Clinical Case Reports and Clinical Study
OPEN ACCESS | Volume 13 - Issue 1 - 2026
ISSN No: 2766-8614 | Journal DOI: 10.61148/2766-8614/JCCRCS
Oleksandr Yu. Ioffe1, Oleksandr P. Stetsenko1, Yurii P. Tsiura1, Stepan. L. Kindzer1, Mykola S. Kryvopustov1 and Yevgeniy S. Prykhodko2*
1Bogomolets National Medical University, Kyiv
2Kyiv City Clinical Hospital.
*Corresponding author: Yevgeniy S. Prykhodko, Kyiv City Clinical Hospital.
Received: February 26, 2024
Accepted: April 30, 2024
Published: July 29, 2024
Citation: Oleksandr Yu. Ioffe, Oleksandr P. Stetsenko, Yurii P. Tsiura, Stepan. L. Kindzer, and Yevgeniy S. Prykhodko.et.al. (2024) “A Clinical Case of Surgical Treatment of Appendiceal Stump Abscess.”, Clinical Case Reports and Clinical Study, 11(1); DOI: 10.61148/2766- 8614/JCCRCS/169
Copyright: © 2024 Yevgeniy S. Prykhodko. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
A 25-year-old male patient presented to the Department of Purulent Surgery (DPS) complaining of a "small wound" at the site of the postoperative scar in the right inguinal area and minor purulent discharge from it. The patient underwent surgery for acute phlegmonous appendicitis four months ago, in July. On November 1, after physical exertion, the wound appeared again, and on November 3, the patient independently sought consultation with the DPS at Kyiv City Clinical Hospital No. 3, was examined by a surgeon, and was hospitalized. The wound revision showed a tumor-like formation measuring 2.5 x 3.0 x 2.5 cm, and the parietal peritoneum was revealed too. The appendectomy was performed by the purse-string ligation method with drainage of the abdominal cavity through a separate contraperture with polyvinyl chloride tube drainage. After the operation, a diagnosis was made: abscess of the appendiceal stump, and external fistula of the anterior abdominal wall. The postoperative wound healed with primary tension and the stitches were removed.
Introduction:
In Ukraine, acute appendicitis (АР) accounts for 89.1% of the total number of patients with acute surgical pathology. In modern surgical practice, early and late complications take the first place in the structure of acute surgical diseases of the abdominal cavity, regardless of the age and gender of the patients, and the postoperative mortality rate is 0.15% on average [1, 2]. In the long run, following an appendectomy, despite the advancements in modern surgery, a very rare complication known as inflammation of the appendiceal stump might occur; few surgeons have ever encountered this in their practice. Even at the dawn of surgical treatment for acute appendicitis, surgeons of that time wrote about this pathology in their works 48 clinical cases of this pathology have been reported in the contemporary medical research literature [3,4,5,6].
Postoperative complications present a challenge in abdominal surgery as they interfere with predicting the course and the surgical treatment of abdominal emergencies. According to O. S. Balogun et al. (2019) [7], their number is 28.5%, with such complications as suppuration of the surgical wound in 18.6%, wound dehiscence in 15.2%, and intra-abdominal abscess in 13.5% of patients.
Description of a Clinical Case:
A 25 y.o. male patient presented to the Department of Purulent Surgery (DPS) complaining of a "small wound" at the site of the postoperative scar in the right inguinal area and minor purulent discharge from it.
According to the anamnesis, he underwent surgery for acute phlegmonous appendicitis four months ago. The early p.o. period was uneventful. On the fifth day, he was discharged in satisfactory condition. The postoperative wound healed with primary tension, and the sutures were removed on the seventh day. The patient reported that two months after the surgical treatment, a "small wound" "opened" for no apparent reason at the site of the postoperative scar, and there was also minor purulent discharge from it. That was the cause of his appointment with the surgeon at the polyclinic. The ligature was removed during a wound revision procedure conducted. A ligature fistula at the site of the postoperative scar was diagnosed. The application of dressings, drainage of the wound with an antiseptic Decametoxinum, and oral administration of Lefloxacin 500 mg promoted wound healing by secondary tension. On November 1, after physical exertion (playing football), the wound appeared again, and on November 3, the patient independently sought consultation with the DPS at Kyiv City Clinical Hospital No. 3, was examined by a surgeon, and was hospitalized.
On examination, from the side of the digestive organs without no pathology. Auscultation and percussion are unchanged. A digital rectal examination shows no pathology.
The right inguinal area has a p.o. scar without signs of perifocal inflammation. In the lower third, there is a fistula tract up to 0.1 cm with minor purulent discharge. Hyperaemia of the skin and edema, pain syndrome during palpation is absent, and symptoms of peritoneal irritation are negative. A ligature fistula at the site of the postoperative scar is initially diagnosed.
To prepare for the surgical procedure, the patient underwent clinical and laboratory examinations. CDC on November 3: HB - 148 g/l, glucose - 5.2 mmol/l, leukocytes - 6,7*109/l, rod cells - 4%, segment cells - 70%, eosinophils - 1%, lymphocytes – 24%, monocytes – 1%.
According to the ultrasound of the abdominal cavity, in the right iliac region, in the projection of the postoperative scar at a depth of up to 3.5 cm, a hyperechoic formation measuring 1×1.5 cm with clear contours is visualized. Free fluid is not detected. X-ray of the organs of the abdominal cavity with identification of the fistula tract with sodium amidotrizoate contrast: free gas and Kloiber’s cups are not detected; an accumulation of contrast in the form of a "mace" is noted, with a high probability in the abdominal cavity in the right iliac fossa (figure 1).
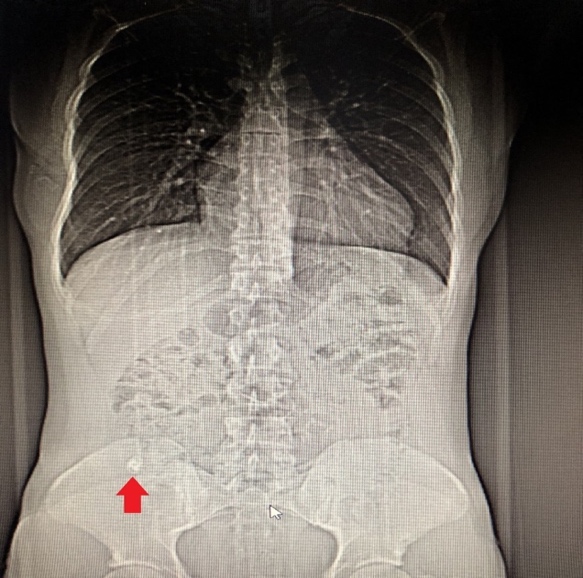
Figure 1: X-ray of the abdominal organs with fistula contrast with sodium
Based on the instrumental research methods results, the patient was prescribed a CT scan with contrast enhancement to confirm or exclude the localization of the pathological process in the abdominal cavity and to determine the extent of the surgical treatment (figure 2).
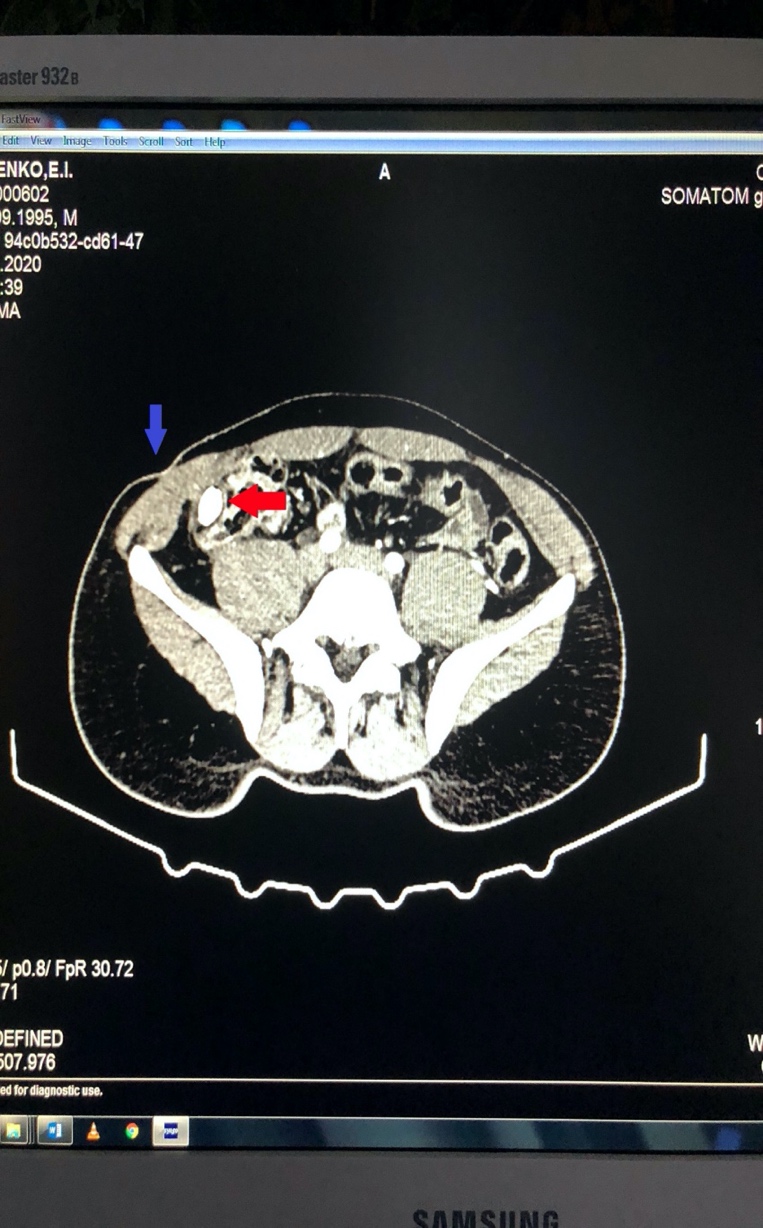
Figure 2: CT of the organs of the abdominal cavity with contrast enhancement.
The blue arrow in the figure indicates the skin defect and the external opening of the fistula. The red arrow in the figure indicates the accumulation of contrast in the right iliac fossa, and based on the radiologist's conclusion, a diagnosis of abdominal abscess was established.
On November 4, the patient underwent surgical treatment following diagnostic procedures. After treatment of the operative field, the postoperative scar was excised together with the fistula tract to the aponeurosis. The abdominal cavity was opened in layers. The wound revision showed a tumor-like formation measuring 2.5x3.0x2.5 cm with even margins of a dense consistency fused with the dome of the cecum, and the parietal peritoneum was revealed too. As a result of the separation of the formation up to 3.5-4.0 cm the appendiceal stump, which was located subserosally in the wall of the cecum, was found (figure 3).
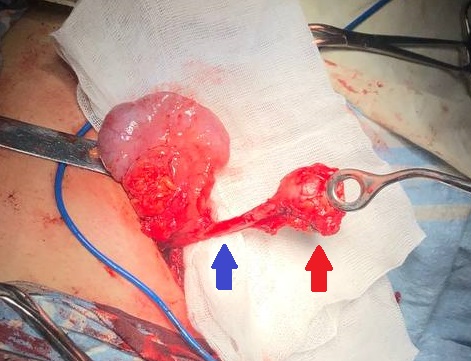
Figure 3: Immobilized "long" appendiceal stump. The red arrow indicates the stump abscess and the blue arrow indicates the stump itself.
Removal of the appendiceal stump was performed by the purse-string ligation method with drainage of the abdominal cavity through a separate contraperture with polyvinyl chloride tube drainage.
After the surgery, a diagnosis was determined: abscess of the appendiceal stump, and external fistula of the anterior abdominal wall.
Therapy was prescribed in the postoperative period for 3 days: Moxifloxacin 400 mg intravenously once a day; Enoxaparin sodium 0.3 subcutaneously once a day; Pantoprazole 40 mg intravenously once a day; and Dexketoprofen 50 mg IV 3 times a day. The drain was removed on the second day.
Treatment outcomes:
The patient was discharged for outpatient treatment on the fifth day after the operation. On the eighth day, he was examined in the hospital; the postoperative wound healed with primary tension, and the stitches were removed. The patient had follow-up exams at 6 and 12 months post-surgery, including an abdominal cavity ultrasound (no pathology).
Conclusions: