Oncology and Cancer Screening
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2994-8746 | Journal DOI: 10.61148/2994-8746/JOCS
Arman.Taheri 1, Hamid. Kayalha2, Hossein Majedi Ardakani3, Alireza Khajenasiri4, Asghar Karbord* 4, SaeydAli. Emami Maibodi5, Naderali Nazemian6
1Assistant Professor and pain Specialist and Faculty Member of School of Medicine of Tehran Medical Science of University. Tehran, Iran
2Associate Professor and pain Specialist student, Faculty Member of School Medicine of Qazvin Medical Science of University, Qazvin, Iran
3Assistant Professor, Department of Anesthesiology, Intensive Care & Pain Medicine, School of Medicine, Tehran University of Medical Sciences. Tehran, Iran
4Assistant Professor and pain Specialist and Faculty Member of School of Medicine of Tehran Medical Science of University. Tehran, Iran
5MSc Epidemiology & Faculty Members of Surgical Technologist Group of Paramedical College, Qazvin University of Medical Science, Qazvin, Iran
6Assistant Professor and pain Specialist and Faculty Member of School of Medicine of Tehran Medical Science of University. Tehran, Iran
*Corresponding Author: Asghar. Karbord, 4Assistant Professor and pain Specialist and Faculty Member of School of Medicine of Tehran Medical Science of University. Tehran, Iran
Received: February18,2021
Accepted: February28,2021
Published: March08,2021
Citation: Karbord A, Evaluation of the success and precision of ultrasound in intra-articular sacroiliac injection. J Oncology and Cancer Screening, 2(2); DOI: http;//doi.org/03.2021/1.1002.
Copyright: © 2021 Asghar. Karbord. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Background: The sacroiliac joint stabilizes the pelvis and transmits trunk pressure to the lower limbs. The shape of this joint and the joint surfaces are irregular and cause restrictions on movement and friction while moving. For this reason, these Caused of low back pain. However, it is difficult to place the needle accurately inside the joint space without image guidance, and improvement of ultrasound technology may lead to high success rate of intra-articular drug deposition.
Objective: Assessment of the rate of accuracy on the ultrasound guided intra-articular Sacroiliac joint injection.
Design: "Narrative Review article" Which By reviewing 50 intervention articles in this field, to determine the accuracy and precision of this therapeutic-diagnostic intervention.
Methodology: This study is a review study, in which more than 50 specialized intervention studies have been performed on the success, accuracy, extent and effect of ultrasound on intra-articular sacroiliac injection.
Results: The placement of the needle with ultrasound guidance into the sacroiliac joint was confirmed successful in 90-97 % (4000) patients by fluoroscopic arthrogram and per articular injection.
Conclusion: ultrasonography provides a high success rate of intraarticular sacroiliac joint injection as confirmed by fluoroscopy, no significant difference in clinical outcome between intraarticular and per articular injection was found.
Introduction
The sacroiliac joint is a true diarthrodial joint composed of the sacrum and bilateral iliac wings [1]. This joint stabilizes the pelvis and transmits trunk pressure to the lower limbs [2]. The anterior part of this synovial joint and the posterior part are mostly syndesmosis [3]. Numerous ligaments and muscles support this joint. Joint stability is maintained by these muscles and ligaments at rest (long standing) and in motion (running) [4]. The shape of the joint and the joint surfaces are irregular and cause restrictions on movement and friction while moving, and this causes movement restrictions for this joint. The maximum amount of movement in all three axes is 1 to 3 degrees [5]. Axial pressures such as sudden rotation cause joint damage. Intermittent rotational pressures cause joint inflammation and joint pain [6]. Damage to the joint capsule, synovial, ligaments, as well as small and large fractures, chondromalacia eventually reduces or increases joint movement [7]. Factors that contribute to sacroiliac joint damage include differences in leg length, scoliosis, pregnancy, gait disorders, motor crashes, falls, and joint fusion in the sacral lumbosacral region [8]. The sacroiliac joint is 1 to 2 mm wide and consists of S1-S2-S3, which is concave and ilium, which is convex. With age, the joint distance decreases and its shock absorber property decreases, and the joint becomes drier [9]. Sacroiliac joint pathologies account for 10 to 27% of low back pain cases. Pain in the sacrum and buttocks that shoots into back of the thigh. There is no standard diagnosis or treatment, but it can be diagnosed with the following factors. [10]. History and physical examination: With the following history, the probability of sacroiliac joint damage is higher, Falling on your hips, crashing into a vehicle while pressing your foot on the brake pedal or floor during a crash, falling into a pit or unpredictable height, a history of surgery, and fixing a lumbosacral [11]. Includes three or more positive tests: compression/approximation test, forties finger test, Patrick s test, gaenslen test, thigh thrust test, gillet test, distraction test [12]. One of the treatments is local injection of anesthetic with corticosteroids inside the sacroiliac joint [13]. Determination of the sacroiliac joint is done by various methods such as fluoroscopy or ultrasound. In both cases, the patient lies on his back and a pillow is placed under the patient's pelvis [14]. Ultrasound method uses a low frequency curved transducer that is placed transversely on the middle posterior sacrum crest. The transducer is then gently moved outward toward the sacroiliac joint to see the inner edge of the ilium [15].
Procedure:
Ultrasound evaluation and needle guidance were performed using a musculoskeletal ultrasound machine with a linear 2.5- to8.0-MHz ultrasound probe and a Terason Ultrasound Machine with the setting on a trapezoidal field of view. Fluoroscopy imaging was performed using a General Electric OEC 9900 Carm. Injections were performed by a primary and subspecialty board-certified physician with more than 10 years of practice in the use of fluoroscopic and in ultrasound-guided injections. Fluoroscopy imaging was also reviewed by a board-certified radiologist confirming successful arthrography of the SIJ. After obtaining written consent to participate in the in situational review board–approved study, the patient was placed prone on the fluoroscopy table. The area over the SIJ was sterilized, prepared, and draped in a standard surgical fashion. Each selected participant underwent unilateral ultrasound evaluation of the SIJ before completion of an ultrasound-guided needle placement into the SIJ as described in previous literature.12Once the SIJ, sacral cornu, and the posterior superior iliac spine(PSIS) were properly visualized and color Doppler was used to determine the presence of vascular structures, the planned needle entry point was marked with a sterile marker (Figs. 1A, B) A3.5- or 5-in spinal needle (depending on the soft tissue body mass the was visualized during the pre-procedural ultrasound)was inserted, in plane with the ultrasound probe, toward the SIJ. The needle was slowly advanced under ultrasound guidance, whereas the physician was anesthetizing the soft tissue with small aliquots of 1% lidocaine. Once the needle was visualized with the ultrasound to be in the SIJ space (Figs. 2A, B) [16]. It was confirmed under live fluoroscopy (Fig. 3) Then using1–2 m of contrast dye the needle's location was observed and documented) [17]. An injection was considered a success if the arthrography confirmed intra-articular contrast by the physician and radiologist. If the needle was deemed to be within the SIJ with a positive arteriogram, a solution of40 mg triamcinolone, as well as 1 ml of 1% lidocaine was injected. If the needle was not within the joint upon the injection of contrast, then the arthrogram was considered unsuccessful. The needle was repositioned under fluoroscopic guidance until a successful arthrogram had been achieved before the medication was injected. This aspect is a major difference with this study compared with other recent studies, ultrasound guidance by demonstrating that ultrasound for needle guidance is as accurate as fluoroscopy for SIJ injections.6,7Fluoroscopy has been used as a validated control in assessing accuracy of ultrasound-guided procedures in othersettings.8 However, there are several limitations with fluoroscopy that are particularly evident with repeated injections, such as two-dimensional imaging, exposure to ionizing radiation, the need for a contrast agent, and the direct and indirect costs associated with each procedure including the use of the fluoroscopy suite and the radiology technologist.9 The evidence for the diagnostic accuracy of SIJ imaging is limited and more high-quality studies are needed.10Ultrasound has become a useful tool used in many procedures performed in rehabilitation and musculoskeletal medicine because of its advantages of cost-effectiveness, lack of radiation, readiness of use, and dynamic examination.11 Ultrasound-guided SIJ injections are typically not covered by health care insurance because of their determination of a lack of evidence.6,7Ultrasound guidance has been shown to be a feasible technique for needle insertion into the SIJ using defined so no anatomic landmarks; however, more research is needed in this area for it to become a more widely accepted practice including inclusion as an acceptable imaging modality by the American Medical Association Common Procedural Terminology.
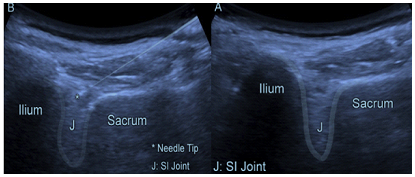
Figure 1: Ultrasound of SIJ :( A) Left SIJ with PSIS of the Ilium on the left and sacrum on the right, with the SIJ located in the open space between.
(B) Right SIJ with PSIS/ilium on the right and sacrum on the left, with the SIJ located in the open space between.
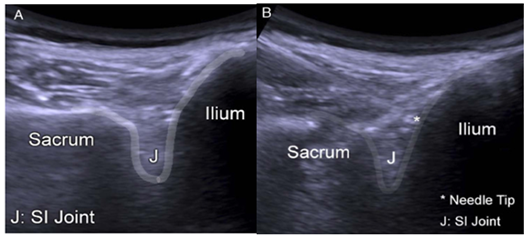
Figure 2: Ultrasound-guided SIJ injection :( A) Left SIJ with PSIS/ilium on the left and sacrum on the right, with the SIJ located in the open space between, and needle advanced into the joint.
(B) Right SIJ with PSIS/ilium on the right and sacrum on the left, with the SIJ located in the open space between, and needle advanced into the joint.
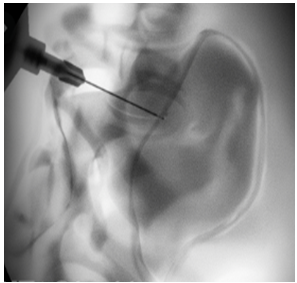
Figure 3: Fluoroscopic- guided injection of the SIJ.
Method:
In this study, the primary objective of the authors is to determine the accuracy of ultrasound technology for needle placement in the SIJ. The 4000 patients were recruited by practitioners in a multispecialty practice and included3000 females and 1000 males. Their presentations were consistent with SIJ dysfunction that was referred for SIJ intra-articular steroid injections. For each patient, a body mass index of greater than 40 was noted as morbid obesity. To be included in the study, the participant have age older than 18 yrs.’, low back or buttock Spain, three or more of five positive provocation tests: FABER/Patrick's (flexion, abduction, and external rotation), Gaenslen, thigh thrust/femoral shear test, ASIS distraction (supine), and sacral compression (side lying), and failure to respond to one or more conservative therapeutic approaches (i.e., oral medications to include muscle relaxants/anti-inflammatory agents, physical therapy, guided home exercise program).Patients were excluded from the study if they presented without positive SIJ pain on physical examination, had an allergy to contrast dye, had a contraindication to fluoroscopy, had an active injury of structures adjacent to the SIJ (i.e., lumbar spine pathology, hip pathology, piriformis syndrome), had arthropathy secondary to rheumatic causes, and had active or previous infection, bleeding, seruma or abnormal anatomy. This study conforms to all STROBE guidelines and reports the required information accordingly (see Supplemental Checklist, Supplemental Digital Content 1, http://links.lww.com/PHM/A758). Each participant was initially screened by study personnel. Those who met the inclusion/exclusion criteria were educated about these studies and provided institutional review placement for SIJ injection with confirmation by fluoroscopy. In (96%) of patients, intra-articular contrast spread was seen on fluoroscopy after ultrasound guided SIJ injection with physician and radiology confirmation of successful arthrogram. Of the 200 patients who did not demonstrate intra articular
Spread, patients had a body mass index of greater than 40. Of the 3800 joints with intra-articular spread, one was found to have vascular uptake of contrast in addition to intra-articular arthrogram on fluoroscopy. In this case, the needle was repositioned to avoid intravascular injection of anesthetic or steroid and accurate intra-articular spread was eventually seen on fluoroscopy. There were no complications reported throughout these studies with any patients at the time of the injection, on the day 1 post procedure phone interview, nor the 2- to 3-wkfollow-up history and physical examination visit.
Discussion:
In the event of SIJ dysfunction, several studies have proven the success and efficacy of intra-articular SIJ injections with fluoroscopic or CT guidance [9,10,14,16]. Ultrasound-guided SIJ injections are being conducted in some clinical settings but are not yet widely performed because it has been deemed which still injected extra-articular despite knowing that they had missed their primary target structure of the intra-articular SIJ.[14,15].Therefore, to reiterate the methods for the purposes of these studies, a negative (unsuccessful) needle guidance with ultrasound was defined as any needle movement/read just mend by the performing physician after the initial needle placement with ultrasound guidance and before the initial fluoroscopic imaging/contrast injection. The patients were immediately followed for any adverse reactions as well as post procedure relief in the recovery area. Participants were scheduled for follow-up appointment with in 2 to 3 wks. To assess for any adverse reactions and progress with relief of symptoms. Patients also received a post procedure follow-up phone call on the day after the procedure to inquire about any adverse reactions, which is standard operating procedure for our procedure suites for all injections.
Result:
In all patients, ultrasound images were adequate for identifying the necessary anatomy for needle placement. A total of 4000 patients (3000 females and1000 males) were successfully enrolled into the study and underwent ultrasound-guided needle with ultrasound confirmed with a standard imaging modality such as fluoroscopy. However, since the submission of our protocol to the institutional review board, there has been some literature on ultrasound guided versus fluoroscopy guided SIJ injections [14, 15]. Other studies differ focuses on the accuracy of needle placement with ultrasound guidance, whereas the other studies focus only on comparative efficacy between ultrasound- and fluoroscopy-guided injections. This is particularly important in comparing these studies as Soneji et all included ultrasound-guided injections in which they documented had missed the primary target of the SIJ in their results. Unfortunately, Soneji ET al [15] did not provide information on the statistics regarding how many of the test subjects in the ultrasound ground did not have an SIJ injection but instead had received a per ligament injection. Although Jee et al.14 provided retrospective information regarding the accurate placement of the needle by a radiologist after injection but still had injection of anesthetic or corticosteroid even if later found to have been intravascular. The efficacy of intra-articular versus per articular SIJ injections a controversial matter [18]. One study suggested that per articular injections are more effective because they treat the SIJ capsule and ligaments, which are thoroughly innervated [19]. Although this may provide some promising alternatives, the performance of a SIJ is still considered to be completed by accurately placing the needle into the joint and not near or around the joint or treating surrounding structures. Therefore, our study was able to demonstrate that ultrasound needle guidance can be accurately completed and demonstrate that it can be used for precise and reliable intra-articular SIJ injections.
In our study, a 96%accuracy rate was observed comparing ultrasound-guided SIJ confirmed with fluoroscopy immediately after ultrasound-guided needle placement. This is comparable with success rates reported in fluoroscopy-guided injections. In the 2000 of 4000 patients who were not intra-articular, a high body mass index of greater than 40 (morbid obesity) was noted, suggesting a higher degree of technical difficulty in obese patients. There were minimal complications and no adverse events in our study. Contrast vascular uptake was seen in one patient. There was no instance of intravascular steroid injection, because this was identified with the fluoroscopic confirmation and the needle was repositioned and new confirmation was obtained that the needle was intra-articular without being intravascular. Vascularuptake is a known complication in SIJ injections. Jee et al.14found vascularization around the SIJ in 34 of 55 patients. To our knowledge, there is limited but growing literature on the efficacy of ultrasound-guided SIJ injections [20–25] in our study, we aimed to determine the accuracy of ultrasound technology for needle placement in the SIJ. In these studies, the authors did not aim to determine the comparative effectiveness of performing SIJ injections using ultrasound versus fluoroscopic guidance, nor did we intend to compare its success rate with those of other guidance modalities such as fluoroscopy, CT, and magnetic resonance imaging. We believe that to be able to successfully compare efficacy, we needed to first establish that there was accuracy of needle placement into the SIJ time-consuming for the patient and the health care system. The author recognizes that more studies need to be performed to compare efficacy to fluoroscopic and/or CT-guided injections [26-31]; however, it is recommended that insurance companies permit the routine use of ultrasound for needle placement for the injection of the SIJ.