Clinical Medical Case Reports and Case Series
OPEN ACCESS | Volume 2 - Issue 1 - 2025
ISSN No: 3065-7644 | Journal DOI: 10.61148/3065-7644/CMCRCS
Ravi Patel DO1*, Samer Asmar MD2, Richa Patel MD3, Ruben Kandov MD4
1Department of Internal Medicine, Zucker Hofstra Northwell Health at North Shore University Hospital.
2Department of Internal Medicine, Zucker Hofstra Northwell Health at Staten Island University Hospital.
3University of Illinois, Peoria, Illinois.
4Department of Cardiology, Zucker Hofstra Northwell Health at Staten Island University Hospital.
*Corresponding author: Ravi Patel, Department of Internal Medicine, Zucker Hofstra Northwell Health at North Shore University Hospital.
Received: July 16, 2025 |Accepted: July 24, 2025 |Published: July 28, 2025
Citation: Patel R, Asmar S, Patel R, Kandov R. (2025) “Case Report: ST Elevation Myocardial Infarction in a Mid-Twenties’ Male Patient with COVID Pneumonia.”, Clinical Medical Case Reports and Case Series, 2(1); DOI: 10.61148/3065-7644/CMCRCS/057
Copyright: © 2025. Ravi Patel. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
This report describes a case of a mid-20s male patient who presented with ST-elevation myocardial infarction (STEMI) and tested positive for Coronavirus Disease 19 (COVID-19). COVID-19 is known to cause myocardial injury, and patients with active COVID-19 infections presenting with acute STEMI have varying outcomes. The optimal management strategy for patients with COVID-19 and concurrent STEMI is challenging, with fibrinolytic therapy gaining attention as a potential treatment option. However, findings from a large case series of COVID-19 positive patients presenting with STEMI who were treated with PCI reported a higher rate of stent thrombosis, emphasizing the need to monitor thrombotic events in this population. Further research is needed to address unanswered questions about this select patient population. For COVID-19 negative patients presenting with STEMI, PCI within 90 minutes of hospital presentation is recommended, and this recommendation remains applicable during the COVID-19 pandemic. The Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American Heart Association (AHA) recommend pursuing PCI in STEMI patients during the COVID-19 pandemic, and ongoing observational registries support this recommendation.
COVID; STEMI; Emboli Foot Line: STEMI in a young adult with COVID
Systemic viral infections have been associated with acute myocardial infarction and inflammation which may act as a pathological trigger for acute plaque rupture and thrombosis [1,2]. Coronavirus Disease 19 (COVID-19) caused by Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-CoV-2) is a multi-organ disease with a wide array of clinical presentations [3]. Among hospitalized patients with COVID-19 infection, myocardial injury detected by biomarkers of cardiac insult is as high as 20% to 30% [4]. Notably, myocardial injury may present with electrocardiographic features of ST-segment elevation myocardial infarction (STEMI) [5]. The prognosis of STEMI patients with COVID-19 infection is highly variable with reports of inpatient mortality ranging from 12% to 72%. [1,6] Despite the growing literature pertaining to COVID-19 positive individuals, little is known about the specific clinical characteristics and outcomes of patients with active COVID-19 infections presenting with acute STEMI. Here, we report a case of acute STEMI in a young patient who tested positive for COVID-19.
Case Presentation:
A male patient in his mid-twenties, with a past medical history of COVID pneumonia about a year ago, presented to the hospital emergency department complaining of chest pain.
According to the patient, the chest pain woke him up from his sleep around 1 am on the day of admission. The chest pain was characterized as sharp, retrosternal, and non-radiating. It worsened when he lay down and improved when he sat up. He also had two episodes of nausea and vomiting the morning of hospitalization around 6 am. He was about to leave for work when he spoke to his family member who works in healthcare. They advised him to go to the hospital for his symptoms, and therefore, he presented to the hospital.
The patient reported that he tested positive for COVID approximately one to two weeks prior to hospitalization and was asymptomatic when he had his COVID test performed. He received two Pfizer COVID vaccines as his primary series of COVID vaccination. The patient also reported that he has been experiencing chest discomfort since being infected with the COVID-19 virus last year and that his primary care physician diagnosed him with costochondritis for his pain.
In the emergency department, the patient's vital signs were stable with a blood pressure of 139/85, heart rate of 58, temperature of 95.4°F, respiratory rate of 18, and oxygen saturation of 100% on room air. Physical exam was unremarkable. His initial labs were significant for a white blood cell count of 16.57, predominantly neutrophils, elevated monocytes 1.44, elevated myelocytes 1.7%, and decreased lymphocyte % 15.7 with a normal lymphocytes value of 2.60, elevated calcium 10.2, elevated anion gap 15, elevated alkaline aminotransferase (ALT) 69, elevated lactate 4.70, and elevated troponins 0.05. The patient tested positive for COVID-19 PCR in the emergency department.
Chest X-ray did not show any acute cardiopulmonary disease [Figure 1]. Initial EKG showed concave upsloping ST elevations in leads II, III, aVF, V2, V3, V4, and V5 as shown in Figure 2, and therefore a code ST segment elevation (STEMI) was called. A repeat EKG showed persistent ST elevations in leads V2-V4, new T-wave inversions in lead III, avF, new ST elevations in lead I, aVL as shown in Figure 3.

Figure 1: Chest X-ray showed no signs of acute cardiopulmonary diseases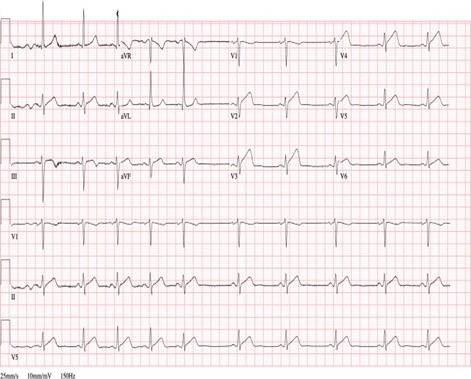
Figure 2: Initial EKG revealed concave upsloping ST elevations in leads II, III, aVF, V2-V5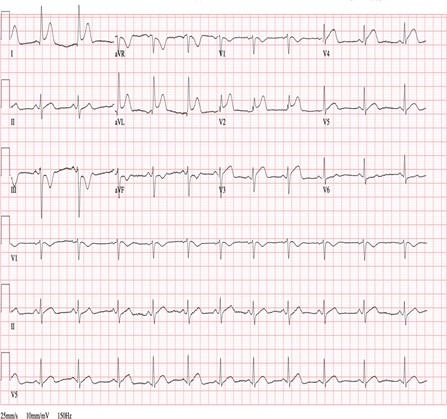
Figure 3: Electrocardiogram (EKG) shows ST elevations in leads I, aVL, V2-V4, and T-wave inversions in lead III, aVFThe patient was immediately taken to the cardiac catheterization lab, where a left heart catheterization revealed 90% thrombotic occlusion of the proximal and 100% occlusion of the distal Left Anterior Descending artery (LAD), as shown in Figure 4.
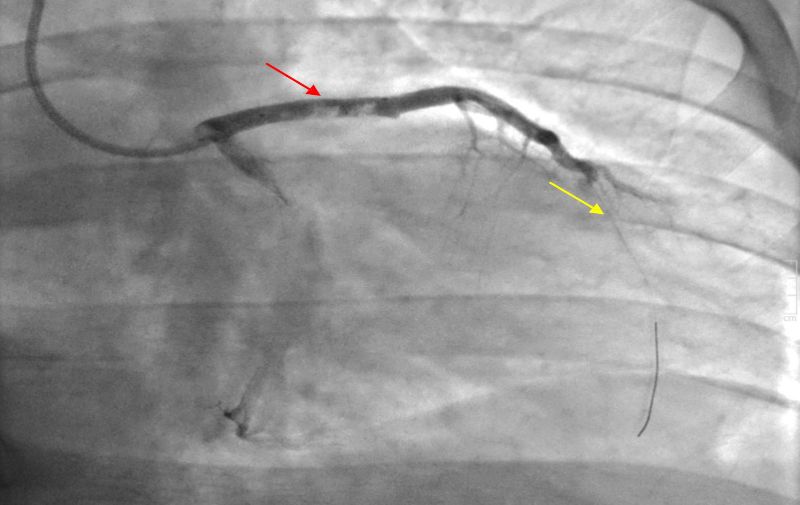
Figure 4: Angiograph indicated the presence of thrombi obstructing 90% of the proximal (red arrow) and 100% of the distal (yellow arrow) Left Anterior Descending artery (LAD).
Two drug-eluting stents – 4.0 X 20 Synergy XD and 4.0 X 8 Synergy XD – were placed in the proximal LAD lesion. There was TIMI 2 flow before, and TIMI 3 flow after the intervention was performed on the proximal LAD. Mechanical thrombectomy with a CAT6 RX kit and balloon angioplasty was performed on the distal LAD lesion. TIMI 0 flow improved to TIMI 2 flow after the procedure [Figure 5]. Blood flow to other coronary artery branches was normal. The patient was subsequently admitted to the Coronary Care Unit, where he underwent a significant hypercoagulability workup.

Figure 5: Angiograph conducted after the interventions showed the placement of two drug- eluting stents in the proximal LAD (red arrow) and the performance of thrombectomy with balloon angioplasty in the distal LAD (yellow arrow).
Subsequent labs showed an elevated C-reactive protein (CRP) level of 6.7, an elevated serum lactate dehydrogenase (LDH) level of 566, an elevated triglyceride level of 250, an elevated total cholesterol level of 276, an elevated LDL (low-density lipoprotein) cholesterol level of 174, a normal HDL (high-density lipoprotein) cholesterol level of 51, a d-dimer level less than 150, ferritin 336, and a serum pro-brain natriuretic peptide (pro-BNP) level of 9. The Transthoracic Echocardiogram revealed a moderately reduced ejection fraction of 40%, along with a moderate decrease in the left ventricular systolic function of the apical inferior, lateral, and septal segments.
The patient was discharged home on 81 mg aspirin once daily, 75 mg Plavix once a day, sacubitril-valsartan 24-26 mg twice a day, Xarelto 20 mg once a day, atorvastatin 40 mg once a day, metoprolol succinate 50 mg once a day, and pantoprazole 40 mg once a day.
Discussion:
Acute ST-elevation myocardial infarction (STEMI) is a serious condition associated with high morbidity and mortality rates, which are influenced by patient characteristics. Older age, female sex, medical comorbidities, anterior MI, and underlying coronary artery disease are all associated with worse outcomes in these patients [7]. Recent evidence suggests that acute respiratory viral infections, including influenza, can act as triggers for acute STEMI, with influenza increasing the risk of morbidity and mortality [2,8] Therefore, it is plausible that COVID-19 infection and the subsequent systemic inflammatory response may have triggered the STEMI event in our patient.
The optimal management strategy for stable patients presenting with COVID-19 and concurrent STEMI poses a challenge. Fibrinolytic therapy has gained attention as a potential treatment option for this patient population [9]. In China, experts recommend fibrinolytic therapy over primary percutaneous coronary intervention (PCI) for stable STEMI patients with COVID-19 who present within 12 hours of symptom onset and have no contraindications for fibrinolytics [10] This recommendation is based on the need to carefully balance healthcare provider exposure and patient benefit [11] However, findings from a large case series of COVID-19 positive patients presenting with STEMI who were treated with PCI reported a higher rate of stent thrombosis (21%) than previously reported rates of early stent thrombosis (1%) [1,12]. This highlights the need to adapt STEMI management for COVID-19 patients and underscores the importance of monitoring thrombotic events in this population. Many questions remain unanswered about this select patient population, and further research is needed.
For COVID-19 negative patients presenting with STEMI, the current standard of care is PCI within 90 minutes of hospital presentation. Fibrinolytic therapy is recommended if there is an expected delay of more than 90 minutes to PCI [13,14]. The Society for Cardiovascular Angiography and Interventions (SCAI), the American College of Cardiology (ACC), and the American Heart Association (AHA) recommend pursuing PCI in STEMI patients during the COVID-19 pandemic [15] An ongoing observational registry created under the guidance of these cardiology societies supports this recommendation, as PCI is feasible and remains the predominant reperfusion strategy for COVID-19 positive patients presenting with MI [16].
Conclusion:
The COVID-19 pandemic has posed a challenge to the management of STEMI patients. While PCI remains the standard of care for COVID-19 negative patients, fibrinolytic therapy has gained attention as a potential treatment option for stable COVID-19 positive patients. However, the risk of thrombotic events in this population underscores the importance of careful patient selection and monitoring. Further research is needed to guide the optimal management strategy for this select patient population.