Authors
Hesham Maged Mohamed
International Scholars, Neuropsychiatry Specialist.
Article Information
*Corresponding author: Hesham Maged Mohamed, International Scholars, Neuropsychiatry Specialist.
Received: July 20, 2025 |Accepted: July 30, 2025 |Published: August 07, 2025
Citation: Hesham Maged Mohamed., (2025) “Psychiatric Illness in Post-Traumatic Brain Injury Patients: A Review Article.” Clinical Psychology and Mental Health Care, 7(1); DOI: 10.61148/2994-0184/CPMHC/066.
Copyright: © 2025 Hesham Maged Mohamed. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Abstract
Traumatic brain injury (TBI) is called the silent epidemic as many of the symptoms are not readily detectable despite TBI being a worldwide public health issue. Epidemiological studies in the US shоw that annually up to 2 millions people experience a traumatic brain injury (TBI). Of these, almost 300,000 are hospitalised, and over 50,000 will die from their injuries.
[1] Trauma registries shоw that approximately 5.3 millions American are living with TBI-related disabilities.
[2] The 2010 Global Burden of Disease survey shоw that in most countries, motor vehicle accident are the most prevalent cause of TBIs.
[3] In regions of the world that are currently experiencing gating and hostilities (Central America, the Middle East and Central Africa), military combat is the most prevalent cause of TBI.
[4] Traumatic brain injury (TBI) is significantly linked to a wide range of psychiatric conditions, including depression, anxiety, post-traumatic stress disorder (PTSD), and personality changes. These mental health issues can be acute or chronic, are common after both mild and severe TBIs, and are associated with worse health outcomes, decreased quality of life, and challenges with rehabilitation and independence.
[5]
Keywords:
Traumatic brain injury (TBI) - Depression- Post traumatic stress disorder (PTSD)- Anxiety- Personality changes
Introduction:
Discussion:
A TBI occurs when external forces act on the head causing brain damage that alters brain function’s can cause mild, moderate, or severe outcomes with symptoms ranging from altered mental state, memory issues, neurological deficits, permanent disability, or death. A widely accepted severity classification is based on the GCS applied at initial presentation.
• Mild Head Injury: GCS 13-15
• Moderate Head Injury: GCS 9-12
• Severe Head Injury: GCS 3-8.
Duration of PTA has also been proposed as a classification for mild, moderate and severe head injury:
• Mild: PTA ≤24 hours.
• Moderate: PTA 24 hours to 14 days.
• Severe: > 14 days to 8 weeks.
• Very Severe: > 8 weeks.
There is a clear biomechanical relationship between the type of TBI and the cascade of neurological deficits encountered:
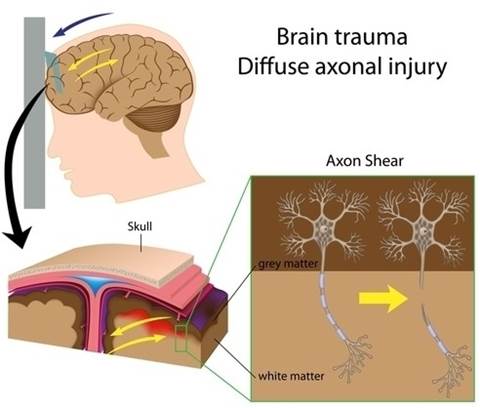
Contact forces acting on the head cause the brain to move inside the skull. This movement within the skull often causes damage to the temporal (ventral anterior, medial, and lateral temporal cortices) and frontal lobes. Rapid acceleration and deceleration cause damage mainly to axonal projections and blood vessels within the brain stem, the parasagittal white matter of the cerebrum, the corpus callosum, the grey- white junctions of the cerebral cortex, and the grey-white junctions in the ventral and anterior frontal and temporal lobes. TBIs involving penetration will ultimately depend on the entrance location, trajectory, and size of the object. Damage is caused by the projectile, bone fragments, and even via the introduction of potentially infectious material on the projectile. The neurobiological mechanisms of TBI involve the combination of focal damage and diffuse injury. Primarily, focal injury occurs at the time of the event and includes cortical and subcortical lacerations as well as intracranial bleeding. Diffuse injuries, on the other hand, are related to the pathological stretching and tearing of axons, otherwise known as a diffuse axonal injury (DAI).
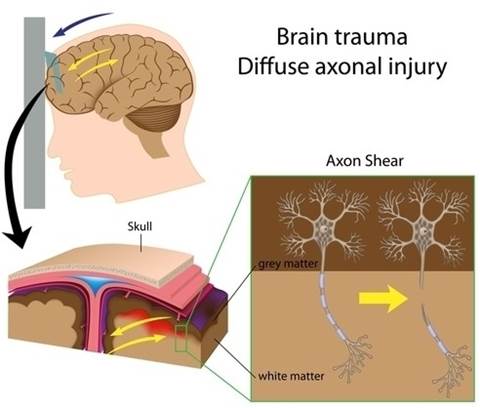
Figure No.1 (Brain Trauma and Diffuse axonal injury)
- There is a complex cascade of cellular and neurochemical effects that follow the initial trauma.
(6) (7) Firstly, the acute biomechanical damage of brain tissue is associated with the perturbation of neuronal membranes resulting in the influx of extracellular calcium ions and the efflux of potassium ions. The influx of calcium ions results in mitochondrial damage by reducing the production of ATP and increasing oxidative stress.These events cause the release of excitatory amino acids (e.g. glutamate) that bind to the N-methyl-D-aspartate
(NMDA) receptors, which results in further depolarization of the neuron. As calcium ion levels increase, there is the suppression of glucose metabolism. However, as the cell is attempting to restore ionic balance, this raises glucose consumption, which means that internal energy stores are depleted.Together, this creates an environment of anaerobic glycolysis and the overproduction of lactate, which causes acidosis, oxidative damage, and even cell death. A common consequence of TBI is the activation of microglial cells.
(8)Microglial cells are then known to migrate to injured brain tissue where they play an essential role in the inflammatory response after TBI. Microglial activation is necessary to clear up molecular and cellular debris at the site of damage. In the short term, microglia may have regenerative properties as they attempt to restore normal cellular function in damaged brain regions. However, when chronically activated, microglia are associated with the up-regulation of pro-inflammatory cytokines and other noxious inflammation mediators that result in further tissue and cellular dam .
Neutrophils and macrophages infiltrated at the site of the injury maintain neuroinflammation which affects the endothelium thus impairing the integrity of the blood-brain barrier, leading to increased extracellular fluid that, combined with cell swelling, leads to brain edema and increased ICP. There are several high-risk regions of the brain that are vulnerable to TBI. The that are involved in cognition and social behaviour are primarily involved.
• The neural circuits in the prefrontal cortex, which modulate executive functions such as working memory, decision making, problem-solving, and mental flexibility.
• The neural circuits arising from cells in the , which have a critical role in intuitive reflexive social behaviours and the capacity to self-monitor and self-correct in real time within a social context.
• The neural circuits starting in the , which regulate motivation and reward-related behaviours.
• Therefore, the severity and location of the brain injury play important roles in the resulting neuropsychological squealed. In one study they compared the frequency of psychiatric disorders in 939 patients with different severities of TBI. The prevalence of any psychiatric illness in the first year was 49% following a moderate-to-severe TBI, 34% following a mild TBI, and 18% in the control group that had no TBI. (9)
• A Finnish study which identified patients up to 30 years after a TBI showed rates as high as 48.3% for any psychiatric disorder and major depression was the most common diagnosis (26.7%). (10) and often coexist because brain injuries are often sustained during traumatic experiences. Recent military conflicts have revealed that there is a complex relationship between psychological and biomechanical trauma. (11) (12)
• One study, in particular, showed that there were higher rates of PTSD in Iraq war veterans who had reported a previous TBI in conjunction with loss of consciousness in comparison with veterans that reported other injuries, or no injuries. (13)
• Post TBI, patients with acute stress reaction are more likely to develop PTSD compared to those without (81% vs 11.5%)
• It is suggested that contact or impact forces to the hippocampus and amygdala are likely to be implicated in PTSD. The hippocampus and amygdala are brain regions that have networks associated with contextual memory consolidation and fear conditioning. Alterations in these circuits have been shown to trigger PTSD symptoms after the exposure to trauma.
• Moreover, the hippocampus is particularly vulnerable to the effects of traumatic stress. Therefore, TBI-related biomechanical forces and neurochemical stress-mediators could promote the development of PTSD.Interestingly, subjects with memories of the traumatic event are more likely to develop PTSD compared to those with amnesia of the event. Thus, although PTSD can occur with post-traumatic amnesia (PTA), PTA may have a protective role in the development of PTSD.
• The biomarker S-100B which is an astrocytic protein when raised in the acute phase of TBI is predictive of PTSD one year later. (14)
• The biological treatment of PTSD is no different to PTSD without brain injury with the exception that medication choices should take into account the sensitivity to side effects that can accompany TBI. Trauma-focused CBT may need to be adjusted to take into account cognitive impairments. Early CBT in the acute stress reaction phase post-trauma can prevent the development of PTSD. The proportion of patients with PTSD at 6 months was reduced from 58% to 17%. (15)
• Cognitive impairments are the most common complaints after TBI and can present substantial challenges to independent living, social re-adaptation, family life, and return to work.
• Frontal executive functions such as problems with problem-solving, impulse control, and self-monitori
depression has been found to be correlated with lower bilateral hippocampal volume and reduction of left frontal grey matter.Depression with anxious distress was related to injuries in the right hemisphere, while depression without anxious distress was related to anterior injuries on the left hemisphere. (14) (18)
regarding TBI and recovery expectations, reassurances, and frequent support is recommended. may decrease depressive, anxious, and anger symptoms as well as improve problem-solving skills, self-esteem, and psychosocial functioning following TBI. used to treat idiopathic depressive disorders are useful for the treatment of depression in patients with TBI. Due to concerns about the tolerability and effectiveness of TCAs in this population, :
Sertraline and Citalopram:
- Favoured due to their beneficial effects, relatively limited side effects, and short half-lives.
2. Limited by their relatively more significant potential for adverse effects and drug- drug interactions.
For example, fluoxetine and paroxetine are robust inhibitors of cytochrome P450 enzymes and are associated with problematic drug-drug interactions when co-administered with a substrate, inhibitor, or an inducer of these enzymes. Paroxetine also has significant anticholinergic effects, which increases the risk of treatment-related cognitive dysfunction among patients with TBI. SSRI are also effective for pathological laughter and crying. Depression complicated by brain injury can be treatment resistant. Therefore alternatives should be considered in the context of resistance.
is indicated in severe depression or prolonged stupor following head injury.
Mania associated with TBI may present with higher aggression, irritability and less euphoria. (19)
Injuries of the brain affecting the inhibitory function of the frontal lobes on the subcortical limbic structures is implicated in the development of mania. Mania is more common in individuals that have damage to the orbitofrontal and temporal cortex. Valproate is considered first line. Antipsychotic medications such as quetiapine, olanzapine and aripiprazole are useful with a caution that higher doses can reduce seizure threshold. The neuroprotective effect of lithium may be particularly useful in this group of patients. However, confusion, ataxia and reduced seizure threshold are potential side effects to be vigilant for. The term “personality change” is often used by family members and caregivers to describe the changes to patients after brain injury. The personality changes described are often challenging to address because the patient is often unable to appreciate that their behavior is different after the TBI. Responses can include verbal utterances, physical actions, snap decisions, and poor judgment of the implications of their actions. Responses can include verbal outbursts, aggressiveness, and assaultive behaviour that are characteristically out of proportion to the precipitating stimulus. Responses include exaggerated displays of emotional expression that are out of proportion. They often have a paroxysmal onset, brief duration, and are then followed by significant remorse. This is often misinterpreted as laziness or depression. It is also linked to aggression when attempts to engage the individual in activities that they have little interest in can precipitate assaultive behaviour. The cortico-striatal-pallidal-thalamic pathways (mediators of motivation) are likely to be affected.
Extreme apathy includes abulia and akinetic mutism. Pharmacological treatment of TBI patients with personality changes depends on the presenting symptoms. The literature is supportive of the use of psychotropic agents from several classes, including mood stabilizers, antipsychotics, and antidepressants.
However, there are no significant randomized controlled trials demonstrating the efficacy of one therapy over another. Stimulants, dopaminergic agonists or cholinesterase inhibitors can be tried for apathy, abulia and akinetic mutism. Responds well to Valproate and Carbamazepine. Antipsychotic medications can increase the risk of tardive dyskinesia and neuroleptic malignant syndrome (NMS). Benzodiazepines can result in paradoxical disinhibition.
• Head injury increases the risk of a chronic psychotic illness such as schizophrenia-like illness. Patients with a predisposition to psychosis are at highest risk.
• Delusions were the most common clinical feature with the content being persecutory, reference, control and grandiosity
Attention span
• Short-term memory and learning
• Speed of information processing
• Speech and language functions.These cognitive domains are often affected persistently due to significant injury to medial temporal regions, the dorsolateral prefrontal cortex, and subcortical white matter that connects these regions.
A recent meta-analysis also showed that head injury is associated with increased risks of dementia and Alzheimer’s disease (AD). (16)
Prof Fann and colleagues in 2018, published their research in the Lancet which showed that TBI was associated with an increased risk of dementia both compared with people without a history of TBI and with people with non- TBI trauma.
is indicated and highlights the areas of deficit and those of preserved function.
is useful for the treatment of impaired attention, interpersonal communication skills, and executive function following TBI. However, this form of treatment is only useful for patients with mild-to-moderate cognitive impairments who still have a degree of functional independence (e.g., methylphenidate, dextroamphetamine, amantadine, levodopa/carbidopa, bromocriptine) can modestly improve arousal and speed of information processing, reduce distractibility, and improve some aspects of executive function. Modafinil has been shown to promote wakefulness in patients with ABI. �Borghol et al., 2018�
(Donepezil and Rivastigmine) are useful and indicated in patients with significant memory impairment’s can also result in an increased risk of mood and disorders. Depressive disorders associated with TBI are categorized as Mood Disorders Due to Another Medical Condition (TBI) and are classified as follows: If the full criteria for a major depressive episode are met:
2. A depressed mood that does not meet the full criteria for a major depressive episode
3. When the predominantly depressed mood coexists with manic-like symptoms
These disorders differentiate from other common emotional disorders in patients with TBI, such as the transient disturbances of emotional expression and experience that occur in this population. This includes symptoms such as emotional lability and pseudobulbar involvement (pathological laughter and crying).Prevalence rates for depression vary from 18-61%. After head injury, the boundaries between depression, adjustment disorder and grief often overlap. Rupture of the neural circuits involving prefrontal cortex, amygdala, hippocampus, basal ganglia and thalamus may be implicated in the development of depression EEG abnormalities in the temporal lobe have been found in patients with psychosis, and some cases had seizures. Abnormalities in the frontotemporal lobes and the neurotransmitter pathways in these areas have been implicated in the development of psychosis.
Risperidone is effective based on case reports. Other alternative atypical antipsychotics are also reasonable. Clozapine may be indicated in treatment resistance, and a low threshold for prophylactic valproate should be considered due to the increased risk of seizures in this group of patients. Contact and inertial forces that act on the head initiate a cascade of cellular and neurochemical effects that cause a TBI. A TBI has short and long-term impacts and increases the risk of developing a psychiatric illness.
Conclusions:
Traumatic brain injury an important etiological factor in the appearance of psychiatric disorders. depression is the most prevalent psychiatric alteration after a TBI, becoming a sequel that shows a higher incidence in the first year after the traumatic brain injury The findings found in relation to post-traumatic stress disorder are controversial, showing great variability regarding the degree of severity. The prevalence of psychotic syndromes is relatively low because it is difficult to determine if the psychosis is a direct consequence of a TBI. In the cognitive sphere, it was found that people with TBI presented alterations in cognitive functions.
Conflict of Interest:
No Conflict Of Interest.
Financial support and sponsorship:
Nil.
Data Sharing and Data Accessibility Policy:
I Agree.