Case Reports International Journal
OPEN ACCESS | Volume 3 - Issue 2 - 2025
ISSN No: 3065-6710 | Journal DOI: 10.61148/ 3065-6710/CRIJ
Dos Santos Souza Daniela C1*, Mussato, Diego H.F2, Oliveira, Leticia S3
1São Paulo State University (Unesp), School of Medicine, Department of Pathology,
Av Prof Mario R Guimaraes Montenegro s/n, 18618-687. Botucatu, SP, Brazil.
2São Paulo State University (Unesp), School of Medicine, Department of Pathology, Botucatu, SP, Brazil.
3São Paulo State University (Unesp), School of Medicine, Department of Pathology, Botucatu, SP, Brazil.
*Corresponding author: Daniela Cristina Dos Santos Souza, MD, PhD, Department of Pathology, São Paulo State University (Unesp), School of Medicine, Botucatu, SP, Brazil, Avenida Prof. Mário Rubens Guimarães Montenegro s/n, Botucatu-18618-687, SP-Brazil.
Received: August 20, 2025 | Accepted: September 10, 2025 | Published: September 25, 2025
Citation: Dos Santos Souza Daniela C, Mussato, Diego H.F, Oliveira, Leticia S., (2025) “Study of Histopathological Patterns of Pulmonary Infections in Autopsies at Death Verification Service: Association with Risk Factors and Comorbidities” Case Reports International Journal, 3(2); DOI: 10.61148/3065-6710/CRIJ/030.
Copyright: © 2025 Daniela Cristina Dos Santos Souza. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Our study aimed to analyze the morphological patterns of lung infection types in autopsy cases and to establish associations between clinical conditions, comorbidities, and risk factors present in patients at the time of death. Clinical and laboratory data were also obtained. A total of 165 autopsy reports of patients who died from pneumonia between 2010 and 2023 were analyzed. Autopsy samples of lung infections were examined under an optical microscope, and pulmonary findings such as: tracheitis, pulmonary edema and congestion, diffuse alveolar damage, cavitation, alveolitis, perialveolar capillaritis, interstitial xanthomatous cells, intra-alveolar xanthomatous cells, emphysema, interstitial fibrosis, and alveolar bronchiolization, were observed. Histological findings were represented as categorical variables. Bivariate associations were estimated using simple linear regression with a Poisson response for binary outcomes, or normal regression for numeric outcomes. Pulmonary anthracosis, alveolar xanthomatous macrophages, alveolar emphysema, interstitial xanthomatous macrophages, pulmonary edema and congestion, tracheitis, and bronchitis were the significant histological findings in this study. These were significantly associated with pneumonia in patients who presented with senility, diabetes, obesity, and chronic obstructive pulmonary disease. This broad study of autopsy lung samples revealed interesting associations with comorbidities, reinforcing the need to closely monitor the evolution of pneumonia in these epidemiological groups.
Lung; Pneumonia; Autopsy; Risk factors
Lower respiratory tract infections are one of the leading causes of mortality worldwide. Among these, one of the most prominent is pneumonia, a term used to define any lung infection.[3] The clinical presentation may be acute, characterized by symptoms such as fever, cough, shortness of breath, and a decline in general health, or chronic, with a more prolonged course.[4]
Thus, the present study aimed to analyze the morphological patterns of types of lung infections in autopsy cases within the death verification service (DVS) and establish associations between clinical conditions, comorbidities, and risk factors that patients presented with at the time of death.
Material and Methods
Cases were included in the study when autopsies revealed evidence of lung infections in the necroscopic examination. The clinical and laboratory results were evaluated using autopsy records. All histological slides of necroscopic cases selected for material suitability were reviewed.
Data regarding age, sex, clinical course (diabetes, hypertension, dyslipidemia, obesity, smoking, alcoholism, cachexia, allergies, autoimmune diseases, and other lung pathologies, such as pulmonary fibrosis, chronic obstructive pulmonary disease (COPD), clinical history of immobility/bed restriction, hospitalization, institutionalization, oncological history, previous surgeries, immunodeficiencies, and vaccination).
Autopsy samples of lung infections were examined under an optical microscope, and pulmonary findings are described in Table 1. The collected data were separated into categorical variables by epidemiological profiles and histopathological patterns found in the microscopic analyses of the sample.
Statistical analyses were performed using Statistical Package for Social Sciences (SPSS) version 21 (IBM Corp., Armonk, NY, USA). Qualitative data are presented as frequencies and percentages. Independent t-tests were performed to compare continuous variables between groups, and the results are presented as measures of central tendency (average ± standard deviation and median). The Chi-square test was used to compare categorical variables. Statistical significance was defined as P< 0.05. Histological findings were represented as categorical variables, and bivariate associations were estimated using simple linear regressions with Poisson responses for outcomes and binary or normal responses for numeric outcomes. The variables that presented an association with p < 0.20 were taken to adjust a multiple regression with Poisson or normal response. Statistical significance was defined as P < 0.05.
The study was reviewed and approved by the ethics committee (CAAE:71548923.2.0000.5411).
Results
A total of 165 autopsy reports of patients who died of pneumonia between 2010 and 2023 were analyzed.
Regarding the epidemiological information on the number of autopsy cases studied, we extracted the following profile extracted from the necropsy reports (data from deceased patients): male patients 61.81%, female patients 38.18 %, white ethnicity 36.70%, brown ethnicity 7.78%, black ethnicity 2.22%, ethnicity not reported in the reports 53.3%, occupational exposure in 2.22% with an average age of 60.5 years, smoking in 20% of cases with an average age of 61.38 years, alcoholism in 23.33% of cases with an average age of 52.19 years.
Presence of comorbidities such as diabetes mellitus in 14.44% of cases, with a mean age of 61.38 years, systemic arterial hypertension 35.56% with a mean age of 66.65 years, dyslipidemia in 6.67% of cases with a mean age of 73.33 years, obesity in 8.89% of cases with a mean age of 50.12 years.
Non-pulmonary neoplasms were identified in 15.56% of cases with a mean age of 68.28 years, cachexia in 24.44% of cases with a mean age of 52.64 years, immunodeficiencies not related to the HIV were observed in 5.56% of cases with a mean age of 43.80 years, autoimmune diseases observed in 4.44% of cases with a mean age of 42.75 years, patients seropositive for human immunodeficiency virus in 7.78% of cases with a mean age of 42.71 years.
Patients with pneumonia who also had diseases at a primary pulmonary site: presence of chronic obstructive pulmonary disease (COPD) in 8.89% of cases with a mean age of 69.50 years, idiopathic pulmonary fibrosis in 1.11% with a mean age of 94.0 years, pulmonary hypertension in 12.22% of cases with a mean age of 56.97 years, and some type of lung carcinoma in 5.56% of cases with a mean age of 61.40 years.
Patients who were selected for this case series and still presented complications such as: acute kidney injury in 14.44% of cases with a mean age of 33.14 years, chronic kidney disease in 3.33% of cases with a mean age of 77.66 years, acute respiratory distress syndrome in 5.56% of cases with a mean age of 44.00 years, pulmonary thromboembolism in 10.00% of cases with a mean age of 63.77 years, sepsis in 41.11% of cases with a mean age of 42.49 years, use of supplemental oxygen in 7.78% of cases with a mean age of 57.57 years and with care in an intensive care unit (ICU) in 20.00% of cases with a mean age of 32.37 years.
Patients who were confined to bed in the postoperative period, with a late surgical history, or institutionalized, totaled 31.11% with a mean age of 57.45 years. Prematurity was observed in 3.33% of cases, and congenital malformations in 2.22% of cases.
All histological criteria studied in the necropsy cases are listed in Table 1, with the number and percentage of cases, respectively, for the 165 autopsies studied.
Table 1: Description of the spectrum of histological changes in pulmonary infections from reviewed autopsy cases
|
Morphological criteria |
Number of cases and percentages |
|
|
Tracheitis |
8 |
4.84% |
|
Bronchitis |
51 |
30.90% |
|
Lymphocytic bronchiolitis in the lamina propria (LP) |
107 |
64.84% |
|
Luminal bronchiolitis |
45 |
27.27% |
|
Bronchiectasis |
18 |
10.90% |
|
Bronchiolectasia |
61 |
36.96% |
|
Pneumocyte hyperplasia type II |
30 |
18.18% |
|
Pneumocyte hyperplasia type I |
28 |
16.96% |
|
Cisuritis |
93 |
56.36% |
|
Alveolitis |
139 |
84.24% |
|
Perialveolar capillaritis |
158 |
95.75% |
|
Pulmonary congestion |
147 |
89.09% |
|
Pulmonary edema |
125 |
75.75% |
|
Pleural effusion |
45 |
27.27% |
|
Neutrophilic lung inflammation |
119 |
72.12% |
|
Lymphomononuclear lung inflammation |
134 |
81.12% |
|
Interstitial distribution |
152 |
92.12% |
|
Alveolar distribution |
127 |
76.96% |
|
Bronchopneumonic pattern |
121 |
73.33% |
|
Panacinar (lobar) pattern |
54 |
32.72% |
|
Condensation |
160 |
96.96% |
|
Atelectasis |
6 |
3.63% |
|
Alveolar thickening |
158 |
95.75% |
|
Granuloma |
30 |
18.18% |
|
Cavitations |
11 |
6.67% |
|
Interstitial xanthomatous cells |
69 |
41.81% |
|
Alveolar xanthomatous cells |
131 |
79.39% |
|
Abscesses |
31 |
18.78% |
|
Empyemas |
11 |
6.67% |
|
Acute suppurative pleuritis |
30 |
18.18% |
|
Fibrinous pleuritis |
33 |
20.00% |
|
Chronic pleuritis |
82 |
49.69% |
|
Pleural adhesions |
41 |
24.84% |
|
Pleural thickening |
125 |
75.75% |
|
Diffuse alveolar damage |
56 |
33.93% |
|
Fibrin in airways |
111 |
67.27% |
|
Thrombi or emboli |
46 |
27.87% |
|
Pulmonary infarction |
23 |
13.93% |
|
Scar area |
108 |
65.45% |
|
Pulmonary necrosis |
66 |
40.00% |
|
Caseous necrosis |
10 |
6.06% |
|
Pulmonary hemorrhage |
81 |
49.09% |
|
Blood in the airways |
101 |
61.21% |
|
Hemosiderin pigment |
123 |
74.54% |
|
Blisters |
104 |
63.03% |
|
Emphysema |
121 |
73.33% |
|
Anthracosis |
124 |
75.15% |
|
Interstitial fibrosis |
117 |
70.90% |
|
Alveolar fibrosis |
43 |
26.06% |
|
Local Neoplasm |
11 |
6.67% |
|
Metaplasias |
9 |
5.45% |
|
Metastasis |
7 |
4.24% |
|
Alveolar bronchiolization |
48 |
29.09% |
|
Lymphoid clusters in the lamina propria |
24 |
14.54% |
|
Mediastinal or peribronchial lymph node enlargement |
15 |
9.09% |
|
Food debris |
34 |
20.60% |
|
Fungal elements |
11 |
6.67% |
|
Viral nuclear inclusions |
8 |
4.84% |
|
Bacterial colonies |
31 |
18.78% |
|
Acid-fast bacilli (AFB) |
8 |
4.84% |
After all the clinical and morphological criteria were reviewed, the data were submitted for statistical analysis. The morphological data were grouped and named with letters in a sequential pattern, forming morphological groups.
Composition of group A: Tracheitis, bronchitis, luminal and lamina propria lymphocytic bronchiolitis, bronchiectasis, and bronchiolectasis. Results for group A: Chronic obstructive pulmonary disease (COPD) was significantly associated with an increase in the number of events (p = 0.017). Diabetes Mellitus was significantly associated with a reduction in the number of events in Group A (p = 0.031). Systemic arterial hypertension was significantly associated with a reduction in the number of events in Group A (p = 0.039).
Composition of group B: Type I and type II pneumocyte hyperplasia, alveolitis, perialveolar capillaritis, and alveolar thickening. Results for group B: Linear regression showed that smoking was significantly associated with a reduction in the number of events in group B (p = 0.009). Chronic obstructive pulmonary disease (COPD) was significantly associated with a reduction in the number of events in group B (p = 0.015).
Composition of group C: Condensation, congestion, and pulmonary edema. Results for group C: In the linear regression, male sex was significantly associated with an increase in the number of events in group C (p = 0.041). Obesity was significantly associated with an increase in the number of events in Group C (p = 0.043). Sepsis and septic shock were significantly associated with an increase in the number of events in Group C (p = 0.027).
Group D: Neutrophilic and lymphomononuclear inflammatory patterns with interstitial and alveolar distribution, interstitial and alveolar xanthomatous cells, bronchopneumonia, and lobar pneumonia. Results for group D: In linear regression analysis, chronic obstructive pulmonary disease (COPD) was significantly associated with a reduction in the number of events in group D (p = 0.017).
Group E: Atelectasis, granuloma, cavitation, abscess, pulmonary infarction, pulmonary necrosis, caseous necrosis, and scar area. Results for group E: Smoking was significantly associated with an increased number of events in group E (p = 0.035). Chronic obstructive pulmonary disease (COPD) was significantly associated with an increased number of events in group E (P= 0.007). Pulmonary hypertension was significantly associated with an increased number of events in group E (p = 0.049).
Group G included pleural effusion, empyema, acute suppurative pleuritis, fibrinous pleuritis, chronic pleuritis, pleural adhesion, pleural thickening, and cisuritis. Results for group G: In linear regression analysis, diabetes mellitus was significantly associated with an increase in the number of events in group G (p = 0.048). Acute kidney injury was significantly associated with an increase in the number of events in group G (p = 0.006).
Composition of group K: Alveolar emphysema and blisters. Results for group K: Systemic arterial hypertension was significantly associated with an increased occurrence in group K (p = 0.036).
Group L: Alveolar bronchiolization, lymphoid clusters in the lamina propria, mediastinal or peribronchial lymph node enlargement, and metaplasia. Results for group L: There were no associations between variables in linear or multiple regression for outcome group L.
Composition of group M: Lung neoplasia and metastases. Results for group M: Linear regression showed that smoking was significantly associated with an increased occurrence in group M (p = 0.001). Systemic arterial hypertension was significantly associated with an increased occurrence in group M (p = 0.040).
Composition of group N: Presence of food debris. Results for group N: In linear regression, bronchial asthma was significantly associated with an increased occurrence in group N (RP = 5.09; p = 0.026). Cachexia was significantly associated with an increased occurrence in group N (p = 0.001).
Composition of group P: anthracosis, alveolar and interstitial xanthomatous macrophages, and alveolar emphysema, as represented in Figure 1.
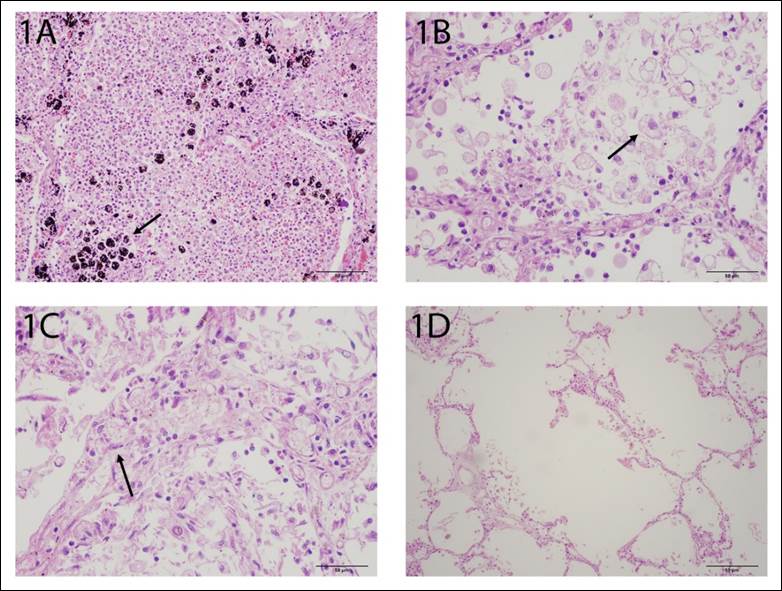
Figure 1: Histological group “P”. 1A: Pulmonary anthracosis (arrow) (H&E: 400X magnification), 1B: alveolar xanthomatous macrophages (arrow) (H&E: 400X magnification), 1C: alveolar emphx’ysema (arrow) (H&E: 400X magnification) and 1D: interstitial xanthomatous macrophages (H&E: 400X magnification).
Results for group P: In the linear regression, the 1-year difference between ages was significantly associated with an increased number of events in group P (p < 0.001) (Table 2). Male sex was significantly associated with an increased number of events in the P group (p = 0.018) (Table 2). Diabetes mellitus was significantly associated with an increase in the number of events in group P (P = 0.032) (Table 2).
Table 2: Study of frequency associations between the histopathological group “P” (pulmonary anthracosis, interstitial xanthomatous macrophages, alveolar xanthomatous macrophages and alveolar emphysema) and risk factors for Pneumonia.
|
Linear regression with normal response to explain the outcome of the number of events in group P |
|||
|
Variable |
b |
IC95% |
p* |
|
Age higher 60 y |
2.00 |
1.47 2.52 |
<0.001 |
|
Male gender |
0.31 |
0.05 0.57 |
0.018 |
|
Smoking |
-0.30 |
-0.62 0.02 |
0.070 |
|
Diabetes mellitus |
0.38 |
0.03 0.72 |
0.032 |
|
Chronic alcoholism |
0.24 |
-0.09 0.58 |
0.156 |
|
Systemic arterial hypertension |
-0.18 |
-0.46 0.11 |
0.227 |
*p was set at p< 0.05.
Composition of groups: F (blisters, interstitial and alveolar fibrosis), H (diffuse alveolar damage, fibrin in the airways, thrombi, or emboli), I (pulmonary hemorrhage and blood in the airways), J (hemosiderin pigments and anthracosis), O (bacterial colonies, viral nuclear inclusions, fungal elements, and staining for acid-fast bacilli). There were no associations between variables in the linear or multiple regression for the outcomes of these groups.
Discussion
Tracheitis, bronchitis, and dilation of the bronchi and bronchioles are more prevalent in cases of necropsies with pneumonia that also reveal chronic obstructive pulmonary disease (COPD).
Our results are in agreement with those described in the literature regarding COPD as a risk factor for pneumonia. Patients with COPD and pneumonia have a higher number of infections, especially those associated with specific bacteria, such as Pseudomonas aeruginosa, and patients with bronchiectasis are
particularly affected by pneumonia due to this etiology.[5] Based on the same observations, inflammatory infiltrates of interstitial and alveolar patterns were rarely observed in cases of deaths in patients with pneumonia and COPD.
Another interesting association was found between histopathological findings of pulmonary edema, congestion, and obesity. Pulmonary edema and congestion are notoriously related to stasis, heart failure, and changes related to coagulation in systemic inflammatory processes, such as sepsis.
Obesity can leave patients susceptible to peripheral airway collapse, atelectasis, and a corresponding decrease in lung compliance.[6] From a pathophysiological point of view, obesity is also associated with increased circulating procoagulant factors [7] and slow venous return related to increased intra-abdominal pressure.[8]
Morphological group P brings together four characteristics: pulmonary anthracosis, alveolar and interstitial xanthomatous macrophages, and alveolar emphysema. It provides relevant information regarding the profile of patients who died from pneumonia and underwent autopsy.
For example, this set demonstrated an association of frequency with the age of patients, especially those over 60 years old, who presented on average two more events (p < 0.001) compared to other age groups and represented 68 autopsies analyzed (41.2% of the sample).
This can be explained, in part, by the longer exposure time to inhalation of carbon particles present in the atmosphere of large urban centers that progressively deposit in the lung parenchyma in the form of anthracosis. The affected patients were predominantly elderly, with a mean age of 63 ± 3.8 years, significantly older than the mean age of unaffected individuals (52 ± 6.4 years). This reflects the chronic nature of environmental exposure.[9]
We observed a higher quantity of anthracose particles within macrophages and a higher number of xanthomatous macrophages in elderly individuals because soot particles are phagocytosed by macrophages, which degenerate and appear greasy on histopathology. However, this process recruits chronic inflammation to the lung, which can disrupt local immune function in patients who already have reduced lung function due to senility and who frequently live with other comorbidities, such as cardiovascular disease.[10]
Alveolar emphysema was more prevalent in the elderly; among the reasons that explain this finding, we can consider that the production and release of free radicals with oxidative potential causes damage to the structures, a process that culminates in tissue repair and fibrosis over time, which can disorganize the lung architecture and generate a pattern of alveolar emphysema with loss of elasticity of the organ and mucociliary dysfunction, which in turn facilitates the trapping of infectious agents, hinders the elimination of secretions due to obstructive factors, and reduces the efficiency of the cough mechanism.[11]
However, for group P, males presented an average of 0.31 more events (p = 0.018) compared to females, comprising 102 autopsies analyzed (61.8% of the sample) against 63 autopsies (38.2%) respectively. Thus, studies have suggested that community-acquired pneumonia is more prevalent in men than in women. Data from the 2019 Global Burden of Diseases (GBD) study indicate that lower respiratory tract infections (LRTI) caused 489 million incident cases globally, with 257 million men and 232 million women. In terms of prevalence, there were 11 million global cases, with 5.8 million in men and 5.2 million in women. [12,13]
Behavioral and exposure factors must also be considered, as men have a higher prevalence of habits that increase the risk of pneumonia, such as smoking (associated with lung damage) and excessive alcohol consumption; occupational exposure, especially in jobs that involve contact with toxic agents or pathogens; and comorbidities, as men have a higher incidence of conditions associated with pneumonia, such as Chronic Obstructive Pulmonary Disease (COPD) and type 2 Diabetes Mellitus, which increase the risk and severity of the disease.[14]
Diabetes Mellitus (DM), also in group P, presented an average of 0.38 more events (p = 0.032) compared to non-diabetics, comprising 25 autopsies analyzed (15.1% of the sample), a prevalent clinical condition in the Brazilian population. The disease of metabolic origin is accompanied by chronic inflammation with oxidative stress and tissue damage, including anthracosis in the lung , and systemic microvascular lesions with reduced perfusion and areas of ischemia, increasing structural damage and compromising function, a point in common with alveolar emphysema. Therefore, several mechanisms are involved in predisposition to infection. For example, high blood glucose levels compromise the function of neutrophils and macrophages, which are immune cells that are essential for fighting infections. [15,16]
Conclusion
Thus, in this autopsy study, we were able to show interesting associations between morphological patterns in histological slides of lung infections and comorbidities, with COPD, smoking, obesity, and diabetes mellitus being the most prominent from a statistical point of view. Our results show through morphological study that male patients aged > 60 years who present with any of these comorbidities show specific histopathological alterations.