Oncology and Cancer Screening
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2994-8746 | Journal DOI: 10.61148/2994-8746/JOCS
Luna Acharya1*, Danish Murab Ur Rehman Safi2, Maimoona Khan3, Prajwal Dhakal4, Oana Paun5
1Department of Internal Medicine, Division of General Internal Medicine, University of Iowa, Iowa City, Iowa, USA.
2Department of Hematology Oncology, Ruby Memorial Hospital West Virginia university, Morgantown, West Virginia , USA.
3Department of Medicine, Shifa College of Medicine, Islamabad, Pakistan.
4Department of Hematology Oncology, University of Nebraska Medical Center, Omaha, Nebraska, USA.
5Department of Internal Medicine, Section of Hematology, University of Iowa, Iowa City, Iowa, USA
*Corresponding Author: Luna Acharya, Department of Internal Medicine, Division of General Internal Medicine, University of Iowa, Iowa City, Iowa, USA.
Received: May 07, 2021
Accepted: May 11, 2021
Published: May 14, 2021
Citation: Acharya.L, D.Murab Ur R.Safi, Maimoona Khan, P.Dhakal, Oana.P. (2021) “Testicular Myeloid Sarcoma: A Rare Presentation of Acute Myeloid Leukemia”, J Oncology and Cancer Screening, 2(4); DOI: http;//doi.org/05.2021/1.1026.
Copyright: © 2021 Luna Acharya. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Myeloid sarcoma commonly involves the head and neck regions and lymph nodes, whereas involvement of testis and ovary are rare occurrences. The diagnosis is challenging due to often non-specific findings. Here we present a rare case of pathology-confirmed testicular myeloid sarcoma presented with recent left testicular swelling without bone marrow involvement.
1. Introduction:
Myeloid sarcoma, also known as granulocytic sarcoma, chloroma and chloroleukemia, is defined by prominent extramedullary sites of leukemia, most commonly related to either cutaneous or nodal infiltration by leukemic cells, but any organ can be involved. It is a rare condition, most often associated with acute myeloid leukemia (AML) and blastic transformation of chronic myeloproliferative disorders. Here we present a case of a testicular myeloid sarcoma with no involvement of bone marrow.
2. Case Report:
A 28-year-old male with no significant past medical history presented with left testicular swelling for two days. Initial blood work, including complete blood count with differential, was unremarkable. Testicular ultrasound showed a 3.5 x 1.7 x 2.5 cm solid-appearing lesion within the left medial testicle demonstrating internal vascularity. CT of chest, abdomen and pelvis revealed no metastatic disease. The patient underwent left radical inguinal orchiectomy. Pathology showed a 5.5 x 4 x 3.5 cm myeloid sarcoma with immunohistochemistry (IHC) staining positive for CD33, 34, 45, 68 and 163 (Figure 1). PET scan did showed no hypermetabolic sites. A bone marrow biopsy showed normocellular bone marrow with normal trilineage hematopoiesis and noblasts.
Because there was no evidence of bone marrow involvement, the patient was started on HiDAC (high dose ara-C [cytarabine]) chemotherapy. He was closely followed with a total of three cycles of HiDAC chemotherapy and to date has no recurrence of cancer. He is still alive after 12 months of initial diagnosis.
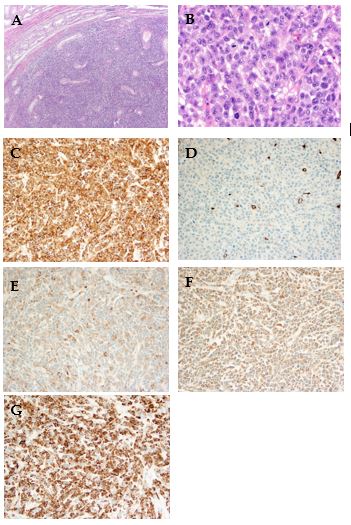
Figure 1: A) 2x magnification of orchiectomy specimen showing myeloid sarcoma. B) 50x magnification of orchiectomy specimen showing myeloid cells. C) Left testicular pathology specimen positive for CD33. D) Left testicular pathology specimen positive for CD34. E) Left testicular pathology specimen positive for CD45. F) Left testicular pathology specimen positive for CD68. G) Left testicular pathology specimen positive for CD163
3. Discussion:
Hematologic malignancies rarely manifest with involvement of tissues or organs, i.e., extramedullary involvement. The diagnosis is challenging due to non-specific findings, associated infertility and difficulty of obtaining specimens for tissue diagnosis [1]. Myeloid sarcoma develops as myeloid disorders usually after allogenic hematopoietic stem cell transplant, expressing high myeloperoxidase expression. It can involve lymph nodes, bone, skin and soft tissue, gastrointestinal tract, peritoneum, ovary, testes, and other organs [2]. Myeloid sarcoma is an neoplasm of monocytes—immature granulocytes with extramedullary involvement. In the literature, most cases of myeloid sarcoma with testis involvement represent a relapse but are occasionally diagnosed at initial presentation [3]. AML presents in less than 1% of patients with prominent extramedullary disease [4]. These patients may present simultaneously with or preceding bone marrow disease or may be seen at AML relapse. When found in association with bone marrow involvement, AML occurs most commonly as either cutaneous or gingival infiltration by leukemic cells and is most often seen when there is a prominent monocytic component to the leukemia (e.g., in acute monocytic or monoblastic leukemia or in acute myelomonocytic leukemia).
Sites of isolated myeloid sarcoma include bone, periosteum, soft tissues, and lymph nodes, and less commonly the orbit, intestine, mediastinum, epidural region, uterus, and ovary [5,11]. The initial presentation of AML with involvement of the testicles, as described in our case, is uncommon and has a poor prognosis [3,12].
Due to the similarities of findings between myeloid sarcoma and high-grade lymphomas, immunohistochemical analysis of the expression of myeloid antigens (MPO, CD68 and/or lysozyme) of undifferentiated neoplasms and high-grade non-Hodgkin lymphomas is an important tool for ruling out myeloid sarcoma. CD68 is the most commonly expressed marker of myeloid differentiation [13,14].
There are diverging viewpoints regarding the therapeutic management of myeloid sarcoma. Possible options include chemotherapy, hematopoietic stem cell transplantation (HSCT), radiotherapy and surgery [13,15]. Radiotherapy can be used in localized forms of the disease, with the aims of consolidating induction chemotherapy, treating lesions that persist after initial chemotherapy treatment, treating localized recurrences after HSCT, reducing large tumor masses or relieving compression symptoms [13]. Systemic chemotherapy similar to what is used to treat AML is considered to be the best strategy for treating myeloid sarcoma. The role of HSCT has not been defined, and this technique should be considered depending on patient age, comorbidities, current state of the disease and the cytogenetic and molecular characteristics of the neoplasm [11,13]. Nonetheless, optimal treatment still needs to be characterized through prospective studies [11,16]. In the curent case, only the patient’s left testicle was involved. There was no involvement of any other organ or bone marrow, thus the patient was started on consolidative HiDAC chemotherapy without induction chemotherapy.
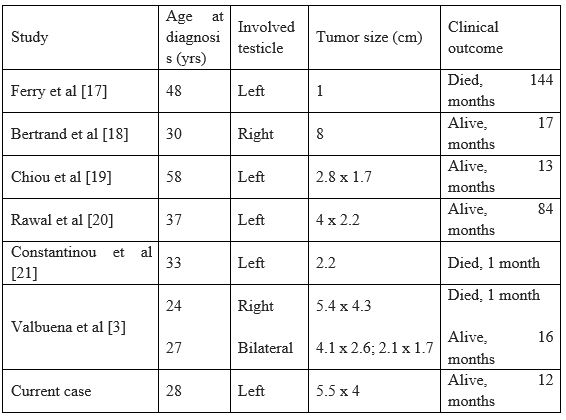
Table 1: describes case reports of testicular myeloid sarcoma.
4. Conclusion:
Despite the rarity of myeloid sarcoma, it should be taken into consideration in the differential diagnoses of undifferentiated neoplasms. The proper use of immunohistochemical techniques aid in making a diagnosis and selecting appropriate treatment.
Author Contributions:
Manuscript drafting: D.S., L.A., M.K.; critical analysis: P.D., O.P. All authors have read and agreed to the published version of the manuscript.
Funding: None
Institutional Review Board Statement: Not applicable.
Informed Consent Statement: Informed consent was obtained from the patient for the publication of this case report.
Conflicts of Interest: The authors declare no conflict of interest.