Clinical Medical Case Reports and Case Series
OPEN ACCESS | Volume 2 - Issue 1 - 2025
ISSN No: 3065-7644 | Journal DOI: 10.61148/3065-7644/CMCRCS
Berhe Tesfai 1*, Hailemichael Gebremariam 2, Okbu Frezgi1
1Department of Obstetrics and Gynecology, Orotta College of Medicine and Health Science, Orotta National Referral Maternity Hospital, Ministry of Health, Asmara, Eritrea.
2Dekemhare Hospital, Ministry of Health, Dekemhare, Eritrea.
*Corresponding author: Berhe Tesfai, Department of Obstetrics and Gynecology, Orotta College of Medicine and Health Science, Orotta National Referral Maternity Hospital, Ministry of Health, Asmara, Eritrea.
Received: March 03, 202
Accepted: April 06, 2025
Published: April 18, 2025
Citation: Berhe Tesfai, Hailemichael Gebremariam,Okbu Frezgi. (2025) “True Umbilical Cord Knot: Challenging Prenatal Diagnosis, Case Series, 2025.”, Clinical Medical Case Reports and Case Series, 2(1); DOI: 10.61148/3065-7644/CMCRCS/18
Copyright: © 2025. Berhe Tesfai. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
True cord knots are extremely rare, and commonly associated with neonatal mortality and prenatal identification is rare and challenging. All cases were multiparous mothers presented to Orotta National Referral Maternity Hospital with labor and three of them had previous cesarean section and delivered active neonates by cesarean section and one stillbirth. All the newborns were males with single loose true cord knot and long cord. High index of suspicion in patients with risk factors and intrapartum fetal monitoring decreases the associated fetal complications
Introduction
A true umbilical cord knot is defined as an entwining of a segment of the umbilical cord (1) and occurs when the umbilical cord twists around itself, forming a tight knot. (2) It can be loose without obstructing the blood flow to the fetus or tight enough to exsanguinate the fetus by compromising the blood flow towards the fetus. (3) True umbilical cord knot is a rare occurrence during pregnancy, with a reported incidence of 0.1 to 2.1% of all pregnancies. (1-7) Prenatal diagnosis of a true knot is a diagnostic challenge for the obstetrician (8), the diagnosis may be missed antenatally during routine ultrasonography (5) and it is mostly discovered at delivery, when the knot is identified. (9) High index of suspicion, routine doppler study of the umbilical cord especially in patients at risk of true knot formation and adequate intrapartum monitoring to ensue good pregnancy outcome (10) and four-dimensional and color doppler examination is very important to diagnose a true umbilical cord. (11)
The risk factors for true cord knots and long cord are advanced maternal age, multi-parity, history of stillbirth, obesity, prolonged gestation, male neonates, maternal anemia, gestational diabetes, polyhydramnios, long umbilical cords and fetuses with excessive moving associated with a doubled risk of intrauterine and perinatal death, and increased risk of adverse neonatal outcome. (2, 6, 12) Neonates with true umbilical cord knots often suffer extents of hypoxia in their prenatal course, which may cause fetal distress or even intrauterine death (10) and routine continuous cardiotocography can be the best modality to pick distress and achieve a good neonatal outcome. (3) True umbilical cord knot is mostly asymptomatic but can lead to a variety of adverse perinatal outcomes intra-uterine growth restriction, caesarean delivery and stillbirth. (4, 7-9)
Cases
First case: This was a 32-year-old gravida 4 para 3 Eritrean woman who had history of previous 2 Cesarean delivery came at term on latent phase of labor and had fetal bradycardia. With an indication of two previous cesarean section, fetal bradycardia on latent phases of labor, emergency cesarean section was made, and active male neonate was delivered cephalic. Intraoperatively, there was a true single loose knot with long cord (picture A), abdomen was closed without complications and discharged after 3 post-operative days.
Second case: This was a 28-year gravida 3 para 2 with history of one previous cesarean section, came with complaint of rupture of membrane at term pregnancy. She had labor pain and fetal heartbeat was 98b/m. Prevaginal examination revealed cord prolapse which was pulsating in latent phase of labor. Emergency cesarean section was performed and active male neonate was delivered cephalic. A single loose true cord knot was found incidental (Picture b, c), and the post-operative period was uneventful.
Third case: This was a 27-year gravida 2 parity 1 woman with history of one previous scar came with labor pain at term pregnancy The presentation was breech and fetal heartbeat of 132b/m. Ultrasound revealed confirmed breech presentation and had normal doppler studies. She delivered by emergency cesarean section a 3.4kg male neonate with good APGAR score. Intraoperatively, a loose, single, true knot with long cord was detected (Figure: d) and the post operative period was uneventful and discharged after 3 days.
Fourth case: This e was a 29-year gravida 2 parity 1 woman came on second stage at term pregnancy. Fundal height was term, longitudinal lie, cephalic presentation, with absent fetal heartbeat. She delivered a 3kg, male fresh stillbirth vaginally and single true cord knot without visible congenital anomalies was noted and discharged after 6 hours hospital stay.
a b
b c
c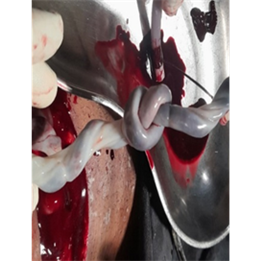 d
d 
Discussion
True umbilical cord knot is a pathology with relatively low very incidence (2, 4, 5, 7, 8) and health professionals’ awareness and antenatal assessment on patients with risk factors is very crucial to increase the detection rate.
Prenatal identification of a true knot is challenging and all our cases were diagnosed postpartum, consistent with other literatures and its detection in-utero often goes unnoticed until delivery (2, 8) and the diagnosis may be missed antenatally during routine ultrasonography. (5, 6) High index of suspicion on patients with risk factors and unexplained fetal distress may help to prevent the perinatal complications and increased stillbirth rate in neonates with true knot.
True cord knots are generally single and loose as in all our cases, which could be mainly the reason why three of them were delivered alive and reports indicated that one true tight knot was noted, resulted stillbirth. (3, 7) Similarly, other reports indicated that incidental finding of a single loose cord knot at delivery. (9, 10, 13) Tight true knot may result in fetal complications but, in most cases the Wharton’s jelly protects from tight knot, consistent with a case report that Wharton’s jelly and hydrostatic pressure of the umbilical vessels usually do not allow knots to completely tighten, but just before or during labor, a previously loose knot can tighten and cause asphyxia. (1)
Fetal distress is one of the initial clinical presentation of patients with cord knot in labor, due to compromising of blood flow to the fetus, like our cases which can be associated with increased risk of intrauterine demise. This was consistent with many case reports that the main intrapartum findings were alterations in the cardiotocography, such as variable and late decelerations and associated with low Apgar scores, fetal distress, caesarean delivery and stillbirth. (4, 7, 8, 12)Routine continuous cardiotocography can be the best modality to pick distress at the earliest time and prevent perinatal mortality. (3)
Our cases had risk factors as multiparty, long umbilical cord and a male fetus and one case had cord prolapse, which is associated with long cord and predisposes them to true knot. Similarly, other studies reported that the risk factors mentioned are long umbilical cord, polyhydramnios, male fetus, gestational diabetes, and multi-parity. (2, 6, 7) Therefore, on patients with the above-mentioned risk factors, antenatal evaluation and intrapartum monitoring for true knot is critical.
Three of our cases delivered alive neonate by cesarean section, as they had previous cesarean section presented with fetal distress and the fourth case was a stillbirth. This was consistent with other study that true knot was associated with emergency cesarean delivery due to non-reassuring fetal heart rate (2, 5) and intrapartum fetal monitoring is vital and neonates could be saved by emergency cesarean section.
Conclusion
True knot is an extremely rare clinical incidence, difficult to diagnose on antenatal and high index of suspicion for those with risk factors and proper intrapartum monitoring is highly recommended to prevent the perinatal complications.
Declaration
Acknowledgments: Authors acknowledges for the hospital staff for management of the cases
Informed consent: All the patients gave written informed consent for publication and use of their data for educational purpose.
Competing of interest: Authors have no competing of interest to disclose
Author Contributions: All authors have contributed to writing the case report and all reviewed and approved the final version of the case report.