Oncology and Cancer Screening
OPEN ACCESS | Volume 7 - Issue 1 - 2026
ISSN No: 2994-8746 | Journal DOI: 10.61148/2994-8746/JOCS
Parham. Hourfar1, Asghar. Karbord*2, Davoud Mohammadi Nokande3, Mehran Mohebi Alidash4
1 Physician of Oxford Center for Enablement (OCE), Windmill, Headington, Oxford OX3 7HE, UK.
2 MSc Epidemiology & Faculty Members of Surgical Technologist Group of Paramedical College, Qazvin University of Medical Science, Qazvin, Iran
3 Assistant Professor, Thoracic Specialist and Faculty Member of School of Medicine of Qazvin Medical Science of University , Qazvin, Iran
4 Nursing Student of Paramedical College, young researcher ,Qazvin University Azad Medical Science, Qazvin, Iran
*Corresponding Author: Asghar. Karbord, MSc Epidemiology & Faculty Members of Surgical Technologist Group of Paramedical College, Qazvin University of Medical Science, Qazvin, Iran
*Corresponding Author: Asghar. Karbord, MSc Epidemiology & Faculty Members of Surgical Technologist Group of Paramedical College, Qazvin University of Medical Science, Qazvin, Iran
Received: February 03, 2021
Accepted: February 08, 2021
Published: February 11, 2021
Citation: Karbord A, Comparison of Accuracy and Precision of Chest X-Ray and Breast Ultrasound in the Initial Diagnosis of Breast Cancer in Young Women Under 25 Years (Gold Diagnosis: Pathology Report). J Oncology and Cancer Screening, 2(1); DOI: http;//doi.org/03.2021/1.1001.
Copyright: © 2021 Asghar. Karbord. This is an open access article distributed under the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
Introduction: Breast cancer is an unprotected growth of abnormal cells created in different breast areas. Every year, a large number of breast cancer sufferers are diagnosed, and a number of people die, breast cancer has been cited as the most common cancers in this genus in Iran, with 21.4% of women's cancers.
Aims: In order to verify the validity of ultrasound and chest x-ray breast cancer, the study was carried out as a result of pathology in breast cancer patients.
Materials and methods: This analytical epidemiological study was performed from 2011 to 2020 on 1650 young women with the first diagnosis of breast cancer who referred to the breast disease clinic in 22 districts of Tehran. Then the necessary information such as the results of history and clinical examination, chest-x-ray and ultrasound report and pathology results and other data were entered into SPSS software and analyzed by analysis of variance. The results obtained in chest-x-ray and ultrasound were compared with the results of pathology (as the gold standard).
Results: In this epidemiological analytical study, the sensitivity of chest-x-ray was 42% and its specificity was 68% and its false negative rate was 28%. The sensitivity of ultrasound was 78% and its specificity was 59% and its false negative was 16%. Also, the sensitivity of ultrasound in the diagnosis of breast cancer was significantly related to the age of patients, marital history.
Conclusion: The results of the study indicate a 58% prevalence of breast cancer in young women in Tehran. Due to the high usage and the most available methods: chest-x-ray and ultrasound, as well as the high percentage of false negatives and low sensitivity of chest-x-ray, to improve the quality of these two diagnostic methods, radiologists report these methods. More carefully with the advice of the surgeon, history and proper clinical examination, along with these diagnostic methods, be the basis for diagnosis and treatment of breast diseases.
Introduction:
Breast cancer is the non-inhibited growth of abnormal cells being developed in different areas of the breast. This can happen in different tissues, such as the ducts that transmit the milk, in milk-producing tissues, or in non-endocrine tissues. Cancer is the second cause of deaths in most advanced countries in the world, the pattern of incidence of different types of cancers varies across different populations and is associated with factors like: occupational, social, cultural and ethnic issues (possibly inheritance), geographical and cultural issues [1]. The study of breast diseases is widespread because it often catches up with women who are the main hub of families and improves their quality of life as an improvement in the quality of the community [2]. A large number of breast cancer sufferers are diagnosed each year and some die [3]. More than 211,000 American women are infected every year. The breast cancer is also seen in the men, but it is far less pronounced in the men [4]. According to a study by Globocan by the International Agency for Research on Cancer, affiliated with the World Health Organization in 2010, About 1050300 new cases of breast cancer have been observed, of which about 44.84% occurred in developing countries and its incidence is increasing in these countries. In Iran, breast cancer has been cited as the most common cancer in women, with 21.4 % of women's cancers. Similarly, in Tehran, this cancer is estimated to be the most common cancer in women (25.5% of all women cancers). which showed the nature incidence of 22.4 per 100,000 people in 1998. Another study showed the incidence of cancer in the country by 15 per 100,000 [5]. Risk factors for breast cancer include a wide range of risk factors from the molecular to the social factors that can vary between different communities, so that estimates of mortality for 1990, more than 6 times of 3/4 in China to 26.7 in northern Europe have been different or, for example, the incidence of breast cancer in the children of Japanese immigrants to Hawaii after a while is similar to that of the destination country. Since many of the risk factors of this cancer can be modified and can be altered by the intervention of interventions, it can provide information in different regions of the country to provide information based on evidence and therefore the Cost-Provide more appropriate effectiveness for each region [6].
According to the extensive results of researchers around the world, breast cancer is among the cancers that are partly inherited. That is, the defective genes transmitted from the father or mother or genes in the individual themselves cause it to emerge. Therefore, with regard to the possibility of transmission of this type of cancer between generations, there are many experiments in the world breast cancer diagnosis clinics that are performed by molecular and genetic methods and the quality of serving people for premature recognition, diagnosis of persons at risk, determining the probability of response to treatment, survival rate, etc. [7].
Chest-x-ray radiography is one of the most non-invasive methods used in the assessment of the breast, both in screening and detecting cases of disease. The predictive value of chest-x-ray varies greatly from study to study. As in previous studies, its sensitivity in cancer diagnosis has been mentioned from 33% to 98% and its specificity has been mentioned from 38% to 91% [13,18].
Another non-invasive method used in breast evaluation, especially in dense breasts, is ultrasound [11]. Ultrasound is also valuable in evaluating uncertain mammographic findings. Regarding the value of ultrasound in diagnosis of the nature of breast diseases, different results have been reported. It is noted that its sensitivity is 70 % to 90 % [14,18]. As the standard for the diagnosis and definitive nature of breast disease pathology, and this method because aggressiveness is not welcomed by patients, doctors sought to use non-invasive methods are more. However, the use of these methods requires systematic studies to determine their diagnostic value according to the current medical conditions in the country. Therefore, in this study, we have tried to evaluate the current status of chest-x-ray and ultrasound reports and their compatibility with the definitive diagnosis of breast lesion [19]. Due to the widespread use of chest-x-ray and ultrasound by the surgeon, the results of this study can be effective in screening, diagnosis and follow-up of breast cancer patients in the country because it is in fact a research based on real evidence in the country.
Materials and methods:
The present study is a cross-sectional study that was performed to investigate the epidemiology of breast cancer risk factors in Tehran from 2011 to 2020. The population under study, young women under the age of 25 years with three methods (ultrasound, chest X-ray and a biopsy of the breast) with confirmed breast lumps and breast disease clinics in Tehran were referred. Demographic information, family history of breast cancer, history of pregnancy and lactation were then entered into a questionnaire by the trainees. All patients underwent a classic examination of both breasts by a general surgeon and the examination results (based on findings such as mass profile and axilla status The basis of the surgeon's clinical judgment) was recorded as 4 groups: benign, malignant, normal and suspected. For each patient who presented with an ultrasound, chest-x-ray, or both, the imaging response was reported as normal, benign, suspected, and malignant based on the available imaging date. In some cases, if the imaging was not done, an ultrasound, chest x-ray, or both were requested based on age and breast density status. Finally, the data were entered into SPSS software version 22 and analyzed by analysis of variance.
Findings:
In this study, participants with a mean age (18.23±3.29) were the youngest 11 years old and the highest 25 years old. Most people were in the age group between 15 to 20 years (60%). The difference between the two groups in terms of age in this study is significant (001/0< P). Also, the mean weight of individuals (64±8.7) with a minimum weight of 41 and a maximum of 128 kg, most of whom (59%) were in the weight group between 60 and 80 kg. In this study, almost half of the women had university education (47%) and undergraduate education (21%) and all of them were students. 56% of women had a family history of breast cancer and 32% of women had a history of menstrual disorders, which was significantly associated with this disorder and breast cancer.
A total of 1,200 chest-x-rays and 1,450 ultrasounds from 1,650 patients who presented with breast mass complaints were reviewed and compared with the pathology report. 900 of these patients had breast cancer and 750 had benign breast diseases. In 900 patients with cancer, 770 chest-x-rays were performed prior to sampling, of which 68% were reported to be malignant and 32% of X - ray report did not match the pathology response. In 750 patients with benign breast masses, 430 chest-x-ray reports were recorded, all of which were performed prior to breast biopsy. Of the 430 chest-x-rays recorded, 70% did not match the chest-x-ray report with the pathology report. False positives and false negatives are shown in Table1. Accordingly, in this study, which is in fact an evidence-based study and review of the current situation of these two imaging methods in the country, chest-x-ray sensitivity was 42% and its specificity was 68%.
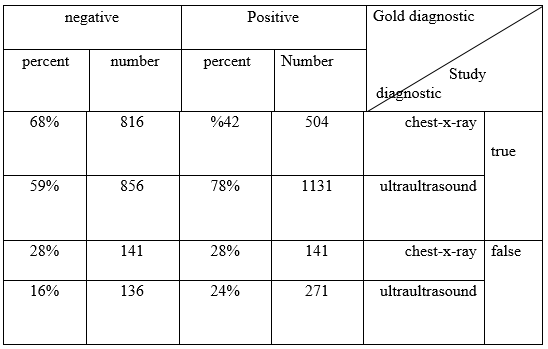
Table 1: Comparison of false and true, positive and negative chest-x-ray and ultrasound with gold diagnosis (study criterion)
Regarding the consistency of ultrasound reports with breast cancer pathology report, out of 900 patients, 850 ultrasound reports were recorded, of which 68% were ultrasound malignant and in 25% of ultrasound reports did not match the pathology response. Regarding the correlation between ultrasound reports and pathology in benign breast mass diseases, out of 83% of patients with benign breast diseases, a total of 75% of ultrasound reports were recorded, of which 47% were benign and 23% of ultrasound reports did not match the pathology response. In total, out of 1450 registered ultrasound cases, the number of positive cases was 68%, false positive 18%, true negative 28% and false negative 18%(Table 1), This study is based on evidence, the sensitivity of ultrasound is 78% and its specificity is 59%. In general, there was a significant difference between the specificity and sensitivity of these two diagnostic imaging methods (P-value =/002). The correlation between ultrasound reports and pathology results in patients with malignancy was significantly correlated with the presence or absence of marital history (P-value =/01). But this relationship was not significant in chest x-ray (P-value =/06) (Table 2). Also, the degree of conformity of ultrasound reports with pathology results was not significant in the presence or absence of marital history in patients with malignancy (In relation to chest x-ray(P=0/4)), but it was significant in relation to ultrasound
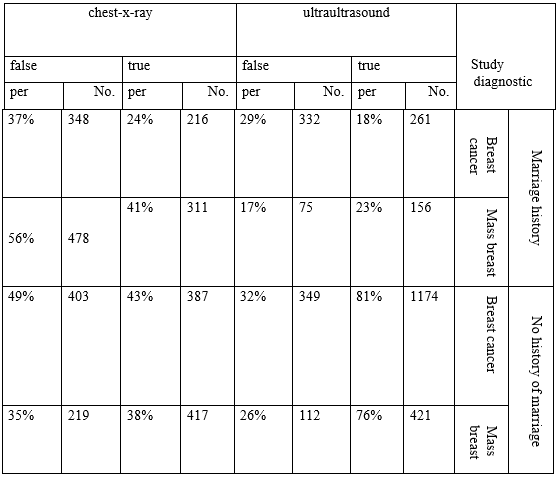
Table 2: Ultrasound and chest-x-ray results in the diagnosis of breast cancer by history of pregnancy and pregnancy
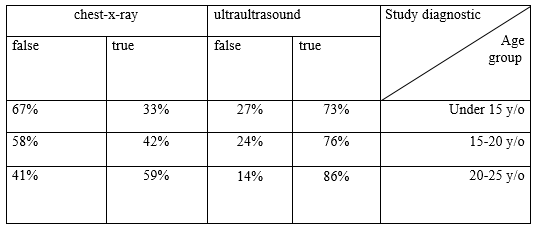
Table 3: Ultrasound and chest-x-ray results in the diagnosis of breast cancer by age of patients at diagnosis
Regarding the degree of conformity of ultrasound reports with the pathology response and its relationship with the patient's age (Table 3), patients were divided into three groups: under 15 years and 15 to 20 years and 20 and above. However, there was no significant correlation between chest ultrasound (P-value = 0.04) and chest-x-ray (P-value = 0.7) with the pathology response with age.
Discussion and conclusions:
The results of the study show that the prevalence of breast cancer in tehran in the generation of young girls is rapidly increasing due to factors such as air pollution, diet, age of socio - environmental conditions. These results are in line with the results of Niloufar Motamedi in Shiraz and Shahrbanoo Kayhanian in Ramsar [20]. In the diagnosis of this disease, increasing use of imaging methods such as chest-x-ray and ultrasound has been the first step for early detection of breast cancer and has had significant effects on increasing the biological factors of these patients [21]. However, like other para-clinical methods, chest x-ray and ultrasound, in addition to the benefits mentioned, face limitations in hardware as well as in the skill of the performer. This is especially evident in the case of ultrasound [22]. Existence of such limitations has caused different studies to determine the sensitivity and specificity of these two imaging methods, the factors affecting them and how to increase the sensitivity and specificity of these two methods and the results of different studies are significantly different. In various studies, 32% of false-positive chest-x-rays and about 39% of false-negative cases have been reported. Chest x-ray sensitivity of 71-90% has been reported [23]. In the case of ultrasound, the values related to the sensitivity and specificity of this test in the diagnosis of breast cancer is very different in different sources and research. In the Sabin Malor study in Germany in 2000, the sensitivity of ultrasound was calculated to be 89.1% [24]. In a 2009 study by Devulli et al. In Serbia, the sensitivity of ultrasound was 71.1%. The existence of different results in different studies is related to the different devices and the dependence of both methods, especially ultrasound on the person performing it, as well as clinical examinations of doctors and midwives. Our study is based on the evidence of the current situation in the country.
In our study, ultrasound false negative 18%, ultrasound sensitivity of 82% and its specificity of 68% were calculated. Given that a positive family history of breast cancer has been one of the most important factors influencing the sensitivity of chest-x-ray reporting by a radiologist, chest-x-ray cases have been reviewed by a radiologist after biopsy. Also, in our study, the presence of marriage and pregnancy significantly reduced the false negatives of ultrasound and in fact increased the power of ultrasound diagnosis, which may be due to changes in breast tissue caused by pregnancy and more attention of the doctor in examination and more accurate view of the photo. Radiology is justifiable. However, the history of marriage and pregnancy was not significantly associated with chest-x-ray sensitivity in the diagnosis of breast cancer, which is similar to the findings of other studies, including the 2004 study by Bank and Reeves [13]. Various factors can affect the accuracy of diagnostic imaging methods (chest-x-ray and ultrasound). Various factors can affect the detection accuracy of imaging methods (chest x-ray and ultrasound). Some are related to patients such as previous breast surgery history, patient's menstrual status, patient cooperation to perform imaging and follow the instructions of the technician and the accuracy of the radiologist during reporting, and some factors are related to the health system, which are: hardware ie Existence of standard device and new generation of chest-x-ray devices and use of film and processor drug suitable for the appearance of appropriate photos. Manpower means a radiologist fluent in chest-x-ray and breast ultrasound. Chest-x-ray and ultrasound performed by a radiologist and observance of scientific principles related to imaging technique to obtain standard stereotypes, non-observance of any of these factors causes the diagnostic power of imaging test to be different from the values mentioned in references and studies. According to the results of this study, which shows that the number of false-negative cases of chest-x-ray in the country is more than 4 times the world level, it is recommended to treat the patient with breast mass carefully and classically. Results of imaging methods, the surgeon's clinical judgment should be given more attention to prevent errors and delays in diagnosis.
Acknowledgments: Many thanks to all the staff at the Breast Diseases Clinic and the people who helped us with this study