Oncology and Cancer Screening
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2994-8746 | Journal DOI: 10.61148/2994-8746/JOCS
Anubha Bajaji
Histopathologist in A.B. Diagnostics, New Delhi, India.
*Corresponding Author: Anubha Bajaji, Histopathologist in A.B. Diagnostics, New Delhi, India.
Received: November 10, 2021
Accepted: November 17, 2021
Published: November 25, 2021
Citation: Anubha Bajaji. (2021) “The Susceptive Proliferation -Irritation Fibroma”, J Oncology and Cancer Screening, 3(4); DOI: http;//doi.org/011.2021/1.1046.
Copyright: © 2021 Anubha Bajaji. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Benign fibromatous neoplasms are composed of dense, collagen-rich, fibrous connective tissue. Oral fibroma is a benign neoplasm of fibroblastic origin frequently discerned within the oral cavity. Fibroma represents as a reactive hyperplasia of fibrous connective tissue engendered due to localized irritation or trauma
Preface:
Benign fibromatous neoplasms are composed of dense, collagen-rich, fibrous connective tissue. Oral fibroma is a benign neoplasm of fibroblastic origin frequently discerned within the oral cavity. Fibroma represents as a reactive hyperplasia of fibrous connective tissue engendered due to localized irritation or trauma.
Fibroma emerges as a nodular mass comprised of fibrous connective tissue with superimposed hyperplastic, hyperkeratotic stratified squamous epithelium. The benign, miniature fibrous connective tissue neoplasm usually demonstrates a magnitude below < 1.5 centimetre. Fibroma is frequently discerned within diverse sites of oral cavity as the buccal mucosa or hard palate, although no organ of neoplastic emergence is exempt.
Fibroma is additionally designated as focal fibrous hyperplasia, peripheral fibroma, peripheral ossifying fibroma, fibroid epulis or fibro-epithelial polyp.
Disease Characteristics:
Majority of oral fibromas manifest as reactive fibrous tissue hyperplasia emerging due to localized irritation or mucosal trauma [1,2].
Calculi, foreign bodies, iatrogenic factors as overhanging dental margins, deep bite, occlusal dental trauma and chronic, persistent denture or dental restorations may contribute to trauma or function as an irritant [1,2].
Traumatic fibroma frequently represents as an oral excrescence confined to the oral cavity and constitutes an estimated 4.5% of oral mucosal lesions. Mucosal sites as the anterior palate may be incriminated [1,2].
Oral fibroma exhibits a female preponderance with a female to male proportion of 2:1. Generally, middle aged females between 30 years to 60 years are incriminated [1,2].
Irritation fibroma arises due to site-specific soft tissue or mucosal irritation and localized proliferation of oral mucosal fibrous tissue is commonly discerned. Irritation fibroma demonstrates a precise configuration of collagen contingent to site of lesion and degree of mucosal irritation [2,3].
Engendered collagen exhibits specific articulations as
Irritation fibroma may occur due to plaque microorganisms or localized irritants and demonstrates a clinical countenance identical to pyogenic granuloma, peripheral giant cell granuloma or peripheral ossifying fibroma [3,4].
It is posited that traumatic fibroma is engendered due to mucosal trauma or irritation wherein lesions appear at mucosal sites predisposed to chronic, repetitive irritation and trauma [3,4].
However, the initially discerned, miniature oral fibroma with perpetual irritation or denture induced trauma may gradually progress to enlarged lesions [3,4].
Multiple oral fibromas appear as a feature of Cowden’s disease [3,4].
Clinical Elucidation:
Generally, fibroma emerges as a solitary, asymptomatic, benign, firm to hard, well circumscribed, sessile or pedunculated lesion [5,6].
Typically, oral fibroma emerges as a miniature, painless, gradually progressive lesion of approximately 2-centimetre diameter. Mastication and speech may or may not be hindered [5,6].
The neoplasm may appear as an enlarged, soft to firm, non-tender, pedunculated lesion with a smooth extraneous surface and a magnitude of around ~ 1.5 centimetres adherent to intraoral mucosa [5,6].
Commonly, lesions are discerned upon the gingiva, tongue or buccal mucosa whereas lesions upon anterior or posterior surface of hard palate are infrequent due to minimal trauma or irritation [5,6].
Histological Elucidation:
Upon gross examination, a well circumscribed, firm to hard, sessile or pedunculated oral outgrowth with a smooth surface, magnitude <1.5 centimetres and an unremarkable superficial mucosal surface is delineated. The firm to hard, pedunculated tumefaction may be adherent to incriminated site of oral mucosa [5,6].
Upon microscopy, pathognomonic fibrous stroma is intermingled with collagen bundles and prominent vascular articulations. Superimposed stratified squamous epithelium appears benign, attenuated or hyperkeratotic and may delineate focal ulceration [5,6].
Usually, a nodular mass comprised of fibrous connective tissue is superimposed by focally hyperplastic and hyperkeratotic stratified squamous epithelium. Subjacent stromal connective tissue is imbued with numerous miniature vascular articulations and mild, focal chronic inflammation [5,6].
Ortho-keratinization of superimposed stratified squamous epithelium with shortened rete pegs may be enunciated. Circumscribing connective tissue stroma is constituted of abundant collagen fibres and proliferating fibroblasts admixed with chronic inflammatory cells as lymphocytes and macrophages along with several vascular articulations [5,6].

Figure 1: Irritation fibroma exhibiting a hard, sessile, well circumscribed fibrous tissue lesion with an unremarkable superimposed stratified squamous epithelium [9].
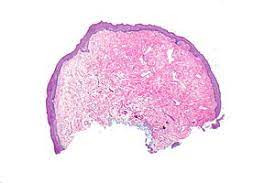
Figure 2: Irritation fibroma exemplifying collagen fibres admixed with proliferating fibroblasts, abundant vascular articulations and chronic inflammatory cells with a superimposed unremarkable epidermis [10].
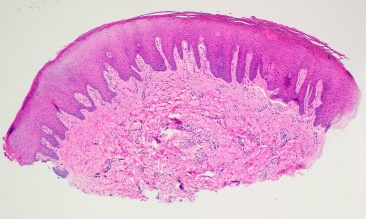
Figure 3: Irritation fibroma enunciating a hyperkeratotic stratified squamous epithelium overlying collagen fibre commingled with fibrous tissue and several vascular configurations [11].

Figure 4: Irritation fibroma delineating an acanthotic, hyperkeratotic squamous epithelium with a subjacent fibrous tissue stroma intermingled with collagen fibres, chronic inflammatory cells and congested blood vessels [12].
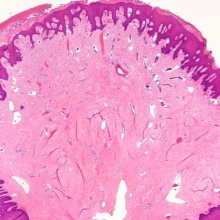
Figure 5: Irritation fibroma demonstrating an attenuated stratified squamous epithelium with an underlying fibrotic stroma intermixed with collagenous tissue and chronic inflammatory cells with patent vessels [13].
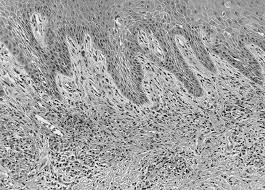
Figure 6: Irritation fibroma depicting a papillomatous stratified squamous epithelial layer with subjacent chronic inflammation admixed within collagen fibres and proliferating fibroblasts [14].
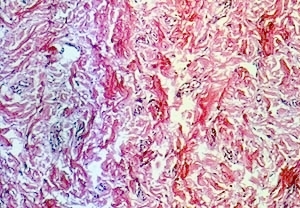
Figure 7: Irritation fibroma delineating randomly dispersed collagen fibres intermingled with fibroblastic tissue proliferation and congested blood vessels [15].
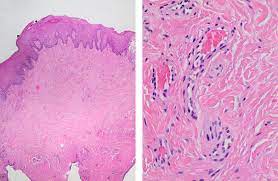
Figure 8: Irritation fibroma enunciating fibroblastic proliferation, collagen fibres, chronic inflammatory cells and congested vascular arrangements with a superimposed stratified squamous epithelium [16].
Differential Diagnosis:
Traumatic or irritation fibroma requires a segregation from lesions of giant cell granuloma, fibrous papule, pyogenic granuloma, neurofibroma, squamous papilloma, palatal fibroma, torus palatinus, dermoid cyst, ameloblastoma, oral lipoma or a benign salivary gland neoplasm [7,8].
Investigative Assay:
A competent and thorough oral examination is essential to discern the irritant or aetiological factor such as trauma arising from palatal occlusion of lower incisors. An occlusal radiograph may be obtained to exclude focal calcification [7,8]
herapeutic Options:
Supra-gingival scaling and mouth rinse with chlorhexidine is beneficial [7,8].
Traditionally, oral fibroma necessitates a comprehensive surgical extermination. Although traumatic fibroma exceptionally reoccurs, constant irritation or persistence of aetiological factor may engender a repetitive lesion [7,8].
Irritation fibroma can be appropriately treated with elimination of contributory factors or identifiable irritants and scaling of adjacent teeth. Comprehensive, aggressive surgical eradication of the lesion can be adopted in order to minimize lesion reoccurrence [7,8].
Extended postoperative monitoring is necessitated for assessing the growth potential of inadequately resected lesions which appears at an estimated ~20%. Nevertheless, lesion reoccurrence may be exceptional and induced by repetitive, site- specific trauma [7,8].
Correction of associated traumatic aetiology or oral mucosal irritation is necessitated in order to ensure lesion alleviation and circumvent lesion reoccurrence. Lesion reappearance may arise due to persistence of irritant or inadequate surgical extermination. Malignant metamorphosis of oral irritation fibroma remains undocumented [7,8].