Oncology and Cancer Screening
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2994-8746 | Journal DOI: 10.61148/2994-8746/JOCS
Anubha Bajaji
Histopathologist in A.B. Diagnostics, New Delhi, India
*Corresponding Author Anubha Bajaji, Histopathologist in A.B. Diagnostics, New Delhi, India
Received: March03,2021
Accepted: March10,2021
Published: March15,2021
Citation: Bajaji A, The Luxuriant Inundation- Benign Hyperplasia Prostate. J Oncology and Cancer Screening, 2(1); DOI: http;//doi.org/03.2021/1.1005.
Copyright: © 2021 Anubha Bajaji. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Preface Benign prostatic hyperplasia is a non-malignant hyperplasia of prostatic tissue which frequently engenders specific clinical symptoms implicating the male lower urinary tract. Prostate volume and magnitude are enhanced at nearly 2% to 2.5% per annum. Clinical symptoms and morphological features are usually not concordant.
Introduction:
Preface Benign prostatic hyperplasia is a non-malignant hyperplasia of prostatic tissue which frequently engenders specific clinical symptoms implicating the male lower urinary tract. Prostate volume and magnitude are enhanced at nearly 2% to 2.5% per annum. Clinical symptoms and morphological features are usually not concordant.
Disease Characteristics An estimated 50% males exceeding 50 years demonstrate benign hyperplasia prostate with occurrence of lower urinary tract symptoms, features which augment in a linear pattern. Prevalence of benign hyperplasia prostate enhances with advancing age and appears at an estimated 50% to 60% within sixties, nearly 70% in individuals between 60 years to 69 years and around 80% to 90% within subjects exceeding > 70 years [1,2].
African Americans and Caucasians delineate a significantly elevated prostatic volume in contrast to population from southeast Asia. Nevertheless, decimated prostate volume does not concur with lower urinary tract symptoms. Additionally, mean international prostate symptom scores (IPSS) is decreased within the Caucasians [1,2].
Clinical Elucidation Nodular prostatic transitional or peri-urethral zone compresses the urethra and engenders clinical symptoms of urinary tract obstruction with acute urinary retention, urinary tract infection, hypertrophy and trabeculation of urinary bladder. Bladder diverticula may appear and usually lack concurrence with prostatic adenocarcinoma [1,2]. Benign hyperplasia prostate is associated with definitive clinical symptoms such as obstruction of bladder outlet (BOO), lower urinary tract symptoms (LUTS) and benign prostatic enlargement (BPE). Thus, instances with benign prostatic enlargement (BPE) with concurrent bladder outlet obstruction (BOO) are designated as “benign prostatic obstruction” [1,2]. Lower urinary tract symptoms (LUTS) are engendered by disorders of male urinary bladder and prostate. Lower urinary tract symptoms (LUTS) are subcategorized as “storage” symptoms such as frequency, nocturia, urgency and “voiding” symptoms as the urinary stream, straining, hesitancy and prolonged micturition [1,3]. Bladder outflow obstruction (BOO) clinically manifests as lower urinary tract symptoms (LUTS), urinary retention or urinary infections arising due to incomplete voiding [1,3]. Extensive, untreated benign prostatic hyperplasia can engender chronic, high-pressure urinary retention which is a potentially life-threatening emergency. Additionally, detrusor muscle of urinary bladder can display modifications such as over-activity and diminished contractility [3,4].Typical clinical representation necessitates evaluation of factors such as disease onset, age, duration, exacerbation and aspects which adequately relieve clinical symptoms [3,4]. Exclusion of pertinent urinary symptoms with concurrent urinary tract infections or overactive urinary bladder is required in addition to ascertainment of incriminated sites such as urinary bladder or prostate. Predominant clinical symptoms are nocturia, poor urinary stream, hesitancy or prolonged micturition. Possible occurrence of acute urinary retention enhances with increasing age [3,4]. Urinary symptoms arising due to serious conditions such as carcinoma of urinary bladder or prostate, neurological disease as cauda equina or chronic, high-pressure urinary retention terminating in renal failure mandate exclusion especially when accompanied by symptoms such as visible haematuria, bone pain, weight loss, neurological deficits, nocturnal enuresis or urinary incontinence[3,4].
Disease Pathogenesis Benign hyperplasia prostate occurs due to several factors. A direct hormonal influence of testosterone upon prostatic tissue is indicated. Testicular androgens are critical for occurrence of benign hyperplasia prostate wherein dihydrotestosterone (DHT) categorically interacts with prostatic epithelium and stroma and adheres to nuclear androgen receptors within stromal and epithelial cells with consequent activation of growth factors. Stromal cells engender 5-alpha-reductase which converts testosterone into dihydrotestosterone. Majority of total prostatic androgens (90%) configured within intact testes metamorphoses into dihydrotestosterone (DHT) under the influence of 5-alpha-reductase 2 configured within prostatic stromal cells [5,6]. Dihydrotestosterone directly impacts stromal cells situated within the prostate, induces paracrine effects within abutting prostatic cells and engenders endocrine outcomes within the bloodstream with consequent cellular proliferation and apoptosis. Benign hyperplasia prostate emerges on account of absent homeostasis between cellular proliferation and cellular demise with excessive cellular proliferation [5]. Consequently, enhanced epithelial and stromal cells accumulate between peri-urethral prostate. Additionally, oestradiol levels are enhanced within aging male subjects which elevate quantifiable androgen receptors [5,6].
Possible factors of disease emergence are subdivided into non-modifiable factors and modifiable factors. Contributors such as age, geographic location, genetic composition, metabolic syndrome, hypertension and obesity impact the occurrence of benign hyperplasia prostate [5,6].
Metabolic syndrome is constituted by hypertension, glucose intolerance, insulin resistance and dyslipidemia. Prostatic volume is significantly enhanced in metabolic syndrome and obesity. Subjects with elevated glycosylated haemoglobin (Hba1c) demonstrate elevated possible emergence of lower urinary tract symptoms (LUTS) [5,6]. Obesity is a component of metabolic syndrome, augments systemic inflammation and is associated with elevated levels of oestrogens.
Genetic predisposition is accompanied by a four-fold increase in possible occurrence of benign hyperplasia prostate in a first degree relative [5,6]. Lower urinary tract symptoms and bladder outlet obstruction occurring in benign prostate hyperplasia is contingent to static and dynamic components. Static obstruction appears as a direct consequence of prostatic enlargement with peri-urethral compression and bladder outlet obstruction. Thus, peri-urethral compression necessitates elevated voiding pressure in order to overcome resistance to urinary outflow. Also, prostatic enlargement deranges bladder outlet with ensuing obstruction to urinary outflow [5,6]. Dynamic obstruction arises due to tension of prostatic smooth muscle on account of decimated elasticity and collagen within the prostatic urethra, features which exacerbate bladder outlet obstruction. Also, loss of tissue compliance and resistance to urinary outflow are factors which contribute to disease emergence [5,6].
Histological Elucidation Benign hyperplasia prostate is accompanied by pertinent histological modifications as benign prostatic enlargement (BPE) which demonstrates enhanced magnitude of the gland following benign hyperplasia and bladder outlet obstruction (BOO) with consequent urinary outflow obstruction. Benign hyperplasia prostate characteristically demonstrates proliferation of epithelial cells and stroma which commences within transition zone of prostate circumscribing the male urethra with consequent urethral compression and bladder outflow obstruction (BOO) [1,2]. Prostatic hyperplasia is usually confined to transitional and peri-urethral zones whereas around 5% instances appear within the peripheral zone. Peri-urethral prostatic nodules are discrete, enlarged and compress encompassing prostatic tissue. Glandular hyperplasia appears as yellowish-pink soft tissue which oozes prostatic fluids whereas foci of stromal hyperplasia are firm, greyish/ white and tough in consistency. Benign hyperplasia prostate demonstrates enhanced quantification, hyperplasia and proliferation of prostatic stromal and glandular cells within the peri-urethral and transition zones [2,4].
Specifically, peri-urethral zone delineates stromal nodules and nodular glandular proliferation within the transition zone. Glandular and stromal tissue depicts hyperplasia with articulation of papillary projections, in-folding buds and cysts. Foci of squamous metaplasia and infarction are discerned [2,4]. Prostatic enlargement commences with urethral circumscription upon point of entry of ejaculatory ducts into the prostate, a region designated as transitional or peri-urethral zone. Morphological continuum with the basal zone is observed. Associated stromal alterations are enhanced quantification of smooth muscle, ductular proliferation and lymphocytic infiltration. A concurrent infectious process or prostatitis is absent. Accompanying elastic tissue may be decimated [2,4]. Microscopic variations such as sclerosing adenosis, fibroadenoma-like hyperplasia, phyllodes-like hyperplasia, leiomyoma-like nodules and fibromyxoid nodules can be encountered. Prostatic enlargement may be associated with infarction [2,4].
Prostatic hyperplasia is immune reactive to CD10[2,3].
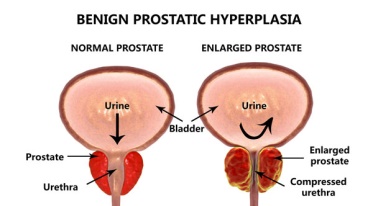
Figure 1: Benign hyperplasia prostate demonstrating urinary retention with outlet obstruction due to prostatic enlargement [9].
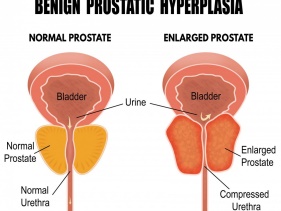
Figure 2: Benign hyperplasia prostate exhibiting prostatic enlargement with urinary outlet obstruction, hypertrophy of detrusor muscle and residual urine [10].
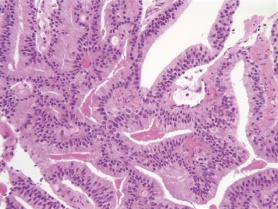
Figure 3: Benign hyperplasia prostate delineating hyperplasia of prostatic stroma along with glandular hypertrophy [11].

Figure 4: Benign hyperplasia prostate depicting concentric secretions impacted within the glandular lumen surrounded by hyperplastic glands [12].
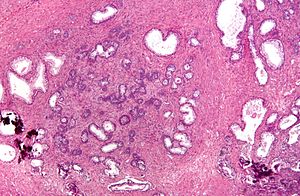
Figure 5: Benign hyperplasia prostate demonstrating muscular hypertrophy encompassing islands of hyperplastic prostatic glands [13].
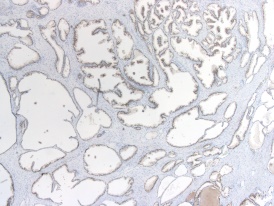
Figure 6: Benign hyperplasia prostate enunciating glandular hyperplasia surrounded by stromal hyperplasia with foci of muscular hypertrophy [14].
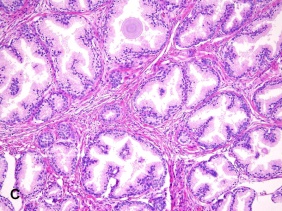
Figure 7: Benign hyperplasia prostate exemplifying significant glandular hyperplasia enmeshed within a hypertrophic and hyperplastic stroma [15].

Figure 8: Benign hyperplasia prostate exhibiting glandular hyperplasia enveloped within a muscular, stromal hyperplasia [16].
Differential Diagnosis Benign hyperplasia prostate requires a segregation from conditions such as
•carcinoma of the urinary bladder or prostate
•cauda equina with associated acute retention
•high-pressure chronic urinary retention which manifests as an insidious process or acute renal failure
•urinary tract infections[7,8)]
•sexually transmitted infections
•prostatitis
•neurogenic urinary bladder which is secondary to Parkinson's disease, multiple sclerosis and associated neurological conditions
•calculi within the urinary tract especially the urinary bladder
•urethral strictures[7,8]
Investigative Assay Comprehensive physical examination, palpation of the urinary bladder and examination of abdomen and external genitalia to exclude meatal stenosis or phimosis is required. Digital rectal examination defines the prostatic contour, consistency as smooth, hard or nodular and magnitude of the gland with pertinent, discernible lobes. However, benign hyperplasia prostate characteristically depicts a smooth, enlarged prostate [7,8]. Evaluation of urinary infection, post-void residual urine volume and international prostate symptom score (IPSS) is recommended. Assessment of urinary outflow with maintenance of urinary frequency- volume chart is beneficial [7,8]. Assessment of renal function tests, urine analysis, prostate- specific antigen (PSA), ultrasonography, urinary outflow studies, evaluation of a neurogenic bladder and cystoscopy is beneficial [7,8].
Therapeutic Options Appropriate identification of probable causes of disease progression and subjects amenable to conservative management is necessitated in order to decimate disease- associated morbidity [7,8]. Benign hyperplasia prostate can be subjected to simple observation, medical management and surgical intervention [7].
Lower urinary tract symptoms can be managed with simple observation, medical therapy or surgical intervention contingent to magnitude of disease as assessed by international prostate symptom score (IPSS).
Weight loss, fluid restriction, minimizing caffeine and circumventing constipation is beneficial [7,8)]. Medical management is achieved by specific agents such as alpha 1-adrenoreceptors such as Tamsulosin and Alfuzosin, 5 alpha-reductase inhibitors such as finasteride and dutasteride. Values of prostate specific antigen (PSA) and prostate volume are decimated.
Antimuscarinics such as solifenacin, tolterodine and oxybutynin can be employed to decrease smooth muscle tone and suppress an overactive bladder. Alternatively, β-3 adrenoreceptor agonist such as mirabegron may relax the detrusor muscle [7,8]. Combination of an alpha-blocker and alpha-reductase inhibitor is efficacious. Employment of 5-alpha reductase inhibitors reduces the prostatic volume and alpha-blockers relax prostatic smooth muscle. Alternatively, minimally invasive treatment option such as ethanol ablation can be adopted [7,8]. Surgical extermination of benign hyperplasia prostate is indicated with refractory urinary retention, recurrent urinary infection, refractory haematuria, renal insufficiency, calculi of urinary bladder, enhanced post-void residual urine and high-pressure, chronic urinary retention. Recommended surgical procedures are transurethral incision of prostate, transurethral resection of prostate, contemporary techniques as the laser vaporization and holmium laser enucleation. Open prostatectomy is principally obsolete [7,8]. Catheterization of the urinary bladder and surgical eradication with a trans-urethral prostatic resection (TURP) in order to relieve outflow obstruction is optimal. Long term catheterization is adopted to manage high-pressure urinary retention [7,8]. Intermittent self-catheterization can be employed. Following catheterization post-obstructive diuresis may ensue. Gradual decompression of the urinary bladder may be as efficacious as rapid decompression [7,8]. Deterioration of lower urinary tract symptoms or increasing difficulty in urinary voiding symptoms is an indicator of disease progression. Complications associated with benign hyperplasia prostate are acute and chronic urinary retention, urinary tract infection as a consequence to incomplete voiding, haematuria and calculi of urinary bladder [7,8]. Diverticula of urinary bladder may ensue within the residual gland following transurethral resection of prostate [7,8]. Complications may also arise on account of bladder catheterization employed to manage lower urinary tract symptoms and are designated as
•failed trial with a catheter along with an absence of catheterization
•blocked catheter, urinary retention, haematuria or urinary tract infection arising due to extensive and extended catheterization[7,8].