Oncology and Cancer Screening
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2994-8746 | Journal DOI: 10.61148/2994-8746/JOCS
Mounir Hmidi*, Hamza Belatik Karim Nadour, Ali Elboukhari
Department of Otorhinolaryngology-Head and Neck Surgery, Military Hospital Meknes, Morocco.
*Corresponding author: Mounir Hmidi, Department of Otorhinolaryngology-Head and Neck Surgery, Military Hospital Meknes, Morocco.
Received: November 16, 2021
Accepted: November 25, 2021
Published: December 06, 2021
Citation: Mounir Hmidi, Hamza Belatik Karim Nadour and Ali Elboukhari. (2021) “Bilateral Ethmoidal Meningoencephalocele”, J Oncology and Cancer Screening, 3(4); DOI: http;//doi.org/011.2021/1.1047.
Copyright: © 2021 Mounir Hmidi. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Transethmoidal meningoencephaloceles are rare entities with congenital, traumatic, or spontaneous origins [1, 2]. Bilateral ethmoidal meningoencephaloceles are even more rare and only a very few case reports have been published [3].
Clinical Image Description:
Transethmoidal meningoencephaloceles are rare entities with congenital, traumatic, or spontaneous origins [1, 2]. Bilateral ethmoidal meningoencephaloceles are even more rare and only a very few case reports have been published [3].
Here we present an unusual case of a 56-year-old female who was presented to Department of Otorhinolaryngology-Head and Neck Surgery, Military Hospital with bilateral ethmoidal meningoencephalocele.
A 56-year-old female was referred a two years’ history of frequent and intense headaches with bilateral nasal obstruction, recurrent postnasal drip and he experienced before consulting with us, a gradually anosmia and intermittent watery rhinorrhea that worsens when he coughs, sneezes and defecate. During the last 2 years, he consulted with several ENT which diagnosed rhinosinusitis that they prescribed antibiotics, decongestants, antialergics, topical and systemic steroids. One of them diagnosed left obstructive polyposis with concomitant middle skull base defect.
Left nasal endoscopy examination revealed an obstructive pulsatile giant mass with “polypoid” aspect that was occupying the superior, inferior and posterior portion of the left nasal cavity. The inferior portion of this mass was surrounded of scarce quantity of clear and non-viscous fluid. (Figures 1). The left middle turbinate was lateralized for expansible effect of the mass. the appearance is less evocative in right.
Computed tomography (CT) of the sinuses showed two osseous defects in the anterior skull base involving the ethmoid bone, associated with a lobular soft-tissue mass extending from brain to both nasal fossae. (figure 2)
Magnetic resonance image (MRI) image showed a hyperintense cystic lesion containing brain tissu that extends from the subarachnoid space to the nasal fossa, predominant in the left side. (figure 3).

Figures 1: Nasal endoscopy examination revealed an obstructive pulsatile giant mass with “polypoid” aspect that was occupying the superior, inferior and posterior portion of the left nasal cavity. The inferior portion of this mass was surrounded of scarce quantity of clear and non-viscous fluid. (Figures 1). The left middle turbinate was lateralized for expansible effect of the mass.
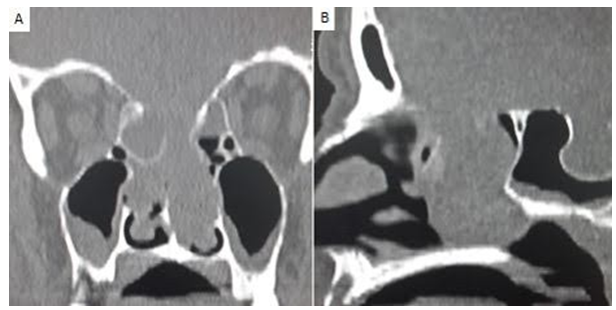
Figure 2: (a) Coronal multidetector CT image, (b) Sagittal multidetector MPR CT image: shows two osseous defects in the anterior skull base involving the ethmoid bone, associated with a lobular soft-tissue mass extending from brain to both nasal fossae.
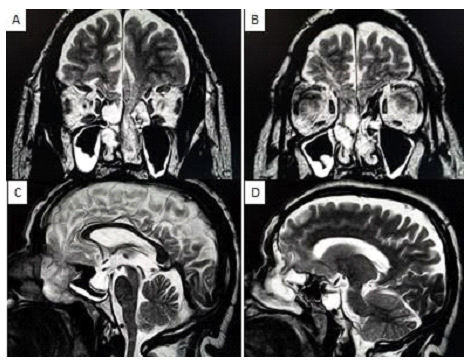
Figure 3: (A, B) Coronal T2-weighted fast spin-echo MR image; (C, D) sagittal T2-WI: shows a hyperintense cystic lesion containing brain tissu that extends from the subarachnoid space to the nasal fossa, predominant inthe left side.