International Journal of Clinical Cardiology and Cardiovascular Interventions
OPEN ACCESS | Volume 4 - Issue 1 - 2025
ISSN No: 2836-2837 | Journal DOI: 10.61148/2836-2837/IJCCI
Julio Echarte-Morales1*, Carlos Minguito-Carazo1, Pedro L. Cepas-Guillén2, Víctor Vallejo García3, Isabel Dolores Poveda Pinedo4, Eduardo Martínez Gómez5, Enrique Sánchez Muñoz1, María López Benito1, Anthony Salazar Rodríguez2, Ignacio Cruz-González3, Emilio Arbas Redondo4, Tomás Benito-González1, Joan Guzmán-Borfarull2, Daniel Tebar Máequez4, Ana Viana Tejedor5, Pedro Luis Sánchez Fernández3, Manel Sabaté2, Felipe Fernández-Vázquez1
1Department of Cardiology, Complejo Asistencial Universitario de León.
2Department of Cardiology, Instituto Cardiovascular, Hospital Clinic, IDIBAPS, Universidad de Barcelona.
3Department of Cardiology, Hospital Clínico de Salamanca.
4Department of Cardiology, Hospital Universitario La Paz.
5Department of Cardiology, Hospital Universitario Clínico San Carlos.
*Corresponding Author: Julio Echarte Morales, C/ Altos de Nava s/n, Servicio de Cardiología, Complejo Asistencial Universitario de León 24003 - León (Spain).
Received date: August 29, 2021
Accepted date: September 06, 2021
Published date: September 10, 2021
Citation: Julio Echarte-Morales, Carlos Minguito-Carazo, Pedro L. Cepas-Guillén, Víctor Vallejo García, Isabel Dolores Poveda Pinedo et al (2021) “Incidence, Morbidity-Mortality and Management of Acute Coronary Syndrome During the Covid-19 Pandemic.” International J of Clinical Cardiology and Cardiovascular Interventions, 2(4); DOI: http;//doi.org/04.2021/1.1020.
Copyright: © 2021 Julio Echarte-Morales. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background and objective: A decrease in the number of admissions due to acute coronary syndrome (ACS) was observed during the COVID-19 pandemic. A study is made of the impact of the pandemic upon the incidence, morbidity-mortality and management of ACS.
Materials and methods: A retrospective multicenter study was carried out with data from patients admitted due to ACS between 14 February and 24 June 2020. The following groups were established according to the period of admission: A) one month before strict lockdown; B) during lockdown; and C) one month after lockdown. The primary objective of the study was to assess differences in mortality among the three periods. Differences in the time from symptoms onset to the first medical contact (FMC) were also evaluated.
Results: A total of 634 patients were included in the study (group A: 205, group B: 303, group C: 126). A 41% decrease in the number of admissions due to ACS was recorded in the first month of lockdown. A diagnostic delay was observed during lockdown (A: 65 minutes (range 38-112) vs B: 120 minutes (60-300) vs C: 120 minutes (60-360), p < 0.001); this period was not associated to increased mortality, however (HR 1.26; 95%CI 0.53-2.97; p = 0.60).
Conclusions: A decrease in the number of admissions due to ACS was recorded during lockdown, with an increase in the time from symptoms onset to FMC in patients with STEACS. This was not associated to an increase in mortality during this period, however.
Introduction
In late December 2019, the Chinese authorities informed the World Health Organization of the first detected cases of pneumonia caused by a new coronavirus in the city of Wuhan [1,2]. Since then, the rapid spread of the disease led to the collapse of healthcare systems in many countries throughout the world, with the adoption of drastic preventive measures on the part of the authorities.
The pandemic caused by the SARS-CoV-2 virus (COVID-19 disease) has had a very important international social, economic and health impact. In the healthcare setting, the resulting organizational and patient care changes have often led to marked variations in the attention to and management of the rest of disease conditions [3–5]. In this regard, some studies have reported a decrease in the number of admissions due to cardiovascular disease, with a strong impact upon morbidity-mortality [6–8]. The care burden represented by COVID-19 and the consequent reduction of the quality of care, the lockdown periods, and the decrease in voluntary access to the healthcare resources, are some of the possible explanations for these changes. The present multicenter study was carried out to assess the incidence of admissions due to acute coronary syndrome (ACS) according to the different periods of the pandemic in Spain, as well as the impact upon the morbidity-mortality and management of patients with ACS.
Material and methods
Study population
A retrospective, multicenter observational study was carried out with data from patients admitted due to ACS between 14 February and 24 June 2020 in 5 different tertiary hospitals in Spain. Patients with ST-segment elevation acute coronary syndrome (STEACS) and non-ST-segment elevation acute coronary syndrome (NSTEACS) were included in the study. The patients were divided into three groups according to the period of hospital admission: group A (14 February to 14 March: one month before strict lockdown), group B (15 March to 24 May: during lockdown) and group C (25 May to 24 June 2020: one month after lockdown). The baseline characteristics of the patients were recorded, as well as the acute complications and cardiovascular events over follow-up such as mortality due to all causes, cardiovascular mortality, stroke, reinfarction, stent thrombosis and the need for repeat revascularization. In the patients with STEACS, we recorded the time from symptoms onset to the first medical contact (FMC), and from electrocardiographic diagnosis to reperfusion (guide advancement). Clinical follow-up was carried out until 25 July 2020 or death, with a minimum follow-up of 30 days. Data compilation was approved by the local Ethics Committee of each participating center.
Objectives
The primary objective of the study was to assess differences in mortality due to all causes among the three groups 30 days after the acute coronary event. The secondary objective was to evaluate differences in the combination of cardiovascular mortality, stroke, admission due to repeat ACS, stent thrombosis and the need for repeat revascularization. Post-infarction complications over follow-up, as well as left ventricular ejection fraction (LVEF) at discharge and the revascularization times (symptoms onset-FMC and diagnosis-reperfusion [guide advancement]) were likewise evaluated in a secondary analysis with comparison among the three groups. With regard to the revascularization times, and given the bias introduced by including STEACS with an evolution of over 24 hours in assessing the time from diagnosis to reperfusion, another sub-analysis was made excluding these patients.
Statistical analysis
Categorical variables were reported as numbers and percentages (in parentheses), and comparisons were made using the chi-square test or Fisher exact test, as applicable. Continuous variables were reported as the mean and standard deviation (SD) or as the median and interquartile range (IQR) in the absence of normal data distribution. The Shapiro-Wilks test was used to assess normal data distribution in the case of continuous variables, with comparisons being made by analysis of variance (ANOVA) for independent samples or the Kruskal-Wallis test (depending on whether the data exhibited a normal distribution or not) to evaluate differences among the three groups. Survival was analyzed from the Kaplan-Meier curves, and the differences were evaluated using the log-rank test. Cox proportional hazards regression analysis adjusted for age was used to assess the influence of belonging to group B (lockdown period) upon total patient mortality. The STATA version 15.1 statistical package was used throughout. Statistical significance was considered for p < 0.05.
Results
A total of 634 patients were enrolled in the study between 14 February 2020 and 24 June 2020. Of these patients, 205, 303 and 126 corresponded to groups A, B and C, respectively. Of the total subjects, 356 (56.2%) were admitted due to STEACS and 278 (43.8%) due to NSTEACS - 29.9% being diagnosed with unstable angina (UA) and the remaining 70.1% with non-ST-segment elevation myocardial infarction (NSTEMI). The baseline characteristics of the sample are shown in Table 1. The patients admitted during lockdown (group B) were younger (p = 0.012) and presented a lesser incidence of arterial hypertension (p = 0.027) and dyslipidemia (p = 0.008) than the patients admitted in the other two periods. On the other hand, these patients presented a lesser proportion of previous ischemic heart disease (p < 0.001) and previous coronary revascularization (p < 0.001). Likewise, we recorded a greater proportion of admissions due to STEACS, with a corresponding decrease in NSTEACS during this period, particularly at the expense of a decrease in the percentage diagnosis of UA with respect to total ACS (p = 0.003).
|
Variable |
Total |
Group A |
Group B |
Group C |
p-value |
|
Age (mean ± SD) |
66.3 ± 12.6 |
67.4 ± 11.6 |
64.8 ± 12.7 |
68.2 ± 13.6 |
0.012 |
|
Males, n (%) |
494 (77.9) |
158 (77.1) |
241 (79.5) |
95 (75.4) |
0.603 |
|
AHT, n (%) |
400 (63.1) |
143 (69.8) |
176 (58.1) |
81 (64.3) |
0.027 |
|
DM, n (%) |
191 (30.1) |
71 (35.1) |
89 (29.4) |
30 (23.8) |
0.086 |
|
DL, n (%) |
368 (58.0) |
137 (66.8) |
164 (54.1) |
67 (53.2) |
0.008 |
|
Smoking, n (%) |
364 (57.4) |
124 (60.5) |
182 (60.1) |
58 (46.0) |
0.015 |
|
PVD, n (%) |
36 (5.7) |
15 (7.3) |
16 (5.3) |
5 (4.0) |
0.405 |
|
CVA, n (%) |
37 (5.8) |
11 (5.4) |
16 (5.3) |
110 (7.9) |
0.531 |
|
CKD (GFR < 60), n (%) |
30 (4.7) |
18 (8.8) |
7 (2.3) |
5 (4.0) |
0.003 |
|
COPD, n (%) |
45 (7.1) |
14 (6.8) |
22 (7.3) |
9 (7.1) |
0.981 |
|
AF, n (%) |
40 (6.3) |
16 (7.8) |
16 (5.3) |
8 (6.4) |
0.517 |
|
IHD, n (%) |
150 (23.7) |
79 (38.5) |
46 (15.2) |
25 (19.8) |
< 0.001 |
|
AMI, n (%) |
103 (16.3) |
52 (25.4) |
31 (10.2) |
20 (15.9) |
< 0.001 |
|
PCI, n (%) |
117 (18.5) |
60 (29.3) |
36 (11.9) |
21 (16.7) |
< 0.001 |
|
CABG, n (%) |
23 (3.6) |
12 (5.9) |
7 (2.3) |
4 (3.2) |
0.112 |
|
Diagnosis |
|
|
|
|
|
|
UA, n (%) |
83 (13.1) |
36 (17.6) |
27 (8.9) |
20 (15.9) |
0.003 |
|
NSTEMI, n (%) |
195 (30.8) |
67 (32.7) |
83 (27.4) |
45 (35.7) |
0.003 |
|
STEACS, n (%) |
356 (56.2) |
102 (49.8) |
193 (63.7) |
61 (48.4) |
0.003 |
|
GRACE (mean ± SD) |
120.1 ± 35.6 |
118.4 ± 35.4 |
119.1 ± 34.6 |
124.8 ± 38.3 |
0.264 |
|
CRUSADE (mean ± SD) |
31.4 ± 13.8 |
34.1 ± 15.2 |
30.4 ± 13.3 |
29.7 ± 11.8 |
0.001 |
|
Catheterization |
616 (97.5) |
198 (96.6) |
295 (97.7) |
123 (98.4) |
0.565 |
|
Emergent |
375 (59.5) |
112 (54.9) |
190 (63.1) |
73 (58.4) |
0.447 |
|
Deferred |
242 (38.4) |
87 (42.7) |
105 (34.9) |
50 (40.0) |
0.447 |
|
Fibrinolysis |
29 (5.1) |
10 (5.7) |
13 (4.5) |
6 (6.1) |
0.652 |
|
PCI |
534 (94.3) |
165 (93.2) |
276 (95.2) |
93 (94.0) |
0.652 |
|
CABG |
29 (4.6) |
11 (5.4) |
8 (2.7) |
10 (8.1) |
0.045 |
|
Conservative management |
3 (0.5) |
2 (1.1) |
1 (0.3) |
0 (0) |
0.652 |
|
Complete revascularization |
456 (75.6) |
138 (74.6) |
223 (76.1) |
95 (76.0) |
0.926 |
Table 1: Baseline characteristics of the study sample
SD: standard deviation. AHT: arterial hypertension. DM: diabetes mellitus. DL: dyslipidemia. PVD: peripheral arterial disease. CVA: cerebrovascular accident (stroke). CKD: chronic kidney disease. COPD: chronic obstructive pulmonary disease. AF: atrial fibrillation. IHD: ischemic heart disease. AMI: acute myocardial infarction. PCI: percutaneous coronary intervention. CABG: coronary artery bypass grafting. UA: unstable angina. NSTEMI: non-ST-segment elevation myocardial infarction. STEACS: ST-segment elevation acute coronary syndrome.
Diagnostic coronary angiography was performed in 97.1% of the cohort, and proved emergent in 59.1% of the cases. There were no differences in the proportion of patients subjected to percutaneous coronary intervention (PCI) in the different periods (p = 0.652). However, a significant decrease was observed in the number of surgical coronary revascularizations performed during lockdown (group A: 5.4%, group B: 2.7%, group C: 8.1%; p = 0.045), including the subgroup of patients with left coronary trunk and/or triple-vessel disease (group A: 17.7%, group B: 5.5%, group C: 34.5%; p = 0.003).
There were a total of 205 admissions due to ACS during the 30-day period between the start of patient recruitment and the official declaration of lockdown. In turn, the number of admissions due to ACS was 120, 138 and 151 during the first, second and third periods of 30 days from the start of lockdown. This represented a decrease of 41%, 33% and 26% in the number of admissions due to ACS with respect to the figure recorded in the month prior to lockdown, for these same 30-day periods. (Figure 1).
Figure 1: Number of admissions due to ACS for every 30 days from the start of the study
ACS: acute coronary syndrome.
The median follow-up was 98 days (63-137). We recorded 36 deaths (5.7%), of which 22 (3.5%) were due to cardiovascular causes. There were no significant differences in mortality rate due to all causes after 30 days among the three groups (group A: 7.3%, group B: 4.3%, group C: 6.4%; p = 0.327). According to the Cox regression analysis, belonging to the lockdown group (group B) was not related to increased mortality due to all causes (HR 1.26; 95% CI 0.53-2.97; p = 0.60). Likewise, no differences in survival were recorded among the three groups (p log-rank test = 0.188) (Figure 2).
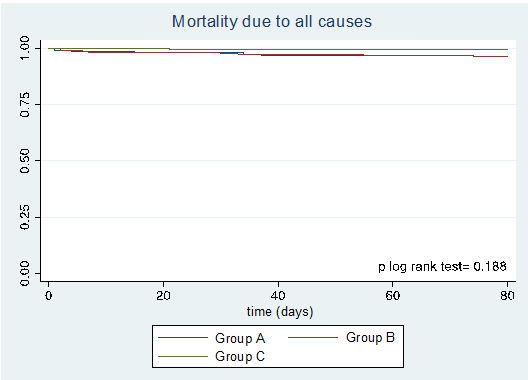
Figure 2: Kaplan-Meier survival curve corresponding to mortality due to all causes
No differences were observed in terms of the need for inotropic drugs, orotracheal intubation, noninvasive mechanical ventilation or renal replacement therapy. We only recorded an increased use of intraaortic balloon counterpulsation in the period prior to the declaration of lockdown. On the other hand, there likewise were no differences in the number of post-infarction complications (p = 0.774) or in the different arrhythmic events (Table 2).
|
Variable |
Total |
Group A (n = 205) |
Group B (n = 303) |
Group C (n = 126) |
p |
|
Mortality due to all causes, |
36 (5.7) |
15 (7.3) |
13 (4.3) |
8 (6.4) |
0.327 |
|
Cardiovascular mortality, |
22 (64.7) |
7 (50) |
9 (75) |
6 (75) |
0.427 |
|
CVA, n (%) |
20 (3.2) |
9 (4.4) |
8 (2.6) |
3 (2.4) |
0.551 |
|
Re-AMI, n (%) |
4 (0.7) |
1 (0.5) |
2 (0.7) |
1 (0.8) |
1.000 |
|
Stent thrombosis, n (%) |
9 (1.5) |
5 (2.9) |
1 (0.3) |
3 (2.4) |
0.054 |
|
Repeat revascularization, n (%) |
6 (1.0) |
4 (2.0) |
2 (0.7) |
0 (0) |
0.259 |
|
CV death + CVA + Re-AMI + Stent thrombosis + repeat revascularization, n (%) |
54 (8.5) |
21 (10.2) |
20 (6.6) |
13 (10.3) |
0.249 |
|
Inotropic drugs, n (%) |
53 (8.5) |
17 (8.4) |
27 (9.0) |
9 (7.2) |
0.836 |
|
PM upon admission, n (%) |
12 (1.9) |
4 (2.0) |
8 (2.7) |
0 (0) |
0.188 |
|
IABC, n (%) |
11 (1.7) |
7 (3.4) |
4 (1.3) |
0 (0) |
0.048 |
|
OTI, n (%) |
41 (6.5) |
15 (7.3) |
21 (7.0) |
5 (4.0) |
0.444 |
|
NIMV, n (%) |
18 (2.9) |
6 (2.9) |
7 (2.3) |
5 (4.0) |
0.604 |
|
RRT, n (%) |
10 (1.6) |
6 (3) |
3 (1.0) |
1 (0.8) |
0.192 |
|
AVB, n (%) |
20 (3.2) |
7 (3.4) |
12 (4.0) |
1 (0.8) |
0.227 |
|
SMVT, n (%) |
18 (2.9) |
6 (2.9) |
9 (3.0) |
3 (2.4) |
1.000 |
|
VF, n (%) |
29 (4.6) |
12 (5.9) |
12 (4.0) |
5 (4.0) |
0.582 |
|
AF upon admission, n (%) |
42 (6.7) |
11 (5.4) |
23 (7.6) |
8 (6.4) |
0.597 |
|
Cardiac rupture, n (%) |
5 (0.8) |
2 (1.0) |
3 (1.0) |
0 (0) |
0.715 |
|
IVC, n (%) |
4 (0.6) |
1 (0.5) |
3 (1.0) |
0 (0) |
0.679 |
|
Acute MI, n (%) |
2 (0.3) |
0 (0) |
1 (0.4) |
1 (0.8) |
0.462 |
|
Bleeding BARC > 3, n (%) |
16 (2.5) |
2 (1.0) |
9 (3.0) |
5 (4.0) |
0.161 |
|
Infection, n (%) |
57 (9.0) |
12 (6.0) |
28 (10.1) |
17 (11.0) |
0.184 |
|
ARDS, n (%) |
12 (1.9) |
1 (0.5) |
7 (2.5) |
4 (2.6) |
0.208 |
|
Mechanical complication (MI, IVC or rupture), n (%) |
10 (1.6) |
3 (1.5) |
6 (2.0) |
1 (0.8) |
0.774 |
|
Killip class III or IV, n (%) |
62 (9.8) |
20 (9.8) |
31 (10.3) |
11 (8.8) |
0.898 |
Table 2: Clinical events according to the period of admission due to ACS
ACS: acute coronary syndrome. CVA: cerebrovascular accident (stroke). Re-AMI: acute myocardial reinfarction. CV: cardiovascular. PM: pacemaker. IABC: intraaortic balloon counterpulsation. OTI: orotracheal intubation. NIMV: noninvasive mechanical ventilation. RRT: renal replacement therapy. AVB: atrioventricular block. SMVT: sustained monomorphic ventricular tachycardia. VF: ventricular fibrillation. AF: atrial fibrillation. IVC: interventricular communication. MI: mitral valve insufficiency. BARC: Bleeding Academic Research Consortium. ARDS: acute respiratory distress syndrome.
During follow-up, we observed no significant differences in the combined endpoint of cardiovascular mortality, stroke, readmission due to new ACS, stent thrombosis and repeat revascularization (p = 0.249). On the other hand, the mean LVEF at discharge was similar in all three groups (p = 0.421), evidencing lower values in the patients admitted due to STEACS (Table 3). With regard to the patient delay times, significant differences were recorded among the different groups, with an increase in time from symptoms onset to FMC in the lockdown period (group B) and post-lockdown period (group C) versus the previous period (group A) (group A: 65 minutes (38-112) vs group B: 120 minutes (60-300) vs group C: 120 minutes (60-360); p < 0.001). These differences were the consequence of an increase in time seen in group B versus group A (p < 0.001) and in group C versus group A (p = 0.0004); no differences in this variable were recorded between group B and group C (p = 0.7102). Lastly, we also recorded significant differences in the time from electrocardiographic diagnosis to reperfusion among the three periods (p = 0.025), at the expense of a shorter time in group C. However, these differences were no longer significant after excluding STEACS with an evolution of over 24 hours from symptoms onset to FMC (p = 0.0789).
|
Variable (mean ± SD) |
Total |
Group A |
Group B |
Group C |
p |
|
LVEF at discharge (all ACS) |
49.2 ± 11.1 |
49.7 ± 11.6 |
48.6 ± 11.2 |
49.9 ± 10.0 |
0.421 |
|
LVEF UA |
55.9 ± 7.6 |
56.4 ±7.5 |
57.3 ± 6.0 |
53.0 ± 9.4 |
0.168 |
|
LVEF NSTEMI |
51.2 ± 10.7 |
51.2 ± 11.8 |
51.0 ± 10.8 |
51.6 ± 9.0 |
0.955 |
|
LVEF STEACS |
46.7 ± 11.2 |
46.4 ± 11.5 |
46.4 ± 11.2 |
47.8 ± 10.6 |
0.683 |
Table 3: LVEF according to the period of admission.
LVEF: left ventricular ejection fraction. ACS: acute coronary syndrome. UA: unstable angina. NSTEMI: non-ST-segment elevation myocardial infarction. STEACS: ST-segment elevation acute coronary syndrome.
|
Variable |
Total |
Group A |
Group B |
Group C |
p |
|
Total STEACS cohort |
|||||
|
Symptoms-FMC (n = 331) |
120 (60-240) |
65 (38-120) |
120 (60-300) |
120 (60-360) |
< 0.001 |
|
Diagnosis-reperfusion |
90 (60-146) |
100 (60-180) |
93 (60-163) |
60 (60-120) |
0.025 |
|
STEACS excluding patients with evolved AMI |
|||||
|
Symptoms-FMC |
120 (60-240) |
60 (36-120) |
120 (60-240) |
120 (60-330) |
< 0.001 |
|
Diagnosis-reperfusion |
90 (60-120) |
99 (60-150) |
93 (60-120) |
60 (60-120) |
0.0789 |
Table 4: Time intervals from symptoms onset to first medical contact, and from electrocardiographic diagnosis to reperfusion (guide advancement), in minutes.
STEACS: ST-segment elevation acute coronary syndrome. FMC: first medical contact. AMI: acute myocardial infarction.
Discussion
This multicenter study evaluated the impact of the COVID-19 pandemic upon the incidence, morbidity-mortality and management of ACS according to the hospital admission period, including a comparator group of patients that were admitted one month after the end of strict lockdown. The main findings were a decrease in the number of admissions due to ACS during the first months of lockdown, and an increase in the time from symptoms onset to FMC in patients with STEACS; this was not associated to an increase in mechanical complications or mortality, however.
Decrease in the incidence of ACS
Previous studies have reported a decrease in hemodynamic laboratory care activity as a consequence of the disease in admissions due to ACS during the pandemic, particularly in the context of STEACS [9–11]. Our findings confirm these data, with a marked 41% decrease in the first 30 days with respect to the previous month. This decrease persisted over the rest of strict lockdown and the post-lockdown period; however, as the isolation measures were eased and the incidence of infections decreased, a gradual rise in admissions due to ACS was observed. One of the factors that may have contributed to this situation is the intense care burden that characterized the first months of lockdown, with the consequent underdiagnosis and decrease in admissions due to ACS [12].
On the other hand, a notorious observation is the inverse relationship between the decrease in number of infarctions assisted in hospital centers and the increase in out-hospital sudden death worldwide [13]. A study in New York city recorded a three-fold increase in the cases of cardiac arrest (CA) and sudden death assisted by paramedical teams versus the same period in 2019 - these patients generally being older and with a greater presence of comorbidities [14]. Similar data were obtained by a French study showing the incidence of CA to double during the pandemic with respect to previous years [15]. Likewise, a study conducted in Italy documented this same increase coinciding with the rise in COVID-19 cases [16]. Seemingly less plausible is the idea that there may have been a genuine decrease in the incidence of the disorder attributable to physical rest among the population, with a more relaxed routine, improved diet control and a drop in environmental pollution [17,18]. Of note is the fact that the patients admitted during lockdown were younger, with fewer comorbidities and with a lesser cardiological history. This coincides with the observations of other authors [19,20]. These data suggest that older patients, with more disease antecedents and associated comorbidities, may have delayed or even indefinitely postponed contact with the healthcare system out of fear of becoming infected [21,22].
Symptoms-FMC-revascularization times in STEMI and adverse events
The times from symptoms onset to FMC increased significantly during lockdown, coinciding with the maximum peak in the incidence of infections. This observation is consistent with the data found in the literature [23]. However, no such delay was observed in the time from diagnosis to reperfusion (guide advancement). Fortunately, the mentioned delay did not result in an increase in mechanical complications or mortality in hospital or over follow-up.
Oriol et al. reported a delay in time from symptoms onset to FMC (105 minutes versus 71 minutes in the comparator group from 2019), with similar times from diagnosis to reperfusion [24]. This delay was associated to increased in-hospital mortality during the pandemic (7.5% vs 5.1%; unadjusted OR 1.5 (1.07-2.11); p < 0.001) - in contrast to our own observations. The absence of a direct relationship between delayed diagnosis and adverse events is difficult to interpret, though a plausible explanation may be the increase in out-hospital sudden death resulting from mechanical complications or malignant arrhythmias and the selection bias that occurs - since this study only included those patients with hospital admission.
Management strategies: percutaneous coronary intervention and surgical revascularization
No differences were seen in terms of the percutaneous invasive management of the patients with ACS before, during or after lockdown. The diagnostic coronary angiography and primary angioplasty rates, as well as the fibrinolysis, conservative management and complete revascularization data were homogeneous among the three groups in our study. These findings are in agreement with those of most of the studies analyzing the approach to ACS during the pandemic [12,24].
However, mention must be made of the marked decrease in myocardial surgical revascularization despite the presence of a significant number of patients with left coronary trunk and/or triple-vessel disease. Of these patients, 17.7% were subjected to surgical revascularization in the month prior to lockdown, only 5.5% during lockdown, and 34.5% in the month afterwards. Some registries describe a decrease in coronary surgeries [25], though others do not observe this tendency [19,25]. Such a marked decrease in surgeries during lockdown may be explained by the generalized tendency to postpone all operations as far as possible during those months, as evidenced by other studies [26]. Despite the complex coronary anatomy in patients with coronary trunk or triple-vessel disease, the treating physicians may have opted for percutaneous management of the culprit vessel, with the idea of completing revascularization at a later time through deferred surgery, or the provision of conservative management at least on a temporary basis. This is consistent with the fact that during the month after the end of lockdown, the number of revascularization surgeries increased to levels exceeding those before the official declaration of lockdown. In this context, it may be assumed that the operations that had been postponed during lockdown were carried out at this later time.
Limitations
Our study has the limitations inherent to retrospective, multicenter observational data analysis. In addition, the short duration of follow-up may have precluded the identification of potential consequences or differential events among the study groups. The lack of information referred to ACS occurring during the pandemic in patients that never reached tertiary care centers also complicates the drawing of conclusions.
Conclusions
A decrease in the number of admissions due to ACS was recorded during lockdown, with an increase in the time from symptoms onset to FMC in patients with STEACS. This was not associated to an increase in mortality of all causes during this period, however.
Abbreviations:
ACS: Acute coronary syndrome
STEACS: ST-segment elevation acute coronary syndrome
NSTEACS: Non-ST-segment elevation acute coronary syndrome
NSTEMI: Non-ST-segment elevation myocardial infarction
UA: Unstable angina
FMC: First medical contact
Acknowledgements: The authors thank the collaborators of each center participating in the study for their contribution to data collection and review of the present manuscript.