Case Reports International Journal
OPEN ACCESS | Volume 3 - Issue 1 - 2025
ISSN No: 3065-6710 | Journal DOI: 10.61148/ 3065-6710/CRIJ
Qu Mingzhu, Nie Pin, Dang Yanli, Liu Rumei, Zhu Kaiguo, Chen Baoying*
Xi'an International Medical Center Hospital.
*Corresponding author: Chen Baoying, Xi'an International Medical Center Hospital.
Received Date: January 24, 2025
Accepted Date: March 28, 2025
Published Date: April 10, 2025
Citation: Mingzhu Q, Pin N, Yanli D, Rumei L, Kaiguo Z, Baoying C. (2025) “A Case Report of Tubular Carcinoma of the Breast.” Case Reports International Journal, 3(1); DOI: 10.61148/CRIJ/008.
Copyright: © 2025 Chen Baoying. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
In women, breast cancer is one of the most widespread malignancies, with a fatality rate second to that of lung cancer. Tubular carcinoma of the breast (TC) is a well-differentiated invasive ductal carcinoma, characterised by orderly tubular formation. Carnil and Ranvier first described this disease in 1869[ ]. TC is typically detected through screening mammograms, so it is normally tiny and untouchable[ ]. However, with the improvement of imaging diagnosis levels in current years, the detection rate of ductal carcinoma of the breast has improved considerably.
breast cancer; lung cancer; TC; ductal carcinoma
Introduction
In women, breast cancer is one of the most widespread malignancies, with a fatality rate second to that of lung cancer. Tubular carcinoma of the breast (TC) is a well-differentiated invasive ductal carcinoma, characterised by orderly tubular formation. Carnil and Ranvier first described this disease in 1869[[i]]. TC is typically detected through screening mammograms, so it is normally tiny and untouchable[[ii]]. However, with the improvement of imaging diagnosis levels in current years, the detection rate of ductal carcinoma of the breast has improved considerably.
1. Materials and Methods
1.1 General information
A 52-year-old woman complained that calcifications of her breasts were found a month ago, during a physical examination.
1.2 Physical examination
Bilateral breasts were symmetrical, with no nipple discharge, nipple depression, or alterations in thickening of the skin.
1.3 Image examination
1.3.1Ultrasound:
At the position of 11 o'clock in the left breast, approximately 45mm from the nipple, a range of flaky low echo of about 18mm×10mm×14mm could be seen. It had an irregular shape, blurred edges, distorted structure of surrounding glands, strong punctate echo inside, slight attenuation of the rear echo, and the direction was parallel to the skin. CDFI revealed: peripheral discernible spots and striped blood flow signals. Elasticity score: 5 points.
1.3.2 X-ray:
A high-density mass shadow was observed in the upper quadrant outside the left breast, the boundary was indistinct, the size was about 33×30mm, and clustered dotted calcification shadow could be seen in it. In addition, multiple punctate calcifications could be observed in the breasts.
1.3.3 Magnetic resonance imaging (MRI):
At approximately 10 o'clock in the upper quadrant of the left breast, about 42mm from the nipple, a focal non-mass-like enhancement shadow with a disordered internal structure and with a range of about 14×12 mm could be observed. The dynamic enhancement time signal curve was flat, DWI is somewhat higher, and the ADC value is approximately 0.000906 mm²/s.
In the upper left quadrant of the breast at about 10 o'clock, the structural disorder is not mass-like enhancement. Bearing in mind the possibility of adenopathy and hyperplastic nodules, intraductal carcinoma (BI-RADS 4) ought to be excluded.
1.4 Magnetic resonance guided puncture biopsy:
The patient took a prone position, and the left breast was disinfected and fixed. Subsequent to an intravenous injection of contrasting agent, the lesion revealed a focal non-mass-like enhancement, and the glandular structure at this location was imprecise. A small incision was made after a local disinfection, and a coaxial positioning needle was inserted from the inner side of the left breast. Then a 10G rotary cutting needle was inserted, and tissues removed from various angles. These tissues were fixed with formalin. The patient felt no discomfort because the puncture process was smooth.
1.5 Pathological results:
Scattered catheter structures were discovered in the sclerotic fibrous stroma on the left side, and the immunophenotype suggested that myoepithelium was not present, which supported tubular carcinoma (WHO Ⅰ); ER (100%, medium); PR(-); AR (50%, weak); E-cadherin(+); HER-2(1+, negative); Ki-67(1%).
2. Discussion
According to the 2019 WHO Classification of Breast Tumors, ductal carcinoma of the breast is classified as a non-special form of invasive breast cancer, and tubular carcinoma with a shape more than 90% would be diagnosed. People have also started to realise that tubular cancer has a better prognosis than well-differentiated (grade 1) non-specific invasive breast cancer[[iii]]. Due to this good prognosis, Kader HA[[iv]]By compared simple ductal carcinoma to stage Ⅰ breast cancer, and a number of scholars discovered that the axillary lymph node involvement of simple ductal carcinoma was less than that of stage Ⅰ invasive ductal carcinoma, and the lymph node metastasis rate and local/systemic incidence rate were inferior to those of stage Ⅰ invasive ductal carcinoma. Consequently, in the majority of cases can omit systemic adjuvant therapy and axillary therapy can be omitted. This makes it crucial to distinguish tubular carcinoma from other diseases.
The rate of detection for breast ductal carcinoma by X-ray photography is approximately 9%-19%. The characteristic manifestation is an asymmetrical mass with burr or blurred edges. In addition, it can manifest as a mass with microcalcification, distorted structure and local asymmetry[[v]].Presently, there are a dearth of literature about usual MRI findings of ductal carcinoma of breast and MRI findings of this patient's breast (Figure 1). This patient underwent a magnetic resonance biopsy to precisely puncture the lesion and acquire the case results, thus providing a foundation for the patient's treatment.
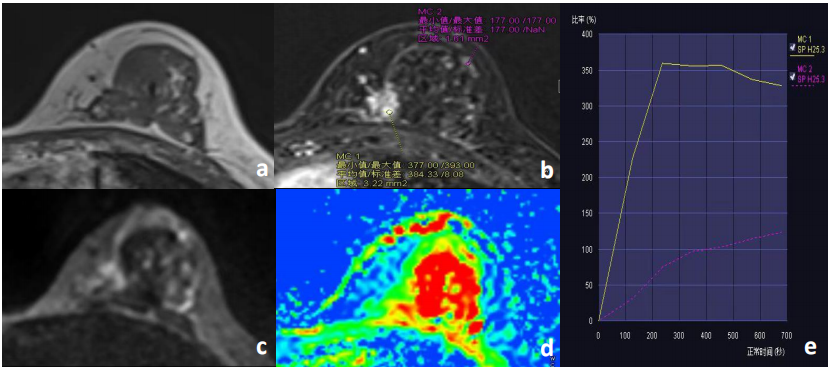
Figure 1: The patient is a 52-year-old female, who was pathologically confirmed to have tubular carcinoma of the left breast at approximately 10 o'clock. Figure A reveals that the lesions of MR T1WI reveal isointensity, the lesions of the contrast-enhanced scan reveal mass-like enhancement, with a disordered internal structure and uneven signal (Figure B). The dynamic contrast-enhanced time signal curve is flat (Figure E), the lesions reveal a slightly higher signal on DWI (Figure C), and the ADC is somewhat decreased.
Fund: Shaanxi key research and development project-general project-social development field (2020SF-049); Xi'an Science and Technology Plan Project (20YXYJ0010 (5).