Case Reports International Journal
OPEN ACCESS | Volume 3 - Issue 1 - 2025
ISSN No: 3065-6710 | Journal DOI: 10.61148/ 3065-6710/CRIJ
Rawan Alkhatib, MBBS1*; Joseph Bushra, MD1; Christopher L Berry, MD1
1Department of Emergency Medicine, The Guthrie Clinic.
*Corresponding author: Rawan Alkhatib, Department of Emergency Medicine, The Guthrie Clinic.
Received: June 10, 2025
Accepted: June 17, 2025
Published: June 20, 2025
Citation: Rawan Alkhatib, Joseph Bushra, Christopher L Berry. (2025) “Man with Buttock Mass Two Months After Trauma” Case Reports International Journal, 3(1); DOI: 10.61148/3065-6710/CRIJ/020.
Copyright: © 2025 Rawan Alkhatib. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
A 34-year-old male patient presents to the emergency department due to a progressively expanding mass on his left buttock (Figure 1). Two months prior to this visit, the patient had been injured in a motorcycle collision. Computed Tomography (CT) performed on the day of his initial injury showed a non-specific fluid infiltration over the left iliac crest, lower back, and buttock, without a large fluid collection, considered to be hematoma. (Figure 2). On his second visit, there was a firm and tender mass measuring approximately 21 x 18 cm with overlying erythema on the left buttock. The patient reported progressive enlargement of this mass over the prior months and sensitivity to light touch. Vital signs were noted to be stable. CT with contrast (Figure 3) as well as Magnetic Resonance Imaging (MRI) (Figures 4) were performed.
motorcycle collision; hematoma; Magnetic Resonance Imaging (MRI); Computed Tomography (CT)
Introduction
A 34-year-old male patient presents to the emergency department due to a progressively expanding mass on his left buttock (Figure 1). Two months prior to this visit, the patient had been injured in a motorcycle collision. Computed Tomography (CT) performed on the day of his initial injury showed a non-specific fluid infiltration over the left iliac crest, lower back, and buttock, without a large fluid collection, considered to be hematoma. (Figure 2). On his second visit, there was a firm and tender mass measuring approximately 21 x 18 cm with overlying erythema on the left buttock. The patient reported progressive enlargement of this mass over the prior months and sensitivity to light touch. Vital signs were noted to be stable. CT with contrast (Figure 3) as well as Magnetic Resonance Imaging (MRI) (Figures 4) were performed.
Images
Figure 1: MLpic1.png (Figure 1) Label: Large soft tissue mass with patient lying in right lateral decubitus position.

Figure 2: MLCTOrig CorAx.png (Figure 2) Label: Coronal and Axial CT with intravenous contrast showing hematoma (white triangles) present during original evaluation.
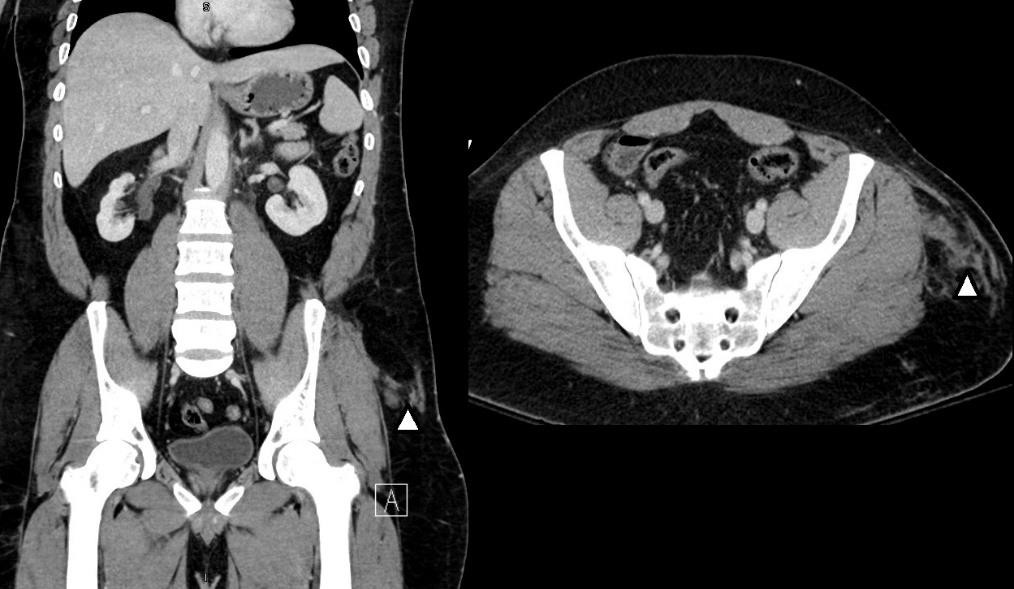
Figure 3: MLCTCorAx.png (Figure 3) Label: Coronal and Axial CT with intravenous contrast showing large fluid collection (white triangles)

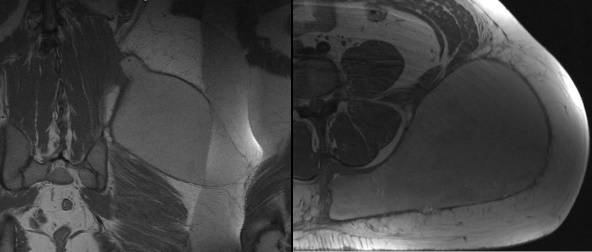
Figure 4: MLT1AxCor.png (Figure 4) Label: Coronal and Axial T1 weighted MRI of the mass showing large multi-septated complex fluid collection with increased signal intensity consistent with hemorrhagic or lymph fluid surrounded by a thick wall.
Diagnosis
Morel-Lavallée Lesion. This patient had a large fluid collection in the subcutaneous tissue of the left pelvis posteriorly on computed tomography and magnetic resonance imaging, suspicious for a Morel-Lavallée lesion. Morel-Lavallée lesions are closed degloving injures that are seen in polytrauma and high energy trauma mechanisms.
While Morel-Lavallée lesions are most commonly located in the lateral thigh, they can occur in other locations such as the buttocks, lower leg, lower back, abdominal wall, and upper extremity1. Diagnosis can be complicated; magnetic resonance imaging is superior to computed tomography1,2,3,4 as findings on CT may be non- specific. Presentation may be delayed for months to years post injury1.
Possible complications of Morel-Lavallée lesions include superinfection or skin necrosis.2,3 Management options include conservative therapy, aspiration, sclerodesis, minimally invasive surgery or open surgery. 2,3 In this case, open surgery was performed with 1250 ml of clear brown fluid evacuated from the cavity with appearance of fat necrosis. Cultures obtained were negative. Two JP drains were put and left in place, and the patient was discharged home two days after the presentation.