Clinical Research and Clinical Case Reports
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2836-2667 | Journal DOI: 10.61148/2836-2667/CRCCR
Tammiraju Iragavarapu
Affiliation- Professor and HOD of cardiology, ASRAM Medical college, Eluru, Andhrapradesh-534005, India.
Corresponding authors: Tammiraju Iragavarapu, Affiliation- Professor and HOD of cardiology, ASRAM Medical college, Eluru, Andhrapradesh-534005, India.
Received Date: August 16, 2024
Accepted Date: September 23, 2024
Published Date: October 18, 2024
Citation: Tammiraju Iragavarapu, (2024). “Mediastinal Mystery:Malignant Cardiac Tamponade masquerading Mediastinal mass with bovine aortic arch. Insights from a Case Report”. Clinical Research and Clinical Case Reports, 5(2); DOI:10.61148/2836-2667/CRCCR/85.
Copyright: © 2024 Tammiraju Iragavarapu,This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Thymoma, a spindle cell tumor originating from the anterior mediastinum, is a rare neoplasm that seldom presents with cardiac tamponade, a life-threatening condition where fluid accumulation in pericardial sac impairs cardiac function. We report the case of a 23-year-old male who presented with classic symptoms of cardiac tamponade, which were later found to be secondary to an invasive spindle cell thymoma. The tumor's aggressive nature and advanced stage rendered surgical resection unfeasible. Initial management involved an emergent pericardiocentesis to relieve the cardiac compression and stabilize the patient. Following this, a multimodal therapy with chemotherapy and radiotherapy was implemented, aiming to control tumor progression and manage symptoms. This case underscores the importance of early intervention and the potential benefits of a coordinated, multidisciplinary approach in managing neoplastic cardiac tamponade.
Introduction:
Thymomas are rare tumors that originate from the thymic epithelial cells in the anterior mediastinum, accounting for about 20-30% of all mediastinal tumors. These tumors typically present with local symptoms due to compression of adjacent structures. Spindle cell thymomas, a histological subtype, are even less common and can present diagnostic challenges1. Cardiac tamponade, as an initial manifestation of thymoma, is exceedingly rare but necessitates immediate recognition and intervention due to its life-threatening nature. This case report highlights the clinical presentation, diagnostic workup, and management of a patient with cardiac tamponade caused by an anterior mediastinal spindle cell thymoma.
Case Presentation:
A 23-year-old male with no past medical history presented to the emergency department with complaints of dyspnea, chest pain, and fatigue. The patient reported a history of progressive shortness of breath and chest discomfort over the past few weeks, which had acutely worsened. Upon presentation, the patient was found to be hypotensive with a blood pressure of 90/70 mm Hg, tachycardic with a heart rate of 120 beats per minute, and exhibited signs of raised JVP (14 cm). The patient was afebrile and coherent. On systemic examination, cardiovascular findings included muffled heart sounds, while the respiratory examination revealed decreased breath sounds over the left side of the chest. ECG showed electrical alternans (Fig 1a). Chest X-ray demonstrated cardiomegaly with left-sided pleural effusion(fig 1b).
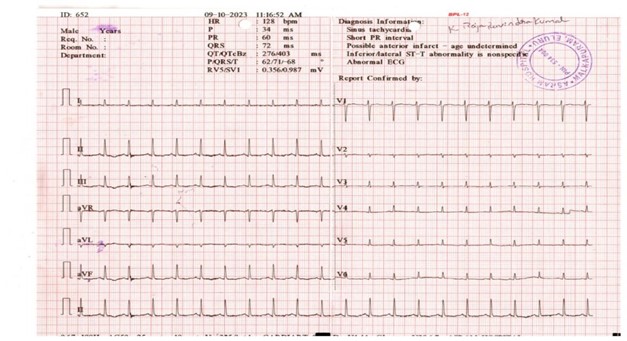
Figure 1A: ECG showing electrical alternans
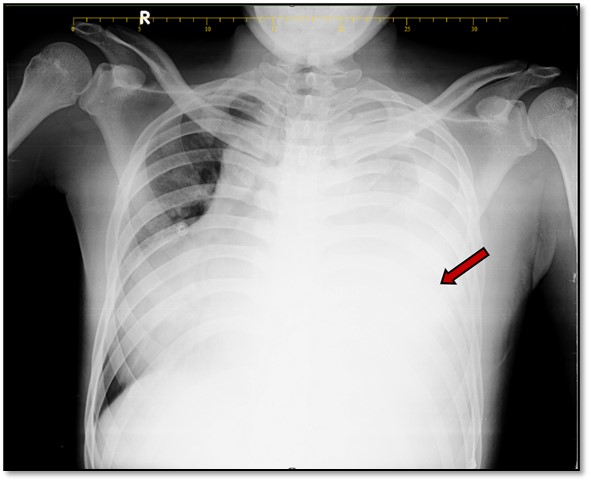
Figure 1b: shows a chest X-ray with a left-sided pleural and mediastinal shift to the right side.
Transthoracic Echocardiography showed dilated left ventricle with moderate LV dysfunction and large pericardial effusion with diastolic collapse of the right ventricular free wall suggestive of tamponade(fig 2).
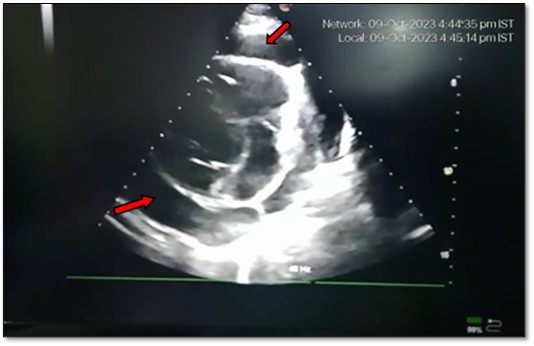
Figure 2: 2D echocardiogram showing pericardial effusion with tamponade.
CT Scan of the Chest showed a large ill-defined lobulated soft tissue density lesion measuring 17 x14x10cm (CCX TR X AP) noted arising from the anterior mediastinum seen extending into the left hemithorax. On post-contrast, there is heterogeneous enhancement with non-enhancing necrotic areas within. This mass lesion is causing tracheal, oesophageal, and mediastinal shift towards the right side, abutting the main pulmonary artery and encasing the left pulmonary artery and left pulmonary vein. It is also encasing the arch of the aorta and its branches, abutting the descending aorta, and encasing the left main bronchus(fig 3).
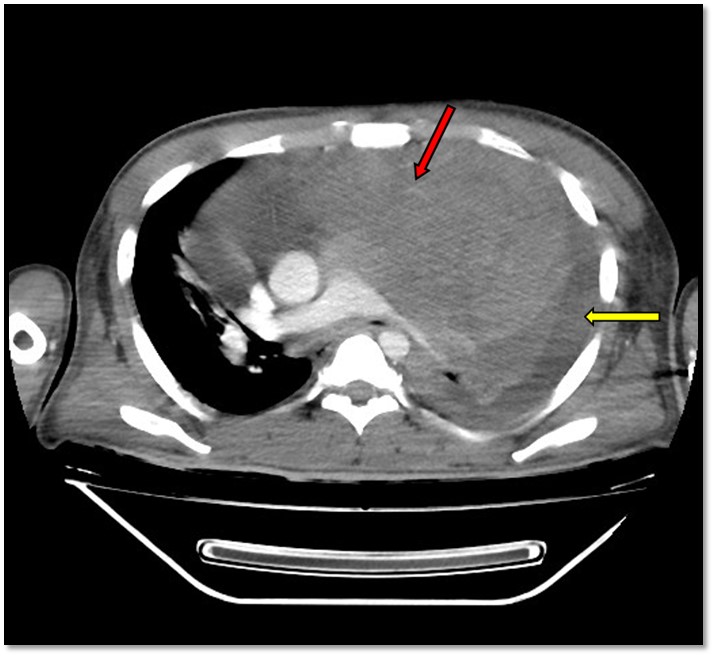
Figure 3: Contrast-enhanced computed tomography (CECT) showing a large anterior mediastinal mass (red arrow) and a left massive pleural effusion (yellow arrow).
In view of hemodynamic instability, emergency pericardiocentesis was performed, draining 1000 mL of pericardial fluid, resulting in immediate hemodynamic stabilization. CT guided biopsy of mass lesion was done and histopathological examination showed spindle cell thymoma. Surgical resection was not done due to the encasement of the great vessels and its branches. The patient was started on induction chemotherapy with the CAP regimen (cyclophosphamide, doxorubicin, and cisplatin), followed by radiotherapy for local disease control and palliation. The patient succumbed 6 months after treatment.
Discussion:
Etiopathogenesis:
The incidence of pericardial disease as the presentation of an unrecognized underlying malignancy is about less than 10%2. Another similar study reported that the likelihood of finding a neoplastic disease is more for large pericardial effusions when compared to small effusions. Autopsy studies reveal that malignant cardiac tamponade is responsible for approximately one third of cases. Thymomas are uncommon anterior mediastinal tumors, with an incidence of 0.15 cases per 100,000, originating from the thymic epithelium and constitute about one fourth of all mediastinal masses across all age groups. They can present with a wide range of clinical symptoms, from asymptomatic masses found incidentally to severe compressive symptoms1. While 70-80% of them are benign, 2-6% are malignant. Spindle cell thymomas, a rare histological subtype characterized by elongated spindle-shaped cells, can present diagnostic challenges due to their rarity and diverse manifestations3. Thymoma can cause pericardial effusion in several ways:1.Direct invasion: The tumor can invade the pericardium, leading to inflammation and fluid accumulation. 2.Metastasis: Thymoma cells can spread to the pericardium, causing effusion. 3.Autoimmune response.Thymoma can trigger an autoimmune response, leading to inflammation and fluid build-up in the pericardium. 4.Inflammation by Chemoradiation. Cytologic evaluation had a specificity of nearly 100% for diagnosing malignant pericardial Effs4,5.
Definitive diagnosis of thymoma is confirmed through histopathological analysis of tissue samples. In our case, according to Masaoka staging, the thymoma is classified as a stage III tumor. Histologically, the thymic epithelial tumor in our patient is identified as a World Health Organization (WHO) type A thymoma, characterized by lobulated neoplastic spindle cells with areas of tumor necrosis. The TNM stage for this case is stage III B.
Management-
The management of pericardial effusion is guided by the presence or risk of tamponade. As our patient presented with cardiac tamponade, an emergency pericardiocentesis was done. Pericardiocentesis is a catheter-based procedure designed to aspirate fluid from the pericardial space, indicated for cardiac tamponade, large pericardial effusions (typically >2 cm), symptomatic moderate effusions, and diagnostic purposes. Three main approaches can be used for pericardiocentesis: the apical, the subxiphoid, or the parasternal approach. An alternative to traditional surgical approaches is percutaneous balloon pericardiotomy (PBP), which creates a pericardial window using a balloon catheter and is especially effective for recurrent effusions, particularly in neoplastic cases6.
The treatment of choice for underlying tumor is surgical resection for localized tumors, offering the best chance for cure. However, in cases where the tumor is invasive and encases vital structures, as in our patient, surgical resection may not be feasible. In such scenarios, multimodal therapy, including chemotherapy and radiotherapy, is essential for disease control and palliation. The CAP regimen is commonly used for chemotherapy, targeting proliferative cells and reducing tumor burden. Radiotherapy complements chemotherapy by providing local control and alleviating symptoms caused by the tumor's compressive effects7.
Prognosis:
The prognosis of thymomas varies based on the tumor stage, histological subtype, and response to treatment. Although less common, Spindle cell thymomas can have a favorable prognosis if detected early and managed appropriately. Long-term outcomes are influenced by the tumor's invasiveness and the effectiveness of multimodal treatment strategies. The one-month mortality rate for patients with neoplastic cardiac tamponade is 33%, with an average survival of less than five to six months. This survival period further decreases to just 2-3 months if fluid cytology is positive for malignant cells8,9. In our case report, due to more invasive nature of the tumor, patient survived for only five months after undergoing pericardiocentesis and chemotherapy.
The salient features of Neoplastic pericardial effusion were mentioned in
Table 1: Showing Salient Features Of Neoplastic Pericardial Effusion
|
Etiology |
Primary Malignancies: Tumors originating in the pericardium (e.g., mesothelioma, sarcomas). Secondary Malignancies: Tumors that metastasize to the pericardium (e.g., breast cancer, lung cancer, leukemia, lymphoma). |
|
Mode of Spread |
Hematogenous Spread: Tumor cells spread through the bloodstream. Lymphatic Spread: Tumor cells spread through lymphatic channels to the pericardium. Direct Extension: Tumors from nearby structures invade the pericardium. Inflammation: chemoradiation Opportunistic infection |
|
Clinical Features |
Symptoms: Dyspnea (shortness of breath), chest pain, fatigue, cough. Signs: Pericardial friction rub, decreased heart sounds, hypotension (in severe cases). |
|
Diagnosis |
Becks triad is less commonly seen. chest X-ray showing enlarged cardiac silhouette Echocardiography CT/MRI |
|
Treatment |
Medical Management: Diuretics, , and corticosteroids to reduce inflammation. Pericardiocentesis: subxiphoid/apical Surgical Options: Pericardial window, percutaneous balloon pericardiotomy (PBP), and pericardiectomy in severe or persistent cases. |
|
Prognosis |
Prognosis is largely influenced by the type and stage of the underlying malignancy. 5-6 months on average. |
Conclusion:
This case underscores the diagnostic and therapeutic challenges associated with neoplastic cardiac tamponade, especially when it involves spindle cell thymomas presenting with cardiac tamponade. Early recognition and prompt intervention are critical for optimizing patient outcomes. Multimodal treatment strategies, including chemotherapy and radiotherapy, are vital in managing unresectable tumors and achieving disease control and symptom palliation.
Conflict of Interest: No conflicts of interest.
Funding: This study received no specific funding.
Ethical Approval: Ethical approval was obtained from the institutional review board of ASRAM Medical College.
Informed Consent: Informed consent was obtained from the patient.