Clinical Medical Case Reports and Case Series
OPEN ACCESS | Volume 2 - Issue 1 - 2025
ISSN No: 3065-7644 | Journal DOI: 10.61148/3065-7644/CMCRCS
Vishnu Sharma1, Aayush Kulshreshtha2*, Vansh Bagrodia3, Komal Agarwal4
1Associate Professor, Department of Clinical Hematology, SMS Medical College, Jaipur.
2Department of Emergency Medicine, Fortis Escorts Hospitals, Jaipur, Rajasthan, India.
3Intern, SMS Medical College, Jaipur, Rajasthan, India.
4Department of Medicine, RUHS College of Medical Sciences, Jaipur, Rajasthan, India.
*Corresponding author: Aayush Kulshreshtha, ADepartment of Emergency Medicine, Fortis Escorts Hospitals, Jaipur, Rajasthan, India.
Received: June 01, 2025
Accepted: June 10, 2025
Published: June 15, 2025
Citation: Sharma V, Kulshreshtha A, Bagrodia V, Agarwal K. (2025) “Acute Interstitial Nephritis and Seronegative Polyarthritis as Presenting Manifestations in a Case of Multiple Myeloma.” Clinical Medical Case Reports and Case Series, 2(2); DOI: 10.61148/3065-7644/CMCRCS/021.
Copyright: © 2025 Aayush Kulshreshtha. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited
A 39-year-old male presented with 18 months of bilateral symmetrical polyarthralgia, progressive joint swelling, and significant weight loss. Initial investigations revealed mild renal dysfunction and were negative for common rheumatologic markers. The patient experienced multiple admissions for unexplained renal insufficiency and was eventually diagnosed with AIN. Neurological symptoms led to a diagnosis of carpal tunnel syndrome, and MRI findings indicated erosive arthritis and synovitis. Suspecting an underlying malignancy, hematologic evaluations confirmed MM with renal biopsy revealing light chain cast nephropathy and bone marrow biopsy showing extensive plasma cell infiltration. The patient responded well to bortezomib therapy
Multiple myeloma, seronegative polyarthritis, acute interstitial nephritis, atypical presentation, renal dysfunction
Introduction
Multiple myeloma (MM) is a clonal plasma cell proliferative disorder characterized by the abnormal increase of monoclonal immunoglobulins. Malignant clonal plasma cells secrete an excess of either intact immunoglobulins or free light chains of a single type, called monoclonal proteins (M-protein). The most common type of M-protein is IgG, followed by IgA and light chain only . [1] These proteins infiltrate tissues and organs, leading to various clinical symptoms such as hypercalcemia, renal dysfunction, anemia, or bone pain accompanied by lytic lesions.
The diagnosis of MM is established when at least 10% clonal plasma cells are present in the bone marrow or a biopsy-proven plasmacytoma is found, and at least one myeloma-defining event is present. Myeloma-defining events include evidence of end-organ damage (hypercalcemia, renal insufficiency, anemia, or bone lesions) or biomarkers of malignancy (≥ 60% clonal bone marrow plasma cells, involved/uninvolved serum free light chain ratio ≥ 100 (involved serum free light chain level ≥ 100 mg/L), or > 1 focal lesion on MRI studies of ≥5 mm in size) .[2]
Case Report
A 39-year-old male was referred to us by the rheumatology department as a suspected case of multiple myeloma. The patient had a noteworthy history of bilaterally symmetrical polyarthralgia for 18 months, predominantly on the right side, with the main joints involved being the shoulder, hip, wrist, and knee. The pain was progressive, associated with joint swelling and limitation of movement. He also reported a 30% weight loss during this period.
The patient initially did not consult a physician for the polyarthralgia for a year from its onset and self-medicated with pain medications. He first reported to the hospital in September 2023 with complaints of sudden severe abdominal pain along with nausea and vomiting. The patient also mentioned chronic bilateral polyarthralgia during his history and was duly investigated. Most of his reports were unremarkable except for a USG, which suggested findings of fatty liver grade III and bilateral mild renal dysfunction (grade 2) with elevated serum creatinine levels (3 mg/dL). He was referred to the nephrology department, where a diagnosis of acute interstitial nephritis was made, and he was placed on supportive treatment. The patient was discharged with stable vitals in a few days, but elevated creatinine levels on multiple follow-ups called for repeated admissions. A renal biopsy was advised, but the patient did not consent and requested discharge with supportive treatment, with the polyarthralgia still present.
Three months later, the patient presented to the neurology department of our tertiary care center with complaints of decreased handgrip with weakness and pain in all four limbs. On examination, swelling was noted in all the joints involved in his chronic complaint of polyarthralgia. A diagnosis of carpal tunnel syndrome was made for the decreased handgrip. However, the polyarthralgia remained unexplained, and the patient was referred to the rheumatology department for his myriad symptoms.
The patient underwent another round of extensive investigations which included notable findings: Hemoglobin [9.6 g/dL, N = 12-18 g/dL], Serum urea [61.10 mg/dL, N = 10-50 mg/dL], Serum Creatinine [2.50 mg/dL, N = 0.6-1.5 mg/dL], Serum uric acid [10.3 mg/dL, N = 3.5-7.2 mg/dL]. ANA, RF, anti-CCP, HLA-B27 were all negative, thus ruling out the specific conditions associated with these markers. MRI of B/L shoulder and hip joint and USG of wrist and knee joints suggested erosive arthritis and synovitis.
The rheumatology department concluded a diagnosis of seronegative erosive polyarthritis. Considering findings such as anemia, bone pain, proteinuria, and kidney injury, they sought our opinion with a suspicion of multiple myeloma. We conducted a urine examination, bone marrow aspiration, renal biopsy, and β2 microglobulin testing, which are detailed in Table 1.
A diagnosis of multiple myeloma, R-ISS stage 3 (High Risk), was confirmed based on his reports. He was then started on Bortezomib and reported significant improvement in all of his symptoms.
|
Parameter |
Observed Value |
Reference Range |
|
Serum β2 microglobulin |
16599 ng/mL |
609.0-2366.0 ng/mL |
|
Urine total protein |
250 mg/dL |
- |
|
Urine creatinine |
30.60 mg/dL |
- |
|
Urine protein/creatinine ratio |
8.2 |
0-0.2 |
|
Urine immunofixation: kappa |
34 mg/L |
|
|
Urine immunofixation: lambda |
15279.66 mg/L |
|
|
Urine Bence Jones protein |
Present |
|
|
Renal Biopsy |
Findings in table 2 |
|
|
Bone Marrow Biopsy |
Findings in table 2 |
Table 1: Investigations Conducted by Hematology Department
|
BIOPSY |
FINDINGS |
|
Renal Biopsy |
Glomeruli with irregular thickening and wrinkling of GBM and severe tubular injury with presence of granular, cellular broad hyaline was seen. IF findings showed positive Lambda casts. Overall LM & IF findings are in favour of lambda Light Chain Cast nephropathy.
|
|
Bone Marrow Biopsy |
Hypercellular bone marrow with suppressed hematopoiesis and replaced by sheets of plasma cells |
Table 2: Biopsy Findings
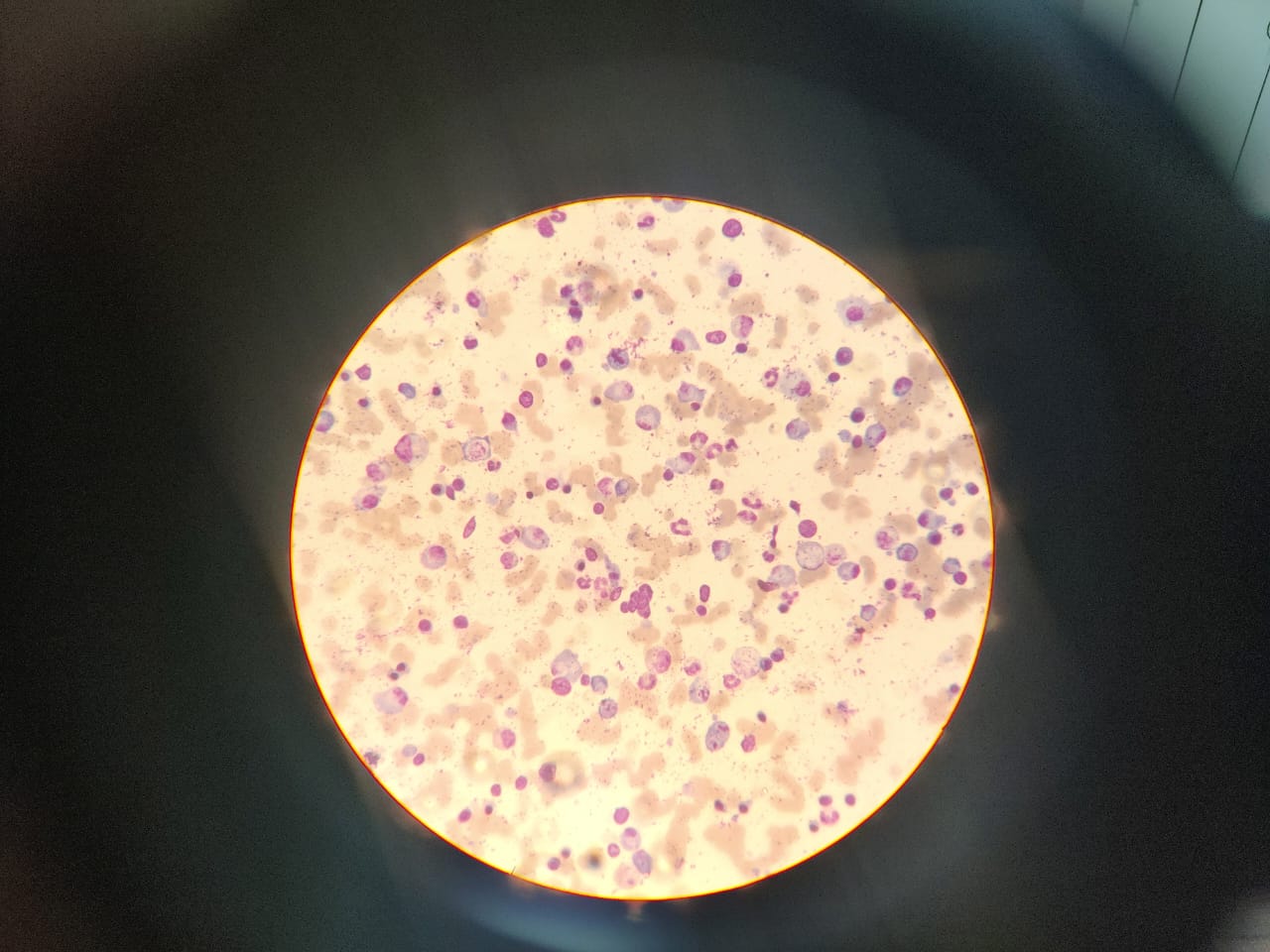
Figure 1: Hypercellular bone marrow with suppressed hematopoiesis
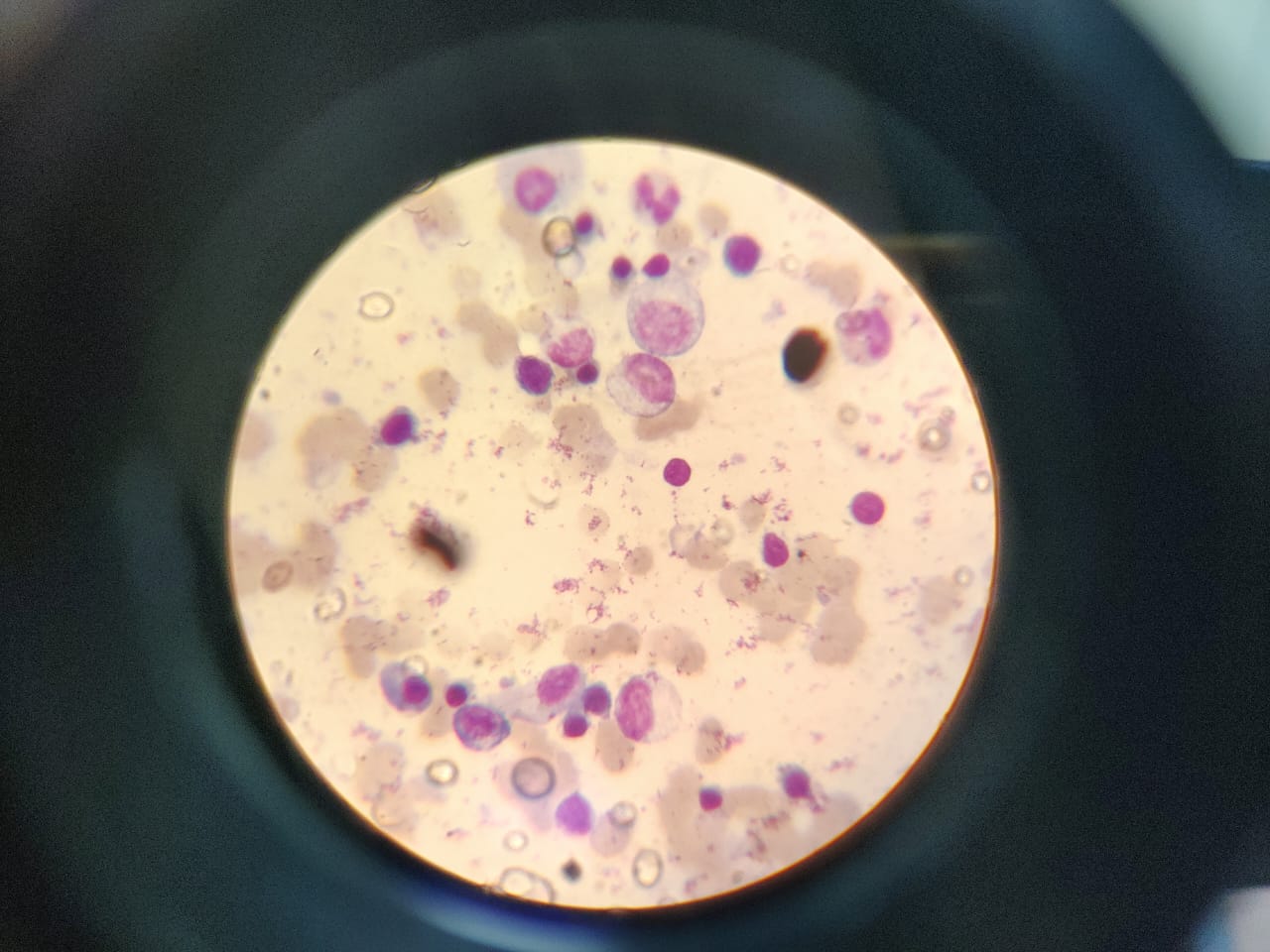
Figure 2: Hypercellular bone marrow with sheets of plasma cells
Discussion
Symptomatic manifestations of multiple myeloma generally involve bone pain, weight loss, and renal dysfunction, while generalized osteopenia, lytic bone lesions, and erosions are common skeletal manifestations of MM [3].
Polyarthralgia can have symptoms such as joint pain, tenderness, stiffness, swelling, and restricted movement. Chronic polyarthritis narrows the diagnosis towards rheumatoid or psoriatic arthritis, osteoarthritis, or gout.Polyarthritis can be severe enough to require emergency intervention or may remain undiagnosed for months, similar to the case where patient self-medicated with NSAIDs for symptomatic relief .
The patient first mentioned his chronic bilateral symmetrical polyarthralgia when he came to the ER for severe abdominal pain.Given his primary diagnosis was AIN and the patient not being cooperative,was discharged after supportive treatment with renal biopsy deferred due to lack of consent. No work-up could be done for polyarthralgia then. Three months later, the patient was diagnosed with carpal tunnel syndrome and subsequently referred to the rheumatology department due to his long history. Specific markers like ANA, RF, anti-CCP were negative, but MRI of B/L shoulder and hip joints revealed adhesive capsulitis changes, long head of biceps tendinitis with subcoracoid bursitis, and bilateral iliopsoas bursitis with hip joint effusion. The pathology was concluded to be seronegative erosive polyarthritis. However, with findings of anemia, proteinuria and weight loss with kidney injury, the patient was referred to us with a suspicion of multiple myeloma. MM was confirmed with bone marrow aspiration, renal biopsy, and β2 microglobulin testing.
Much of his earlier presentations could now be explained by MM. It can be theorized that light-chain molecules are filtered across the glomeruli or secreted and resorbed by the renal tubuli. Thereafter, an immune hypersensitivity reaction between the intratubular and interstitial-implanted light chains could have resulted in AIN .[4] Chronic interstitial nephritis and fibrosis are common findings in myeloma patients [4]; however, AIN as seen in our case is rare in MM, which is why it was not initially considered.
Peripheral neuropathy can be provoked via several mechanisms: M protein produced by malignant plasma cells, deposits of light-chain immunoglobulins in nerve cells, or radicular or medullar compression in myeloma bone disease [5]. Carpal tunnel syndrome may develop from intrasynovial deposition of amyloid protein or immunoglobulins [6].
Articular manifestations in MM are often related to amyloidosis, metabolic complications, and sometimes immunoglobulin deposit [4]. Pathology due to amyloid deposition is referred to as myeloma-associated amyloid arthropathy (MAA). The clinical presentation of MAA mimics arthritis and lacks specificity, where RF and CCP are usually negative. Serum and urine M protein screening can identify plasma cell diseases of such nature [7].
MM rarely presents with signs of arthritis, with shoulder joints being the most commonly affected, followed by the knee, wrist, hip, and metacarpophalangeal joints [7]. Joint involvement in myeloma typically presents as oligoarthritis or mimics a polyarticular rheumatoid-like pattern [6]. Synovial precipitation of paraproteins or immunoglobulin crystals may activate the inflammatory response leading to arthritis .
In a review by Schoninger et al., only three cases of MM initially presented as seronegative arthritis, with the shoulder, knee, wrist, and hip joints being involved [8]. In a review by Ahmed M. Elsaman et al., in 63 cases between 1931 and 2012, arthritis was the presenting manifestation, preceding the diagnosis of MM by 1–84 months, while the latency period in our case was 18 months. Erosive arthritis and MM were diagnosed as part of the same medical evaluation in only eight cases, similar to our case [9].
Overall, this case illustrates an atypical presentation of MM mimicking seronegative arthritis features, thereby challenging the diagnosis and further delaying the treatment of life-threatening malignancies.
Declaration
Ethics approval and consent to participate
Ethical approval was not required for this case report in accordance with the policies of SMS Medical College, Jaipur Rajasthan. Written informed consent was obtained from the patient for participation in this case report.
Consent for publication
Informed Consent was obtained from the patient.
Availability of data and material
Not applicable
Competing interests
Not applicable
Funding: Not applicable
Authors' contributions
Dr. Vishnu Sharma conceived of the presented idea. Dr. Aayush Kulshrehtha, Dr Vansh Bagrodia and Dr. Komal Agarwal wrote the main body of the paper. Dr. Vishnu Sharma verified the paper written by Dr. Aayush Kulshreshtha, Dr Vansh Bagrodia and Dr. Komal Agarwal and made technical corrections. Dr. Vishnu Sharma encouraged Dr. Aayush Kulshreshtha, Dr Vansh Bagrodia and Dr Komal Agarwal to investigate further literature on the topic so as to provide latest updates. All authors contributed to the final manuscript.
We know of no conflicts of interests associated with this publication, and there has been no significant financial support for this work that could have influenced its outcome. As Corresponding Author, I confirm that the manuscript has been read and approved for submission by all named authors.
We thank you for considering the manuscript.
Acknowledgements
Not applicable