Clinical Research and Clinical Case Reports
OPEN ACCESS | Volume 6 - Issue 2 - 2025
ISSN No: 2836-2667 | Journal DOI: 10.61148/2836-2667/CRCCR
Kebede Tefera Betru1 *, Thuledi Makua2
1Hawassa University, College of Medicine and Health Sciences, School of Public Health, Hawassa.
2University of South Africa, College of Human Sciences.
*Corresponding author: Kebede Tefera Betru, 1Hawassa University, College of Medicine and Health Sciences, School of Public Health, Hawassa.
Received: July19, 2025 |Accepted: July 05, 2025 |Published: August 04, 2025
Citation: Kebede T Betru, Makua T, (2025). “Improving Early Detection of Leprosy Cases in the Communities of Sidama Region, Southern Ethiopia: A Qualitative Exploration of Health Professionals' Perspectives and Experiences”. Clinical Research and Clinical Case Reports, 6(1); DOI: 10.61148/2836-2667/CRCCR/091
Copyright: © 2025 Kebede Tefera Betru. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Leprosy is a chronic infectious disease caused by Mycobacterium leprae, one of the world's most neglected tropical diseases, and a leading cause of permanent physical disability. We aimed to explore the enhancement of early detection of leprosy cases in Sidama Region, Southern Ethiopia.
Method: This Study employed a qualitative, descriptive, and phenomenological exploratory approach. Non-probability purposive sampling was used to select participants, including doctors, public health officers, clinical nurses, health center administrators, technical and program experts from regional and district health offices, and health extension workers. In-depth interviews were conducted to gather experiential insights. The qualitative data were analysed using inductive thematic analysis with Open Code software version 4.0. The analysis involved data transcription, coding, theme development, and interpretation of the findings.
Result: The Study's findings indicated that the community's leprosy prevention and control programs remain problematic. Health professionals shared their experiences and perceptions on enhancing early detection of leprosy cases, focusing on several key issues: addressing prevalent misconceptions about Leprosy, encouraging timely healthcare-seeking behaviour, mitigating social stigma associated with the disease, and improving current practices for early detection of leprosy cases.
Conclusion: The study findings highlight persistent challenges in community leprosy prevention and control programs. Health professionals provided insights into strategies to enhance early detection of leprosy cases, emphasizing the importance of addressing misconceptions about the disease, promoting prompt healthcare-seeking behaviour, combating social stigma, and refining existing practices for early case detection. It strengthens the leprosy control program.
WHO classifies Leprosy as one of the twenty neglected tropical diseases (NTDs) (1). Leprosy is a communicable disease caused by the bacterium Mycobacterium leprae; the incubation period is long (average of 5 or more years), and untreated Leprosy can lead to impairment, disabilities, and exclusion. This infection can be cured through multidrug therapy (MDT). The drug regimen is dependent upon the classification of the case: paucibacillary cases receive six months of treatment with two-drug MDT. Multibacillary cases are highly specialized and treated for 12 months with a three-drug MDT. Multibacillary cases are identified as those with more than five skin lesions; paucibacillary cases have five skin lesions or fewer (2). Early diagnosis and use of MDT are the principal tools used to combat Leprosy. Despite a large reduction in prevalence over the last half century, Leprosy remains a public health issue in many countries (3). Delayed diagnosis and treatment can lead to nerve damage, presenting loss of muscle function or paralysis, even permanent disability (4). It is important, therefore, that patients are detected early for appropriate treatment. Several studies conducted in different likkamelaku
Ideally, prevention of disabilities should start with maintaining grade-0 (no disability) status by early recognition and treatment of leprosy reactions and neuritis. Nerve function impairment (grade-1) often manifests in the eyes, hands, and feet, which are most used in daily activities and are prone to injuries and ulcer formations. These, if neglected, lead to infection, tissue loss, and disfiguration. Persons at risk and their family members need to be informed about the signs of nerve involvement, trained in self-care and lifestyle modifications to prevent injuries and protect limbs and eyes, and encouraged to report to health facilities if required (5).
In 2014, 3,758 new cases with 482 children and 384 patients having G2Ds were recorded and the Incidences of new cases or more than ten years, LeprosyLeprosy in Ethiopia has been consistent year after year (AHRI 2017:20). In 2015, 3,970 new cases of LeprosyLeprosy in total were reported in Ethiopia (with 85% MB). Children and women comprised 14.2% and 31% of new leprosy patients, respectively. Over the same reporting period, 10.6% of newly diagnosed leprosy patients had Grade II impairment. The research claims that child health issues are still prevalent in Ethiopia. The number of newly reported instances is significant since it shows whether an infection is present in the neighbourhood. Regarding treatment completion, MB had an 86% rate while PB had a 71% rate (6).
If more accurate diagnostic methods are employed, the real rate of Leprosy may be greater than the existing average (0.7 per 10,000 persons), except for the prevalence of Leprosy, which is currently being treated. Additionally, research from Bangladesh, Indonesia, home-based studies, and India demonstrates that the prevalence of Leprosy is 2.5 to 9 times higher than that reported (7).
The distribution, as shown in the Ethiopia study, which is 59.6%, indicates a delay in diagnosis compared to the national aim of less than 1% for G2D by 2020, and the substantial load of Leprosy among patients after treatment is finished demonstrates that there is still a lack of care. Many individuals experience a variety of neurological and vision issues, including vision loss and neuropathic ulcers (8).
Through indirect means, G2D also disseminates information on additional elements that affect case detection, such as community leprosy knowledge, the ability of medical personnel to identify early signs and symptoms, and the overall quality of the leprosy prevention and control program (9). The WHO's plan for addressing the issue prioritizes measures to detect instances before noticeable deformity appears to reduce detection delays for cases(10).
The Study aimed to explore the bottlenecks in the early detection of leprosy cases in Bursa Woreda, Sidama region, and southern Ethiopia. This will support appropriate public health intervention strategies, planning, and implementation.
Methods
This Study employed a descriptive qualitative design utilizing a phenomenological approach, focusing on the subjective experiences, perceptions, and interpretations of healthcare phenomena among individuals. The Study is conducted in the Bursa District, Sidama Region, South Ethiopia, approximately 214 kilometers from Addis Ababa, the capital city. Bursa shares borders with Hula to the south, Aleta Wendo to the west, Wensho to the northwest, Arbegona to the northeast, and Bona Zuria to the southeast. Based on the 2007 Census data from the CSA, the district's population totals 103,631, with 51,731 men and 51,900 women; 2,304 individuals, or 2.22% of the population, reside in urban areas. The predominant religious affiliation is Protestantism, with 88.63% of the population adhering to this belief, while 6.25% follow traditional religions, 2.18% are Catholic, and 1.77% are Muslim (11). The primary language spoken in the area is Sidamigna. As of 2020, 22 public health facilities exist within the Bursa Woreda, encompassing 3 health centers and 19 health posts. According to the Woreda health bureau's statistics report, communicable diseases, including Leprosy, stand out as the primary health concerns within the study area. Consequently, the researcher investigated all health facilities offering leprosy diagnosis and treatment.
Study participants and sampling techniques
The Study's population comprised healthcare personnel, including CEOs of health centers, district health office TB/leprosy specialists, regional health bureau TB/Leprosy experts, health center OPD staff, health center TB/leprosy focal personnel, and community health extension workers (HEWs) engaged in leprosy prevention and control programs within the designated area. Initially, the researcher acquired staff rosters from the regional health bureau and purposefully selected individuals deemed sufficiently knowledgeable and experienced in leprosy management and program implementation. These selections were based on predefined criteria established by the researchers (12). A total of 23 participants were selected, consisting of 18 health workers and 5 health extension workers directly involved in leprosy prevention and control programs. Participation was voluntary, and participants were informed of their rights to join or withdraw from the Study at any point. In qualitative research, sample size is determined by the depth of information required, with the number of participants known as the sample size. The determination of participant quantity is guided by the information needs of the research and the principle of data saturation, as advocated by Creswell, Poth, Polit, and Beck (13,14).
In qualitative research, saturation delineates the juncture at which the sample size attains adequacy to encapsulate all pertinent themes, insights, and data pertinent to the Study's focal point. This denotes a state where further data collection becomes superfluous, as the amassed information consistently fails to unveil novel perspectives or enrich the comprehension of the research subject. In essence, saturation signifies a thorough understanding of the subject matter through the existing dataset [15]. Sampling ceases when no fresh insights emerge. Participants were solicited for in-depth interviews at locations and times convenient to them.
Method of data collection and analysis
Data collection
Data were collected through individual, face-to-face, in-depth, unstructured interviews. These open-ended interviews commenced with broad inquiries regarding the Study's subject matter, with subsequent questions influenced by participants' responses (16). Probing and follow-up questions were utilized to enhance the depth of investigation, continuing until information saturation was attained. Sessions, lasting 45-60 minutes, were audio-recorded and accompanied by note-taking. To ensure Confidentiality, interviews were conducted in private spaces within participants' workplaces, with each participant's response meticulously documented. Before the main Study, a pilot investigation was conducted at the health center office, involving the selection of medical professionals, including physicians, nurses, health officers, and health extension workers (HEWs). Interviewers, selected from among health professionals with expertise in neglected tropical diseases, demonstrated proficiency in interview techniques and possessed extensive knowledge of the local context, supplemented by rigorous training. Verbatim transcriptions of the interviews were produced from tape recordings, with participants' consent obtained. The use of audiotapes facilitated ongoing data review for validation during subsequent analysis.
Data analysis
The research employed an inductive thematic analysis for data examination, an approach particularly apt for exploratory studies delving into phenomena with limited existing knowledge. Simultaneous data collection and analysis preceded subsequent data gathering. Initial emergent ideas were discerned through audio recordings and field notes, ensuring data saturation. Ongoing data comparison identified saturation points. Verbatim transcription, initially in Amharic and later translated to English, supported interviews and researcher comprehension, meticulously checked for accuracy and coherence. Repeated readings familiarized researchers with the data. Line-by-line coding using OpenCode 4.0 Umeå software began with the richest data, ensuring inter-coder consistency. The principal investigator developed A comprehensive codebook manual, which was iteratively refined, maintaining code consistency through continuous review and recoding. Codes were then clustered into categories, forming the basis for theme development, which was facilitated by interrelated categories. The report was structured around major themes, categories, and participant quotations.
Ethics statement
Before the interview, ethical approval was obtained from the University of South Africa and Hawassa University Ethical Review Committee (Reference number: HSHDC/911/ 2019, IRB/275/12), and permission was obtained from the District Health Office. The purpose of the Study was clearly described for each study participant. Verbal consent was taken from each participant. Because verbal consent offers flexibility, allowing for adaptations or clarifications in the consent process as required, the Confidentiality of study participants was maintained by using code instead of identifying them by their name. All the information was coded for anonymity, and only the investigators can access the data. The participants were involved voluntarily and were informed of their rights to participate or withdraw from the Study at any time.
Results
Socio-demographic characteristics of study participants
All relevant levels of the health system – including the community level, the facility level, the district health office, the regional health bureau, and others – provided participants for this Study. Everybody was qualified, barring the community-level health professional, and all had degrees or higher. Most participants have worked on initiatives connected to Leprosy for over five years. Most participants at the time of the interview either oversaw a leprosy-related office or directed initiatives to combat Leprosy and tuberculosis. Table 1 presents the socio-demographic characteristics of study participants.
Table 1: Socio-demographic characteristics of participants in the Study of health professionals involved in leprosy control activities in Sidama Regional State, Ethiopia,2019
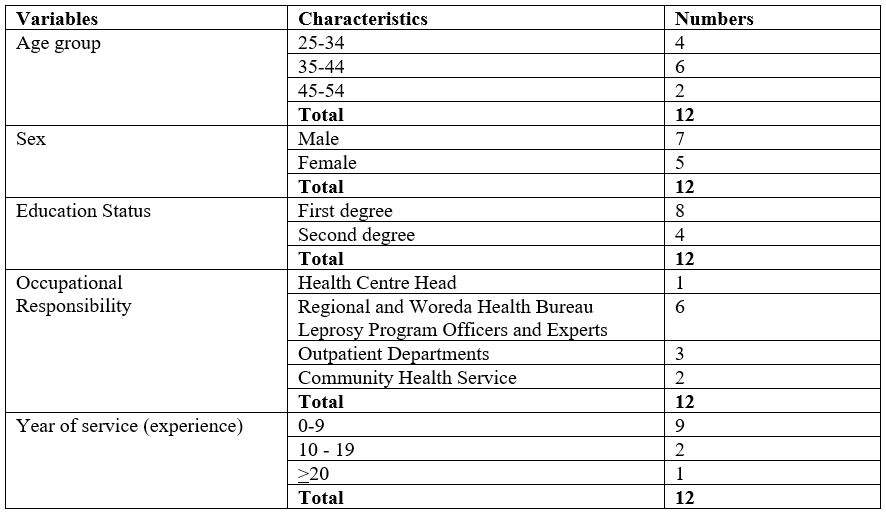
Interviews were conducted with twelve key informant health workers and health extension workers in the study area. The findings from these in-depth and key informant interviews were combined and organized around the following major themes.
The participants all understood that the bacteria Lepraemuris cause Leprosy, a disease that affects the body's nervous system, skin, eyes, and muscles. As a result, the patient can become disfigured. The participants asserted that the tardy diagnosis of the disease is one of the major factors contributing to the development of deformity (G2Ds).
All participants recognised that the problem of Leprosy is getting worse as time passes. The participants see Leprosy as a disease that will always be a public health issue. Participants reported disturbing trends in adult and paediatric leprosy diagnoses, as well as an increase in G II handicap cases. It was made worse by socio-demographic factors and beliefs.
Participants reported that the community believes Leprosy to be a curse for wrongdoings that are passed from parents to their offspring and as a punishment from God for sins committed. In light of that, the community usually prefers going to spiritual places and trying other traditional means
… the community sees Leprosy as a punishment from God for their sins or bad deeds, at that moment they committed to seeking spiritual solutions. This causes irreversible damage to the body because most of the time patients come to health facilities after severe and irreversible damage has happened to their body. [P11]
Since the community considers it a punishment from God, they might go to spiritual places and use holy water … as I said before, those who think that it is God's punishment stay at home and use ineffective interventions. Therefore, the main thing is what the sick person believes about Leprosy. Leprosy and also the community stigma attached to those affected can be huge. [P1]
Another sub-theme emerged is the belief that Leprosy is a hereditary disease passed on from generation to generation. A district officer reported the following:
There are still people who see Leprosy as a hereditary disease … one does not tell the other because of fear of possible consequences to the next generation, like no one will marry from that family, assuming the whole generation is infected … We educate the community that Leprosy is not a hereditary disease. However, some will not accept that. Those people discriminate against leprosy patients at all social events. [P5]
Although many shared that the community has a low awareness of the early symptoms of Leprosy, other participants explained that the community recognises the later symptoms and calls them by their local name. Also, when there is a history of Leprosy within the family or if the disease starts to cause disability, people recognise it. A community-level health worker explained:
When changes start to show in the nails and skin, the community calls it ‘anatamoo' [literal meaning is wound] … So the community identifies Leprosy when people can no longer carry out their daily activities. [P9]
All participants agreed that many are unaware that the disease has a cure for free.
…. by the way, many are not even aware that there are drugs to take and get healed without paying a penny. We had chatted with clients who were recently diagnosed and told us that they did not know it was curable for free. [P8]
The other awareness-related issues explored relate to the transmission of Leprosy. Participants reported that people believe that leprosy transmission is lifelong, whether it is treated or not. One key participant shared real experience, saying.
I always talk about an event that surprised me. As a professional, I know that a cured leprosy patient does not transmit the disease. There was a leprosy patient who took complete treatment and was cured of it. Years later, he died from another illness. The community declined to arrange a funeral ceremony for him. His family had a very harsh and agonising time … at the end, we arranged and buried him … Unless a person breathes, the disease cannot pass from one to another. A dead body cannot breathe! It is wrong to worry and panic about acquiring the disease from a dead body. Indeed, it is an irrational and wrong belief. It shows how unaware our communities are … I commonly share this experience at various sessions. [P1]
Participants were asked about Leprosy awareness among the community and health providers. All participants explained a lack of awareness in the general community and among most healthcare providers, including tertiary-level professionals. G2D is indicative of a delay in the detection of Leprosy.
Interviewed participants reported that early health-seeking practices are low and that this hampers timely intervention and the prevention of leprosy-related complications. Participants agreed that clients come to the health facility when G2Ds are evident. Key participants stated that delaying seeking early care was caused by ignorance of the early symptoms of Leprosy and the availability of free treatment. Furthermore, ignorance, the absence of pain, and being unconcerned are other contributors to the delay in seeking care.
The community feels that they have a disease when the disease progresses to an advanced stage. They come here when they have a wound. They do not come at an early stage. Although patients come for healthcare, they do not expect Leprosy. They said that they had a skin spot that was red, tender, and swollen. They did not come to the health facility early. They have a low level of leprosy-related healthcare-seeking behaviour. [P8]
Another participant concurred with this idea, saying.
As the manifestations are not severe early, the patients have delayed healthcare-seeking behaviour. The patients stay at home for a prolonged time in the early phase. Early, it is not painful. Our communities go to health facilities when the disease advances, affecting their daily lives. Mostly, that might lead to late diagnosis and Grade II disabilities … G II are caused by delayed health-seeking behaviour. [P4]
Another participant said:
… delay to seek care before the diagnosis was made, many patients moved from one healthcare service to another when they did not get better after treatment due to misdiagnoses made. [P6]
A key participant stated:
The main problem is related to the communities' lack of knowledge on the symptoms of Leprosy, its complications, the benefits of early seeking, and the consequences of delayed seeking. Secondly, the community should know that the disease is treatable. As I said before, those who think that it is God's punishment stay at home and use ineffective interventions. Therefore, the main thing is knowledge. [P8]
The participants noted a lack of clinical knowledge on Leprosy among healthcare providers. In most cases, healthcare providers attend outpatient departments with little or no knowledge of leprosy cases in general. Concerning the early detection of Leprosy, most participants mentioned that they had misdiagnosed and mistreated cases. Consequently, such a knowledge and skill gap created an inability to detect the early signs and symptoms of leprosy cases. These conditions can delay treatment initiation, increasing the risk of disability (deformity) and prolonging the risk of infection transmission in the population.
Some of the participants also said that they received integrated TB/leprosy training that lasted for a few days (three to five days). During this training, TB took up almost all of the time. Leprosy training was given as an afterthought during part of a day or on half of the final day of the training, without considering practical experiential learning.
Disabilities, complications, and the continuation of disease transmission are all issues that are impacted by delays in the care and service delivery in medical facilities.
High-level graduates, like the health officers and those with BSc degrees, did not know the manifestations, so they were treated with fungal medications in the early times. How do we expect the community to be aware when they [health professionals] do not know about Leprosy? [P4]
A participant from the Bursa TB/leprosy unit expressed his discomfort with the way of training.
Most of the time, health professionals who are assigned to work in OPD and TB/leprosy clinic get only one day of training on LeprosyLeprosy, so we do not know well what we are going to work with in leprosy cases, even though the training was without practical experiential learning. [P8]
A South Regional Health Bureau participant explained that preventing nerve damage and impairment by early detection and quick MDT treatment of all new cases of Leprosy remains the primary method for controlling the disease. Additionally, an early diagnosis offers the chance to slow or stop further transmission.
About 95% of leprosy cases can be detected with observable signs and symptoms. However, specialists working in tertiary facilities refer suspected cases to national dermatology centers. You can imagine how knowledgeable lower-level health professionals could be. [P4]
Another participant from the Woreda Health Office said:
Patients who are seen at a health facility who are suspected to have Leprosy are not properly assessed or promptly referred. [P10]
Other participants relate to the lack of awareness and skills of healthcare providers, saying
Last year, we requested health professionals to perform physical examinations of the family members of leprosy patients who have been on follow-up for the last four to five years. They did not do it properly. The case detection problem is mainly related to the lack of awareness about leprosy symptoms and diagnosis. Secondly, health professionals do not have equal knowledge. While doing physical examinations of clients, health professionals may not consider a lesion an indicator of Leprosy. Leprosy, because they focus on inspection, they will only do inspection and ignore further investigation of any lesions they see. So, the case detection activity is poor because of awareness-related problems, and health professionals focus on the momentary impression
and inspection, not the long-term approaches. [P2]
Another participant agreed with this viewpoint and stated that inadequate training and excessive levels of professional turnover, both in and out of facilities, contributed to the late discovery.
… as I have said before, they might misdiagnose the case because of a lack of continuous capacity-building activities … high-level graduates like the health officers and those with a BSc degree do not know the manifestations, so in the early times they were just treated with fungal medications. [P1]
Another participant explained that delay relates to looking to other options for treatment.
Delayed health-seeking behaviour relates to painless lesions or early manifestation. Patients might use other home remedies since the early manifestations are not severe. They also might go to spiritual places and use holy water. This might occur. [P2]
Social stigma and discrimination are closely associated with the leprosy disease. All the participants responded that LeprosyLeprosy is a disease highly associated with stigma and that stigma leads to delays in seeking care. Leprosy patients become isolated from almost all social occasions that are highly valued in the community. Leprosy stigma and discrimination are brought on by misunderstandings about the disease and spread to one's own family, friends, peers, and the community, as well as to other locations, including churches, schools, markets, workplaces, and social events such as weddings and funeral ceremonies.
One key participant said:
The community calls it 'a wound' if we interpret it directly. If a person is known as a leprosy client, then he does not attend funerals or go to mourn, will not be engaged in social issues, people do not go together, people do not eat or drink together, and his children do not play with other children. That is the worst thing that can happen to anyone, so they do not go to a health facility early or sometimes lately. Moreover, we all know what happens if they do not get treatment, such as an infected wound that smells bad, physical deformities on their hands, legs, mouths, eyes, noses and bones, as well as physical disabilities in their legs, hands and eyes, which cause them to withdraw from social interaction and be stigmatised if others find out. These are the major justifications for avoiding medical facilities. [P8]
Another participant stressed that self-isolation is a common problem that could delay seeking care.
Most patients conceal their symptoms or deny the diagnosis and delay in seeking treatment … Mostly people exchange idea in villages so if someone who knows the symptoms of LeprosyLeprosy and could tell others about what he saw therefore those is possible symptoms hide themselves even they hide the wounds in their extremities due to fear of social rejection. [P9]
A participant from the MoH related the delay in seeking care to a lack of accountability.
We have to create a system that could help us to make sure that everyone working in the health system to take responsibility and be accountable … for example, if a leprosy client comes with any form of wound or disability then we have to ask the community health worker and the district leprosy focal why this happens. So unless we create a way to make lower-level professionals responsible for what happens to the community, we cannot eliminate Leprosy as a public threat. [P3]
Other participants expressed a different view, saying that failure is the fault of higher administration.
… it is our gap. We do not encourage health extension workers to identify cases. We do not mobilise them. Therefore, patients who come for care at an advanced stage … so patients come when wounds have an odour and make them unable to do daily activities. [P8]
To minimise shame and to stop their families from becoming aware of their condition in their communities, nearly all leprosy patients are compelled to keep their illness a secret from their family members. Sometimes, communities avoid taking part in early case detection activities because they believe that health professionals are unreliable and that doing so will cause them to face social stigma. [P2]
The qualitative Study also revealed that the detection practice at community and facility levels ranges from very low to non-existent. They expressed that community-level practice is non-existent due to lacking trained professionals and less attention to leprosy prevention.
Participants reported that primary health facility-level detection is very simple because clients come at late stages with clear symptoms.
There are
manuals for health professionals at the health centre, but clients come late to G II, at which detection is very simple. However, no early detection practice is being done by lower-level health facility professionals … Let alone LeprosyLeprosy, TB screening has even been forgotten, which is expected to be done for every client attending OPD. The professionals [lower level] do not carefully look at it, which is why we are seeing clients go to the hospital, be diagnosed with TB and Leprosy, and come to the health centre for only follow-up treatment. [P6]
A leprosy focal person from a health facility explained that facilities and community-level detection are doing less than the leprosy-cured client associations formed by NGOs long ago. He reported his real experience, saying.
Last time, there was one case with nodules; the case was not diagnosed by the community health extension worker or health professionals here. An association member brought him here … I have provided the care and consulted the doctor. It was diagnosed as Lepromybose. He is making good progress … they counsel one another on various issues, including medication adherence. [P7]
Concerning community-level leprosy detection, participants said it was barely different from the facility practice. A participant said there is a lower detection rate in the community due to a lack of priority for Leprosy.
Although we encourage health extension workers [community health workers expected to detect Leprosy at the community level] to send cases to the health facility, now, the attention is low … due to that, we might miss cases. Since the health extension workers programme has not been strengthened, we cannot identify cases easily. I believe that there is a high number of cases in the community. However, the number of newly detected cases is low. It might relate to the low level of case detection. [P7]
Other key participants shared this idea and mentioned poor awareness as a reason for the low detection rate in the community.
The case detection is poor. Even in hot-spot areas, case detection is very poor. The community-based one-to-five structure and health development army does not enforce early arrival to the health facility while the patient has early manifestations like lesions. Poor awareness creation contributes to the case detection gap. [P2]
A former TB/leprosy focal person of the district expressed how the activity has been overlooked after a project phased out and how Leprosy boomed thereafter, saying.
Since the Challenge TB project phased out, there has been no meeting, discussion, review meeting, or community-level activity about Leprosy. It is supposed to be our duty to work on … People are going to hospitals for illnesses other than leprosy diagnosis. Leprosy has become the biggest threat here. [P5]
The general public still views Leprosy as a serious illness that should be avoided, and does not think it can be cured.
Discussion
This Study showed that most healthcare professionals have directly observed how society views people with Leprosy. Society believes that the wrath of gods and goddesses brings on Leprosy. An individual with a G2D fervently believes it is a 'punishment' (17). A study conducted in Ethiopia found that over half of those polled believed Leprosy was a genetic disorder, a curse from God, or a result of sin being punished (18). People continue to think that those who previously had Leprosy still do. Few participants believe that leprosy results from eating specific types of food or from malnutrition, is caused by natural forces, or is a punishment for misdeeds (19).
According to a study, there are still many myths about medicine from the late 19th century, including the notion that Leprosy is an incurable, extremely contagious, and touch-transmitted disease (20). According to a study done in Ethiopia, most respondents still think Leprosy is a hereditary disease (21; 18). Most participants from the Mbonge and Ekondotiti health districts stated that Leprosy is inherited or results from a union with a family where Leprosy is present or has been (22). Leprosy is thought to be inherited and incurable in Thailand because the community frequently witnessed multiple cases of the disease in a single family; therefore, villagers were forbidden from allowing their children to marry leprous persons (23).
Leprosy is perceived as an incurable and crippling disease. Study in India, perceived as LeprosyLeprosy an incurable and crippling disease and majority of them also believe that it is a type of retribution for bad activities or actions conducted at some point in the past or present. As old as the sickness is, it is the issue brought on by the idea that it is incurable that is most disconcerting (24).
Leprosy can be completely cured with MDT. Rifampicin, dapsone, and clofazimine are the three medications all leprosy patients must take as part of MDT for six months for PB leprosy and 12 months for MB leprosy. People with Leprosy are no longer contagious after just a few doses of MDT. However, to fully recover from their illness, they must take all the antibiotics as directed by medical professionals. Leprosy stops being contagious in 98% of cases after being identified and treated with MDT. To reduce transmission and avoid disability, early diagnosis and appropriate treatment are essential. The use of SDR as a preventive treatment for adult and child contacts of leprosy patients results in a 57% reduction in leprosy risk after two years and a 30% reduction after five to six years, after ruling out LeprosyLeprosy and tuberculosis (TB) disease and in the absence of other contraindications (25; 26).
Lack of early symptom awareness in the community was identified in the Study. Low rates of early health-seeking behaviours prevent quick intervention and the prevention of leprosy-related problems because awareness and communication about Leprosy are lacking. Participants concurred that patients should go to the G-II medical centre. The number of G2Ds at the time of diagnosis directly indicates the failure to make an early diagnosis and acts as a gauge for the low level of community IEC penetration. According to Danturty, Manchala, and Jairaj (27), the population surveyed does not understand the symptoms of Leprosy. Studies have demonstrated that a substantial number of patients have obvious malformations as a result of the delayed recognition of leprosy signs.
Healthcare-seeking behaviour was the main factor linked to delayed case discovery. The majority of surveyed patients were unaware that the symptoms they were experiencing were leprosy-related, and many of them thought the symptoms would go away on their own because they thought they were afflicted with something else (17; 28). Many patients are still unaware of leprosy symptoms. Nearly half of the participants in the Brazil study delayed visiting a doctor because they did not believe their symptoms were significant.
This Study showed that most health professionals lack clinical knowledge and practice in leprosy cases. In Ethiopia, leprosy control efforts are incorporated into general healthcare services; however, general healthcare professionals' understanding of leprosy diagnosis, management, and treatment was inadequate. The Study revealed that most healthcare professionals did not understand how to recognise Leprosy's early signs and symptoms and how to treat them. Most healthcare professionals were unable to assess patients' muscles and sensations voluntarily. It could be a factor in Ethiopia's comparatively high percentage of G2Ds (29).
The social stigma and discrimination associated with the leprosy disease are very strong. The most pressing issue is the prevalence of deformity because the social responses to people with leprosy-related deformities and their families are frequently tragic, callous, and uncaring, accompanied by offence, expulsion, and even the purposeful murder of victims. This can result in stigma, which is detrimental to the dignity and conduct of leprosy patients (30).
Leprosy patients get separated from nearly all social gatherings that are highly valued in society as a result of the stigma and delay in seeking help. Due to misinformation, leprosy patients are subjected to stigma and discrimination in a variety of settings – churches, schools, markets, and places of employment. They are also prohibited from sitting next to, shaking hands with, sharing or purchasing food from others, using public transportation, and attending social events such as weddings and funerals. Additionally, community members are unwilling to let their children play with the leprosy victims' children. Family members marrying leprosy patients draw criticism. The most frequent social and societal element linked to the delay in discovery was stigma (31; 32; 33).
The Study revealed that health facilities could not pay appropriate attention to the early detection of leprosy cases. According to the Study, the average time it took to diagnose Leprosy was 33.5 months. Remarkably, 70% of the patients claimed that their condition had been initially incorrectly identified and treated. Fungal skin conditions and skin allergies were the most frequently reported incorrect diagnoses. These errors failed to identify first misclassified patients, leading to a much longer diagnostic delay (34). Leprosy's polymorphic nature and the fact that most medical professionals are unaware of its clinical signs are two factors that contribute to misdiagnosis (35). Similar to earlier studies, in Brazil, it was discovered that patient reports of misdiagnosis were frequently associated with prolonged health system delays and diseases like rheumatism and skin allergies (36).
This Study identified that the lack of community-level detection of leprosy cases and contact tracing was one of the major problems. Leprosy contact tracing is the cornerstone of active surveillance and a crucial strategy for the early identification of new cases. It also aids in halting transmission by eliminating potential infection sources. The increase in the number of newly detected cases in several countries is attributed to operational factors rather than an actual increase in incidence because many cases that had been concealed for a long time were discovered as a result of active case detection campaigns (including contact examination) in many countries (37).
A longitudinal study in the Karonga district of Malawi found that people who live in HHCs of MB leprosy patients have a five- to eightfold increased risk of developing the disease compared to people who do not live in such dwellings; however, the risk of developing Leprosy in HHCs of PB leprosy patients is lower. HHCs had a higher risk of developing LeprosyLeprosy, according to a survey conducted in Sri Lanka's Puttalam region (odds ratio: 6.69; p-value 0.001). A study conducted in Bangladesh concluded that a contact examination should be completed as soon as an index case is found. Studies from the Comoros and Bangladesh indicated that contact screenings should be expanded to include neighbours since they revealed a higher risk of Leprosy among contacts outside of households (38)
Leprosy in children is a sign of active community transmission (39). Whether the infection is hereditary or not, close contact may be the source. A neighbourhood's childhood leprosy cases amply illustrate the severity of the undiagnosed adult leprosy problem, as well as its abnormalities, active transmission, and impacts on both the patient and the community. Among 5,760 contacts, 114 new cases were discovered through door-to-door surveys (2.0% prevalence). The two years prior had seen the discovery of 39 additional instances. Living within 25 metres of index cases statistically increased the likelihood of having Leprosy (40).
Limitation
Qualitative research often faces limitations due to small sample sizes, which hinder the generalization of findings to broader populations. Additionally, data saturation or repeating themes can restrict the novelty and originality of qualitative insights. Subjective interpretation during translation may introduce bias. This Study, constrained by budget limitations, included only health professionals working with leprosy programs, not the experiences of patients and the community. Future research should involve larger-scale studies with more diverse samples across multiple geographical locations to validate and expand upon these findings.
Conclusion
The findings underscore ongoing challenges in preventing and controlling Leprosy within the community. Health professionals shared valuable insights into strategies for enhancing early detection of leprosy cases. They highlighted several key areas for improvement:
These findings highlight the necessity for comprehensive, targeted interventions that address these specific areas to bolster leprosy control efforts and improve health outcomes in affected communities.
Acknowledgements
The authors express their gratitude to Hawassa University for funding this Study. We also sincerely thank the study participants for their voluntary involvement and the data collectors for their invaluable assistance.
Funding
Hawassa University provided funding for the research. However, the funding institution was not involved in the study design, data collection, analysis, publication decision, or manuscript preparation.
Competing interests
The authors have declared that no competing interests exist.
Data Availability Statement:
All relevant data are in the manuscript or
UNISA Institutional Repository:
Authors’ contributions
KTB and TM were involved in the Study's design, the drafting of the proposal, the oversight of data collection and analysis, and the preparation of the results and manuscript. All authors accepted responsibility for every aspect of the work and reviewed and approved the final manuscript.