenna et al. (2021) that identified physical exertion as a modifiable risk factor for pregnancy complications, including vaginal bleeding and preterm labor.
Pre-existing medical conditions, such as hypertension and diabetes, were strongly associated with vaginal bleeding (p = 0.002). This aligns with studies by Onyeka et al. (2023) and Brown et al. (2022), which established a significant relationship between medical comorbidities and abnormal uterine bleeding during pregnancy.
The study revealed that vaginal bleeding was strongly associated with adverse pregnancy outcomes, particularly preterm deliveries (58.21% vs. 3.93%, p < 0.05). This is consistent with findings by Adeyemi et al. (2023), who reported that vaginal bleeding in early or mid-pregnancy doubles the risk of preterm birth. Furthermore, studies by Cunningham et al. (2022) suggest that vaginal bleeding is a key predictor of placental complications, which are often linked to preterm delivery.
Participants with vaginal bleeding had significantly lower packed cell volume (28±7.67%) and iron levels (11.06±4.10 μmol/L) compared to those without bleeding (34±5.33% and 19.77±3.24 μmol/L, respectively, p < 0.05). This corroborates findings by Olubunmi et al. (2021), which reported that vaginal bleeding during pregnancy leads to significant maternal anemia, often exacerbated by poor nutritional status and inadequate antenatal supplementation.
Conclusion:
This study revealed that vaginal bleeding in early pregnancy among expectant mothers in Nigeria is significantly associated with several predictors, including the use of herbal remedies, non-prescribed medications, infrequent antenatal care attendance, engagement in strenuous physical activities, and pre-existing medical conditions. Vaginal bleeding was also linked to adverse pregnancy outcomes such as preterm delivery and lower hematological parameters, including reduced packed cell volume and iron levels. These findings underscore the importance of identifying and addressing these risk factors to improve maternal and fetal outcomes.
Recommendations:
Strengthen Antenatal Care Services: Healthcare providers should emphasize the importance of regular antenatal visits to monitor and mitigate risk factors for vaginal bleeding and other complications in pregnancy.