Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
D. Persoons
Orthopaedic surgeon, CH. Of Saverne, France
*Corresponding author: D. Persoons, Orthopaedic surgeon, CH. Of Saverne, France.
Received: November 04, 2021
Accepted: November 09, 2021
Published: November 12, 2021
Citation: D. Persoons “The “Nail-o-flex” Nail as a New Procedure in distal Radius Fractures. A continuous Series of 105 Cases.” Clinical Case Reports and Clinical Study, 5(4); DOI: 10.61148/2766-8614/JCCRCS/100
Copyright: © 2021 D. Persoons. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Distal radius fractures are a daily problem in the elderly. Its treatment remains a critical challenge due to the number of cases, the final cost of the intervention, the level of X-ray irradiation and a demanding fixation of the fragments in osteoporotic bone. The entire closed procedure requires strict percutaneous nailing. This offers advantages in terms of postoperative pain, intraoperative radiation and cost. The main problem so far has been the ability to ensure a stable reduction in time. This point is discussed with the introduction of the “Nail-o-flex®” nail. A continuous series of 105 patients is introduced.
The fracture of the distal radius is common (1) and even the third most common in seniors (15% of fractures in seniors). It is estimated that 150,000 people suffer a fracture of the distal radius each year in France (2). The simplicity, efficiency and low cost of the surgical intervention are decisive factors in terms of public health. Therefore, their mechanism should be better understood (3,4,5). The difficulty in treating distal radius fractures comes from osteoporotic bone and crushed and often unstable fractures. It is indeed necessary to restore the correct length of the spoke to allow the proper functioning of the radioulnar joint. Thus the patient can find a normal pronosupination, and therefore a normal life. The radius is a long bone, relatively straight, and often subject to fractures due to its protective role in the event of a fall or accident. Long wires were first used during the First World War while flexible pins were described as early as the 1950s. Several types of flexible nails dedicated to distal fractures appeared in the early 2000s. Today, there are wires specially designed for fractures of the radial diaphysis.
During a fall, the wrist undergoes a force of compression and bending which causes a crushing of the bony trabecular structure of the distal radius. Cortical rupture is accompanied by the flattening of the deep cancellous bone. At the time of the fall, a crushing of the bone occurs in the distal radius, a compaction which results in a vacuum called "compaction chamber". This bone void explains the failures of the treatment with pins or plaster. As bone is missing, the focus will usually crush a second time after reduction (secundary displacement). This principle was described by Desmanet in 1989 (18) Some implants have even been specially designed to fill the void into the compaction chamber (fig. N° 1). It is therefore possible to view the volume of this compaction chamber. This aspect confirms the absence of cancellous bone inside the radical metaphysis, before starting osteosynthesis.

Fig 1: implant expansible Conventus DRS®
Those intra-fracture implants have the disadvantage of being bulky and not providing any mechanical stability. However, they widely open the fracture focus and they reveal the volume of bone loss at the distal metaphysis level.
2. The reduction :
The fracture of the distal radius is reduced by manual traction. It disimpacts the fracture site and reopens the metaphysis. The nail, as a central stake, maintains the reduction and the void thus created.
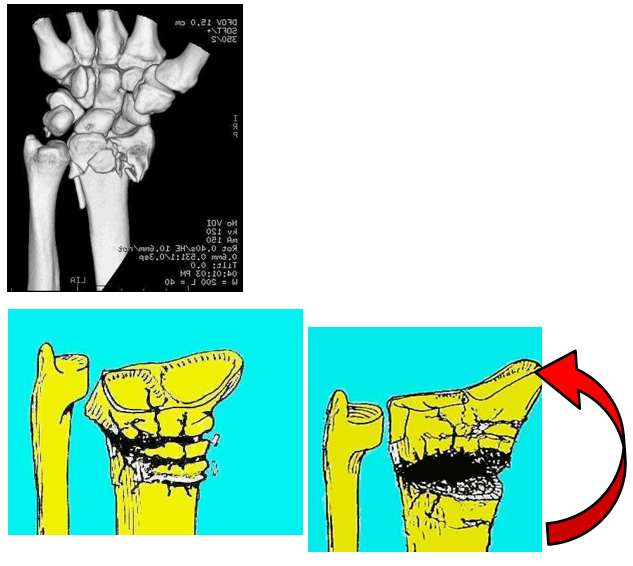
Fig 2 : fracture of the distal radius with the crushing of the metaphyseal bone
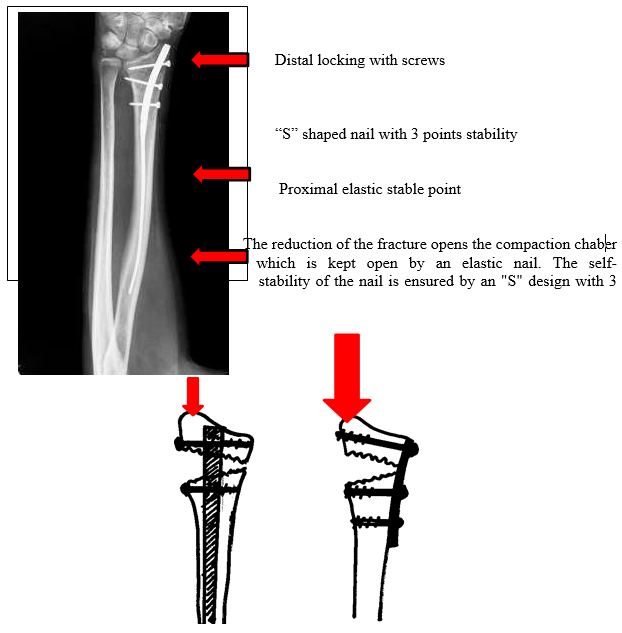
Fig 4: moment of the compressive force exerted on the locking screw of the nail and the palmar plate
3) Nailing history:
It seems to be logical to consider the best treatment of a bone void is to place a stake in the middle of this bone, and fix it above and below. The nailing of long bones, even with severe bone defects, was described by R. Danis of the University of Brussels (Belgium) in 1938 and by G. Küntscher at the University of Kiel (Germany) in 1939. The later used his nails on the wounded of the Finnish front during the Second World War. (5, 6) The transverse locking of the nail has been described by Modny and Bambara in 1953. (7) This lock was improved by Kempf and Grosse (9 ) in 1978 to the point where it prevailed over the screw plate osteosynthesis which became very popular in the 1960-1980. This method has revolutionized the treatment of long bones fractures of the lower limbs. Since the year 2000, it has been applied to the upper limb by drawing smaller, miniaturized nails as it were. The goal was to go back to closed-focus osteosynthesis, as done for the lower limbs.
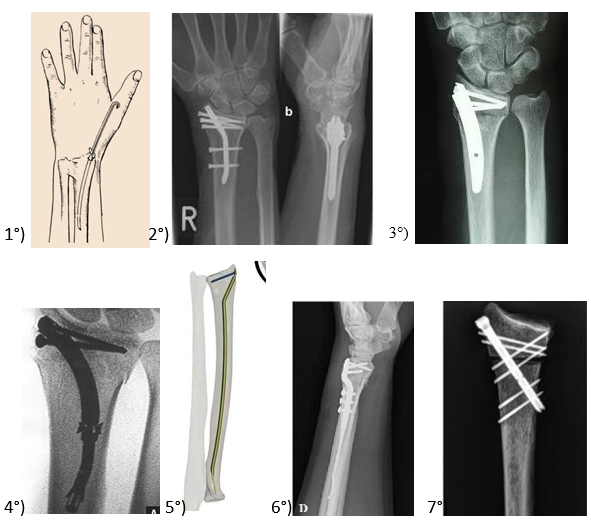
Fig n° 5 : various nails for radius fractures : 1) Rusch nail (1955), 2) targon® nail, 3) micro-nail®,4) Rin® nail 5) Sonoma®nail, 5) Rin® nail, 6) « DNP » dorsal nail-plate 7) Zimmer “X-Screw“® locked screw.
Most recent series seem to show the equivalence of radiological and functional results, between closed nailing and the anterior plates. "The present study supports the view that intramedullary nail fixation and flat fixation for the treatment of displaced extra-articular distal radius fractures have equivalent radiographic and functional outcomes”( 6 ). The major point is to restore the length of the radius despite a bone defect , and the best way seems to perform a static locked nailing.
4 ) Nail-o-flex® nail
The Nail-o-flex® nail was introduced in 2005. It is a specific nail for fractures of the distal radius. It comprises a distal portion which is perforated and a long, smooth proximal part that is thin and flexible to ensure elasticity. The nail-o- flex® nail application technique is directly derived from the long bones nailing of the lower limb.
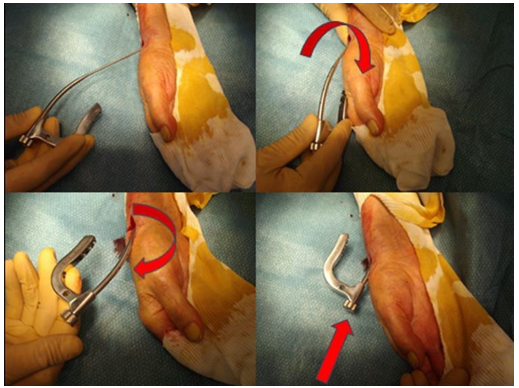
Fig n° 6: The nail is introduced in reversed position. It is turned 180° as long as pushed forwards. A “clic” is heart by the time the fracture is reduced.
The radius fracture is reduced by a classical manual traction. After “reopening” the fracture side (distraction), the nail is inserted at the level of the snuffbox, outside the tendinous areas. This nail is introduced trough the radial styloid process in the inverted position because the first curvature in the right direction by that time. Then, when the nail has been gently pushed by hand over 5 cm, it is turned 180 ° over so that the other curvature is easily introduced. The nail having an "S" position it offers a self-stability inside the radius diaphysis (3 points). But it is also elastic since the 2/3 of the nail are fine as a simple pin and automatically realigns the distal epiphysis and keeps the focus “open”. It must be locked at its distal part, with at least two epiphyseal screws.

Fig 7: Radiological aspect of the reduction and nailing of the distal radius using a strict percutaneous approach.
4) Method:
Between May 2008 and May 2015, the Nail-o-flex® nail was used to treat fractures of the lower end of the radius. The cases presented in this series have been operated by a single operator. These are fractures according to Colle or Smith. We excluded fractures of the anterior or posterior margins that were treated by another method.
Of these 105 cases, the female/male ratio was 7 to 1. The average age was 79 years, ranging from 18 to 92 years. Average operating time was 45 minutes. The hospital stay was 2 days up to 2013. After that period, all the fractures were treated as outpatients. A POP volar splint was used for one week. Than a Velcro splint has been routinely used for an extra period of 5 weeks. All the clinical results were analyzed using the Constant score which resulted in : 75 excellent, 22 satisfactory and 8 poor result. This shows an excellent functional score in 71,4% .
There was no redo for insufficient result. Fractures have been classified according to Laulan and Bismuth (7)
The purpose of this Clinical Series was to confirm that metaphyseal bone defect could be treated with an elastic nail according to the principle of Desmanet (17) , without graft or surrogate, and that the distal epiphyseal lock was sufficient to keep the epiphyseal fragments in a good position during the entire consolidation period. In this series, we have shown that 98/105 cases had retained a radio-ulnar index less than or equal to 0. This shows a good restoration of the length of the radius. Those cases are now improved with experience. In cases of a severe bone defect (E3 or E4), it is recommended to add a dorsal intra-focal pin according to fig. n° 12.
5) Discussion :
The nailing of the fractures of the radius is an outsider, because It exist so far a kind of unanimity about the anterior screwed plates (4). This recalls the 1970’s period and the struggle between the defenders of the screw / plates technic and the promoters of the nail according to Kuntscher and Danis principles, regarding femur or tibia fractures. One can criticize plates to be inserted openly on palmar side opposite to the damaged area (dorsal). This can be the a source of secondary displacement although locked mini-screws. However many mini-nails of the radius have been compromised by unreliability and limited indications. None of them had incorporated the need for an elastic recall force to oppose the natural compaction of the chamber. This is the originality of the nail-o-flex® nail.
The "nail-o-flex" nail combines a long elastic portion that takes an "S" shape in the diaphysis of the radius and a short rigid portion at the distal diaphysis. The elastic portion takes advantage of Desmanet's elastic nailing (17) and the rigid distal portion allows locking such as Kempf nails (9).
1) The compaction chamber:
The first question in the distal radius fractures seems to compensate the loss of bone matter in the metaphyseal region due to the flattening of the spongy bone. This challenge can be reached using the same technic than 1938 Danis and Küntscher nails. The clinical series has shown that the radius only recoils in 7% of cases (7/105), when this complication was usual with the Kapandji type entanglements. Efficiency seems to be due to the fact that the nail acts as a central guardian, without shear stress.
2)The reduction must be stable.
And secondarily, to maintain a quality epiphyseal reduction is relevant. The use of palmar plates may seem paradoxical since the bone comminution is mainly on the opposite side (8,9,10). The operator does not have access to it. Even self-stable screws cannot replace a missing bone. Many authors question themselves about this method which is widely diffused ( 10,11,12). The intramedullary percutaneous nail is mechanically more logical (17). It is central, thus more neutral and simple to use. Lateral approach is direct and offers more security.
3) Maintain an accurate reduction:
To maintain a good orientation of the radial epiphysis: The functional result is good if the epiphyseal length is restored. Restoring a normal prono- supination requires that the radius regain its length. The centro-medullary nail is the most stable way into an osteoporotic bone. It can be tolerated that the epiphyseal anteversion is not 15 ° but only up to 0 ° we found that this has little influence on the function.
The examination of the initial XR is important. If the fracture is classified E3 or E4 , this means the epiphysis is fractured more than 2 fragments. In that case a supplementary wire is required to create a medio-dorsal stable point. The position of this wire must be out of the extensor tendon’s compartment 4 (fig. n° 12). This wire is usually removed after 2 months.
4) Pain control:
The pain assessment is necessary. It is recognized that closed osteosynthesis are less painful than open procedures as screwed plates. (9 )
5) Esthetic aspect

Fig 8: Operative aspect: 4 sutures for a complete osteosynthesis
The aesthetic aspect is interesting. The intervention is conducted by 3 or 4 holes of 2 or 3 mm

Fig. n° 9 : case n° 85. This is not a E1 (AP view) grade but a E3 (lateral view)! A secondary dorsal displacement occurred due to misunderstanding of this fracture. This grade E3 should have necessitated a complementary dorsal pinning. Although accurate DRU joint reduction (on AP view) is present. It resulted the normal prono-supination was normal, but the palmar flexion was reduced.

Fig. n° 10: Grade M4 E4 C1 distal radius fracture with 50° dorsal displacement. It was treated with a combined nail-o-flex nail and dorso- lateral pin. The XR and functional result is excellent. Functional result is excellent.

Fig. n° 11: the additional pin must be placed out of the extensor tendons, close to the ulna, between compartment 4 & 5, with an oblique direction
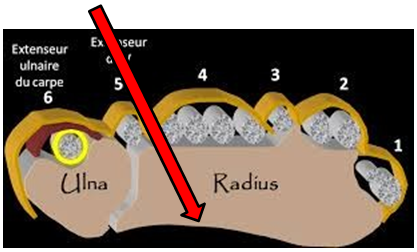
Fig. n° 12: Dorsal aspect of the wrist. The red arrow indicates the position of the dorsal complementary pin in the case of grade E3 or E4 fracture.

Fig. n° 13: a 92 years old male patient with a M4 E1 C1 ** fracture. One year post-op result
6) Conclusion:
Closed surgical treatment of fractures of the distal radius is possible. It requires a stable nail (3 points) and an effective locking system. It alsorequires careful analysis of the fracture. The “Nail-o-flex®” nail was designed in 2005. Its objective was to offer immediate stability and to restore the entire length of the radius in order to obtain a functional radio-ulnar joint. With 15 years of success, it is possible to affirm that the nailing is a simple, reliable and inexpensive osteosynthesis. Its use is easy for any surgeon familiar with the nailing of tibia or femur. It is really a miniature "Kempf" nail. Its reliability is comparable to that of the best series of palm plates, requiring only moderate X-ray irradiation (13, 14, 15, 16).
Clinical series :
Laulan & Bismuth class DRU anteversion functional result
|
1. M4 E1 C1 |
- 1mm |
0 |
excellent |
|
2. M4 E3 C1 |
- 2 |
-10 |
good |
|
3. M4 E4 C2 |
0 |
-5 |
good |
|
4. M4 E2 C1 |
0 |
5 |
excellent |
|
5. M4 E3 C2 |
0 |
5 |
excellent |
|
6. M4 E3 C1 |
0 |
0 |
excellent |
|
7. M4 E1 C1 |
-2 |
10 |
excellent |
|
8. M4 E4 C2 |
-2 |
-5 |
good |
|
9. M4 E3 C2 |
0 |
-12 |
poor |
|
10. M4 E3 C1 |
-2 |
10 |
excellent |
|
11. M4 E3 C1 |
-2 |
10 |
excellent |
|
12. M4 E4 C1 |
0 |
-15 |
poor |
|
13. M4 E3 C2 |
-2 |
5 |
excellent |
|
14. M4 E1 C1 |
0 |
0 |
excellent |
|
15. M4 E3 C1 |
-2 |
10 |
good |
|
16. M4 E2 C3 |
0 |
10 |
excellent |
|
17. M4 E4 C2 |
2 |
-5 |
excellent. |
|
18. M4 E4 C2 |
0 |
-5 |
good |
|
19. M4 E3 C2 |
0 |
-10 |
good |
|
20. M4 E4 C3 |
0 |
10 |
excellent |
|
21. M4 E3 C1 |
2 |
0 |
excellent. |
|
22. M4 E3 C3 |
0 |
5 |
excellent |
|
23. M4 E1 C1 |
2 |
-15 |
poor |
|
24. M4 E2 C1 |
- 2 |
0 |
excellent |
|
25. M4 E3 C1 |
0 |
0 |
excellent |
|
26. M4 E1 C1 |
0 |
0 |
excellent |
|
27. M4 E3 C2 |
0 |
0 |
good |
|
28. M4 E1 C1 |
0 |
10 |
excellent |
|
29. M4 E3 C2 |
- 2 |
0 |
excellent |
|
30. M4 E3 C1 |
0 |
0 |
excellent |
|
31. M4 E4 C2 |
-2 |
10 |
excellent |
|
32. M4 E4 C2 |
0 |
0 |
good |
|
33. M4 E3 C2 |
- 3 |
10 |
excellent |
|
34. M4 E3 C2 |
0 |
0 |
excellent |
|
35. M4 E3 C1 |
0 |
0 |
excellent |
|
36. M4 E2 C2 |
- 2 |
0 |
good |
|
37. M4 E1 C2 |
0 |
- 10 |
poor |
|
38. M4 E4 C3 |
0 |
0 |
excellent |
|
39. M4 E1 C2 |
0 |
0 |
good |
|
40. M4 E1 C2 |
0 |
- 15 |
poor |
|
41. M4 E4 C2 |
- 2 |
0 |
excellent |
|
42. M4 E3 C3 |
0 |
0 |
good |
|
43. M4 E4 C1 |
- 2 |
10 |
excellent |
|
44. M4 E3 C2 |
- 2 |
0 |
excellent |
|
45. M4 E3 C1 |
Smith 0 |
0 |
excellent |
|
46. M4 E2 C2 |
-2 |
0 |
excellent |
|
47. M4 E2 C1 |
-2 |
- 10 |
good |
|
48. M4 E3 C1 |
2 |
- 10 |
poor |
|
49. M4 E3 C2 |
0 |
5 |
excellent |
|
50. M4 E2 C1 |
- 2 |
10 |
excellent |
|
51. M3 E4 C1 |
Smith 0 |
15 |
excellent |
|
52. M4 E4 C1 |
- 2 |
10 |
good |
|
53. M4 E3 C1 |
0 |
0 |
excellent |
|
54. M4 E2 C2 |
- 2 |
5 |
excellent |
|
55. M4 E4 C1 |
- 2 |
0 |
excellent |
|
56. M4 E2 C1 |
0 |
0 |
good |
|
57. M4 E3 C1 |
- 2 |
5 |
excellent |
|
58. M4 E1 C1 |
0 |
0 |
good |
|
59. M4 E1 C2 |
2 |
0 |
excellent. |
|
60. M4 E3 C1 |
- 2 |
5 |
excellent |
|
61. M4 E3 C2 |
0 |
0 |
excellent |
|
62. M4 E3 C1 |
- 2 |
10 |
excellent |
|
63. M4 E4 C2 |
0 |
5 |
good |
|
64. M4 E3 C1 |
- 2 |
10 |
excellent |
|
65. M4 E2 C1 |
- 2 |
0 |
excellent |
|
66. M4 E3 C1 |
- 2 |
0 |
excellent |
|
67. M4 E4 C3 |
2 |
- 10 |
poor |
|
68. M4 E3 C1 |
- 2 |
0 |
good |
|
69. M4 E1 C1. |
-2. |
0. |
excellent |
|
70. M4 E4 C2 |
- 2 |
5 |
excellent |
|
71. M4 E4 C2 |
- 2 |
5 |
excellent |
|
72. M4 E3 C3 |
0 |
0 |
good |
|
73. M4 E3 C1 |
- 2 |
5 |
excellent |
|
74. M4 E3 C1 |
0 |
0 |
excellent |
|
75. M4 E3 C2 |
0 |
0 |
good |
|
76. M4 E3 C1 |
0 |
5 |
good |
|
77. M4 E3 C2 |
- 2 |
5 |
excellent |
|
78. M4 E1 C3 |
0 |
0 |
excellent |
|
79. M4 E1 C2 |
0 |
10 |
excellent |
|
80. M4 E3 C1 |
- 1 |
10 |
excellent |
|
81. M4 E3 C1 |
3 |
- 10 |
poor |
|
82. M4 E3 C1 |
- 1 |
10 |
excellent |
|
83. M4 E3 C1 |
- 2 |
5 |
excellent |
|
84. M4 E2 C1 |
- 1 |
5 |
excellent |
|
85. M4 E3 C2 |
0 |
- 15 |
good * |
|
86. M4 E1 C1 |
- 2 |
15 |
excellent |
|
87. M4 E1 C1 |
- 2 |
10 |
excellent |
|
88. M4 E1 C1 |
- 1 |
15 |
excellent |
|
89. M4 E1 C1 |
-2 |
0 |
excellent ** |
|
90. M4 E4 C1 |
0 |
0 |
excellent |
|
91. M4 E4 C1 |
0 |
0 |
excellent |
|
92. M4 E4 C1 |
0 |
-5 |
excellent |
|
93. M4 E3 C1 |
-2 |
10 |
excellent |
|
94. M4 E3 C1 |
-2 |
10 |
excellent |
|
95. M3 E3 C2 |
-2 |
15 |
excellent |
|
96. M4 E2 C1 |
-2 |
15 |
excellent |
|
97. M4 E1 C3 |
-2 |
15 |
excellent |
|
98. M4 E4 C1 |
0 |
0 |
excellent |
|
99. M4 E1 C1 |
-2 |
5 |
excellent |
|
100. M4 E2 C3 |
-1 |
10 |
excellent |
|
101. M4 E1 C3 |
-2 |
15 |
excellent |
|
102. M4 E4 C1 |
0 |
0 |
excellent |
|
103. M4 E4 C1 |
-1 |
5 |
excellent |
|
104. M4 E1 C1 |
-2 |
10 |
excellent |
|
105. M4 E3 C1 |
-2 |
5 |
excellent |
|
1. M4 E1 C1 |
- 1mm |
0 |
excellent |
|
2. M4 E3 C1 |
- 2 |
-10 |
good |
|
3. M4 E4 C2 |
0 |
-5 |
good |
|
4. M4 E2 C1 |
0 |
5 |
excellent |
|
5. M4 E3 C2 |
0 |
5 |
excellent |
|
6. M4 E3 C1 |
0 |
0 |
excellent |
|
7. M4 E1 C1 |
-2 |
10 |
excellent |
|
8. M4 E4 C2 |
-2 |
-5 |
good |
|
9. M4 E3 C2 |
0 |
-12 |
poor |
|
10. M4 E3 C1 |
-2 |
10 |
excellent |
|
11. M4 E3 C1 |
-2 |
10 |
excellent |
|
12. M4 E4 C1 |
0 |
-15 |
poor |
|
13. M4 E3 C2 |
-2 |
5 |
excellent |
|
14. M4 E1 C1 |
0 |
0 |
excellent |
|
15. M4 E3 C1 |
-2 |
10 |
good |
|
16. M4 E2 C3 |
0 |
10 |
excellent |
|
17. M4 E4 C2 |
2 |
-5 |
excellent. |
|
18. M4 E4 C2 |
0 |
-5 |
good |
|
19. M4 E3 C2 |
0 |
-10 |
good |
|
20. M4 E4 C3 |
0 |
10 |
excellent |
|
21. M4 E3 C1 |
2 |
0 |
excellent. |
|
22. M4 E3 C3 |
0 |
5 |
excellent |
|
23. M4 E1 C1 |
2 |
-15 |
poor |
|
24. M4 E2 C1 |
- 2 |
0 |
excellent |
|
25. M4 E3 C1 |
0 |
0 |
excellent |
|
26. M4 E1 C1 |
0 |
0 |
excellent |
|
27. M4 E3 C2 |
0 |
0 |
good |
|
28. M4 E1 C1 |
0 |
10 |
excellent |
|
29. M4 E3 C2 |
- 2 |
0 |
excellent |
|
30. M4 E3 C1 |
0 |
0 |
excellent |
|
31. M4 E4 C2 |
-2 |
10 |
excellent |
|
32. M4 E4 C2 |
0 |
0 |
good |
|
33. M4 E3 C2 |
- 3 |
10 |
excellent |
|
34. M4 E3 C2 |
0 |
0 |
excellent |
|
35. M4 E3 C1 |
0 |
0 |
excellent |
|
36. M4 E2 C2 |
- 2 |
0 |
good |
|
37. M4 E1 C2 |
0 |
- 10 |
poor |
|
38. M4 E4 C3 |
0 |
0 |
excellent |
|
39. M4 E1 C2 |
0 |
0 |
good |
|
40. M4 E1 C2 |
0 |
- 15 |
poor |
|
41. M4 E4 C2 |
- 2 |
0 |
excellent |
|
42. M4 E3 C3 |
0 |
0 |
good |
|
43. M4 E4 C1 |
- 2 |
10 |
excellent |
|
44. M4 E3 C2 |
- 2 |
0 |
excellent |
|
45. M4 E3 C1 |
Smith 0 |
0 |
excellent |
|
46. M4 E2 C2 |
-2 |
0 |
excellent |
|
47. M4 E2 C1 |
-2 |
- 10 |
good |
|
48. M4 E3 C1 |
2 |
- 10 |
poor |
|
49. M4 E3 C2 |
0 |
5 |
excellent |
|
50. M4 E2 C1 |
- 2 |
10 |
excellent |
|
51. M3 E4 C1 |
Smith 0 |
15 |
excellent |
|
52. M4 E4 C1 |
- 2 |
10 |
good |
|
53. M4 E3 C1 |
0 |
0 |
excellent |
|
54. M4 E2 C2 |
- 2 |
5 |
excellent |
|
55. M4 E4 C1 |
- 2 |
0 |
excellent |
|
56. M4 E2 C1 |
0 |
0 |
good |
|
57. M4 E3 C1 |
- 2 |
5 |
excellent |
|
58. M4 E1 C1 |
0 |
0 |
good |
|
59. M4 E1 C2 |
2 |
0 |
excellent. |
|
60. M4 E3 C1 |
- 2 |
5 |
excellent |
|
61. M4 E3 C2 |
0 |
0 |
excellent |
|
62. M4 E3 C1 |
- 2 |
10 |
excellent |
|
63. M4 E4 C2 |
0 |
5 |
good |
|
64. M4 E3 C1 |
- 2 |
10 |
excellent |
|
65. M4 E2 C1 |
- 2 |
0 |
excellent |
|
66. M4 E3 C1 |
- 2 |
0 |
excellent |
|
67. M4 E4 C3 |
2 |
- 10 |
poor |
|
68. M4 E3 C1 |
- 2 |
0 |
good |
|
69. M4 E1 C1. |
-2. |
0. |
excellent |
|
70. M4 E4 C2 |
- 2 |
5 |
excellent |
|
71. M4 E4 C2 |
- 2 |
5 |
excellent |
|
72. M4 E3 C3 |
0 |
0 |
good |
|
73. M4 E3 C1 |
- 2 |
5 |
excellent |
|
74. M4 E3 C1 |
0 |
0 |
excellent |
|
75. M4 E3 C2 |
0 |
0 |
good |
|
76. M4 E3 C1 |
0 |
5 |
good |
|
77. M4 E3 C2 |
- 2 |
5 |
excellent |
|
78. M4 E1 C3 |
0 |
0 |
excellent |
|
79. M4 E1 C2 |
0 |
10 |
excellent |
|
80. M4 E3 C1 |
- 1 |
10 |
excellent |
|
81. M4 E3 C1 |
3 |
- 10 |
poor |
|
82. M4 E3 C1 |
- 1 |
10 |
excellent |
|
83. M4 E3 C1 |
- 2 |
5 |
excellent |
|
84. M4 E2 C1 |
- 1 |
5 |
excellent |
|
85. M4 E3 C2 |
0 |
- 15 |
good * |
|
86. M4 E1 C1 |
- 2 |
15 |
excellent |
|
87. M4 E1 C1 |
- 2 |
10 |
excellent |
|
88. M4 E1 C1 |
- 1 |
15 |
excellent |
|
89. M4 E1 C1 |
-2 |
0 |
excellent ** |
|
90. M4 E4 C1 |
0 |
0 |
excellent |
|
91. M4 E4 C1 |
0 |
0 |
excellent |
|
92. M4 E4 C1 |
0 |
-5 |
excellent |
|
93. M4 E3 C1 |
-2 |
10 |
excellent |
|
94. M4 E3 C1 |
-2 |
10 |
excellent |
|
95. M3 E3 C2 |
-2 |
15 |
excellent |
|
96. M4 E2 C1 |
-2 |
15 |
excellent |
|
97. M4 E1 C3 |
-2 |
15 |
excellent |
|
98. M4 E4 C1 |
0 |
0 |
excellent |
|
99. M4 E1 C1 |
-2 |
5 |
excellent |
|
100. M4 E2 C3 |
-1 |
10 |
excellent |
|
101. M4 E1 C3 |
-2 |
15 |
excellent |
|
102. M4 E4 C1 |
0 |
0 |
excellent |
|
103. M4 E4 C1 |
-1 |
5 |
excellent |
|
104. M4 E1 C1 |
-2 |
10 |
excellent |
|
105. M4 E3 C1 |
-2 |
5 |
excellent |
functional results : Excellent = 75 good = 22 poor = 8 *Figure n° 10 ** fig. n° 13
Table n°1 : clinical series: A continuous series of 105 cases of distal radius fractures treated with percutaneous nailing “Nail-o-flex®”.

Fig n°9: Laulan and Bismuth classification of distal radius fractures.